1 病例资料
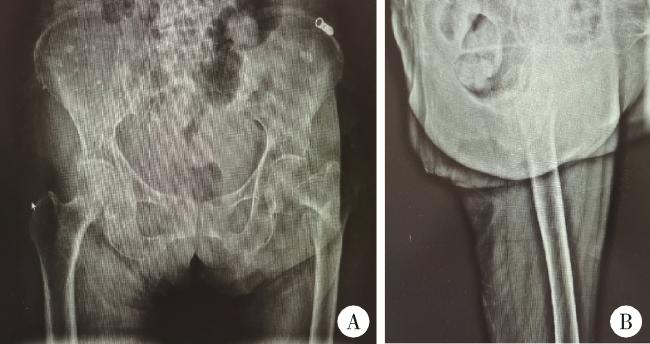
图1 患者第一次入院前髋关节X线片Figure 1 Hip joint X-ray of patient before initial admission A, radiographic examinations, including X-ray imaging of anteroposterior view of hips; B, lateral view of left hip, indicate the presence of an intertrochanteric fracture in the left femur. |
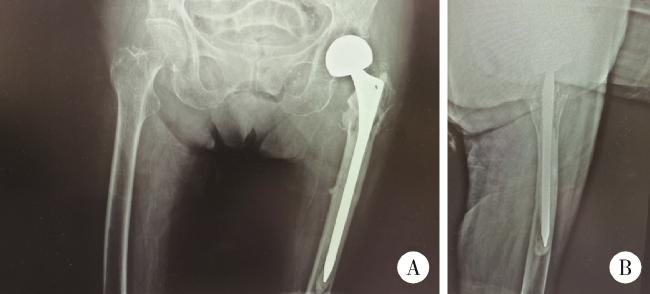
图2 患者股骨粗隆间骨折闭合复位内固定术术中透视X线片Figure 2 X-ray in closed reduction and internal fixation of femur intertrochanteric fracture of paitient A, following closed reduction, the X-ray of the left hip confirmed a well-reduced fracture; B, after inserting the guide pin into the femoral medullary cavity, reaming was performed; C, subsequently, the proximal femoral intramedullary nail and lag screw were inserted, and an X-ray of the femur was taken. |
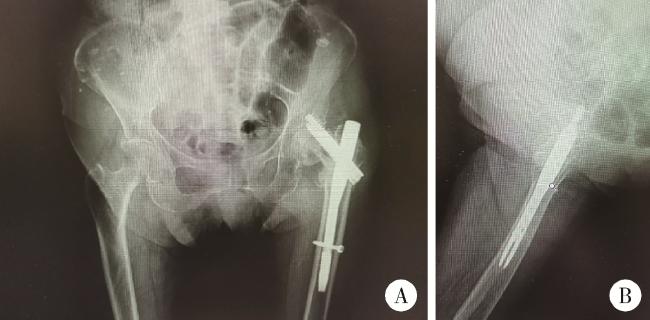
图3 患者左股骨粗隆间骨折闭合复位髓内钉内固定术后X线片Figure 3 X-ray after closed reduction and intramedullary nail fixation of left femoral intertrochanteric fracture of patient A, post-operative anteroposterior view of hips; B, lateral view of left hip, showed that the fracture reduction and internal fixation was satisfactory. |
图4 患者术后16个月髋部X线片Figure 4 Radiographic examination of the hip of patient 16 months postoperatively A, sixteen months post-operation, X-ray imaging of anteroposterior view of hips; B, lateral view of left hip, revealed a fracture in the left femoral neck and a cut-out screw. |
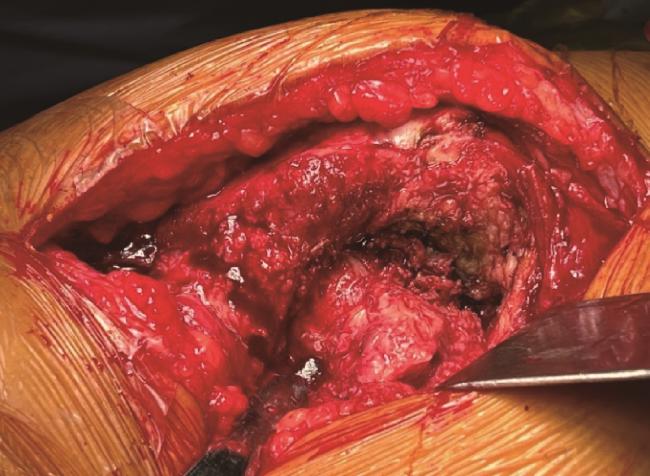
图5 术中所见,患者原股骨粗隆间骨折已愈合,新发股骨颈骨折Figure 5 During the operation, the patient' s original intertrochanteric femur fracture had healed, revealing a femoral neck fracture |