1 资料与方法
1.1 研究对象及患者一般资料
1.2 手术方法
1.2.1 关节镜探查及自体肌腱获取
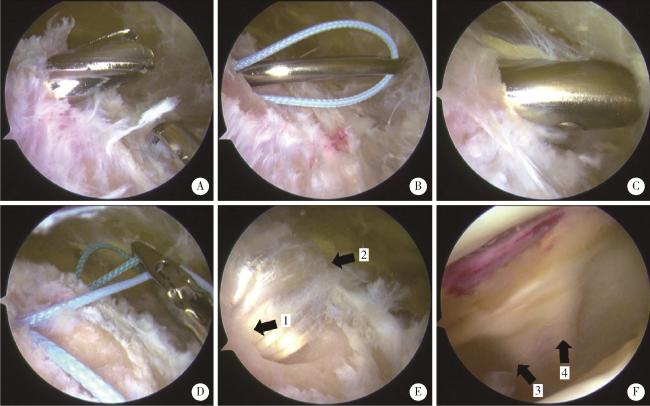
图1 关节镜下内侧髌股复合体重建Figure 1 Arthroscopically assisted medial patellofemoral complex reconstruction A, a patellar tunnel was made at the upper third point of the medial patella with a 4.5 mm drill; B, guide sutures were introduced through the patellar tunnel with an eyelet pin; C, a quadricep-tendon tunnel was created at the midpoint of the superior patella using a blunt cannula; D, guide sutures were pulled out through the medial femoral incision with a grasper; E, the autograft was introduced into the patellar tunnel (arrow 1) and the quadricep-tendon tunnel (arrow 2) with guide sutures; F, intraarticular view of the double-bundle (arrow 3 and 4) reconstructed graft. |
1.2.2 建立股骨骨道
1.2.3 建立髌骨-股直肌肌腱通道
1.2.4 移植物固定
1.3 术后康复
1.4 观察指标
1.4.1 随访及临床指标
1.4.2 影像学指标
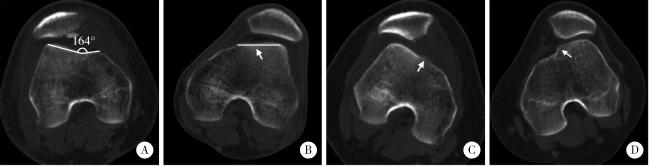
图2 基于轴位CT的Dejour分型示例Figure 2 Examples of 4-grade Dejour classification based on axial CT A, a 38-year-old male was diagnosed with Dejour A trochlear dysplasia, whose CT scan indicated a trochlear groove angle of >145 degree and symmetric trochlear facets; B, a 21-year-old male was diagnosed with Dejour B trochlear dysplasia, whose CT scan indicated a flat trochlea (arrow); C, a 16-year-old female was diagnosed with Dejour C trochlear dysplasia, whose CT scan indicated asymmetric trochlear facets and hypoplastic medial facet (arrow); D, a 17-year-old female was diagnosed with Dejour D trochlear dysplasia, whose CT scan indicated a positive cliff pattern (arrow). CT, computed tomography. |
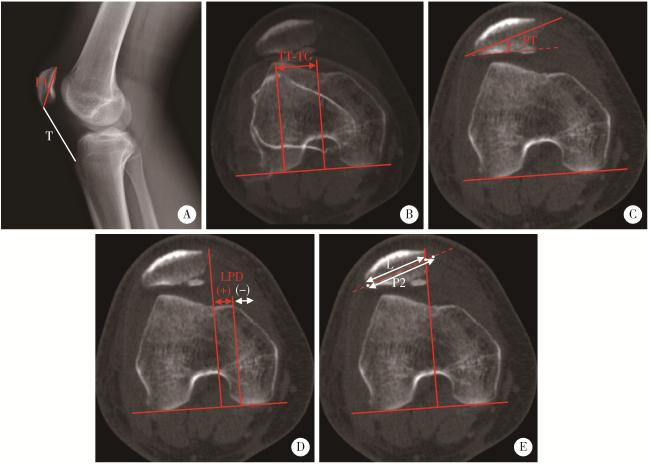
图3 侧位X线及轴位CT影像学指标的测量方法Figure 3 Measurements of radiographic parameters on lateral plain radiographs and axial CT A, Insall-Salvati index is the ratio of the patellar tendon length (T) to the patellar height (P1, distance from the superior pole to the inferior pole) on lateral plain radiographs; B, TT-TG distance is calculated by the transverse length between the trochlear groove and the tibial tuberosity on axial images; C, PT is the angle between the transverse axis of the patella and the posterior femoral condylar line; D, LPD describes the distance between the medial margin of the patella and the medial trochlear margin measured by lines perpendicular to the posterior femoral condylar line; E, bisect offset is determined by the ratio at which the patella width was bisected from its lateral aspect to the transverse width of the patella (L/P2). CT, computed tomography; LPD, lateral patellar displacement; PT, patellar tilt; TT-TG, tibial tubercle-trochlear groove. |
1.5 统计学分析
2 结果
2.1 解剖学危险因素及软骨损伤
表1 解剖学危险因素及软骨损伤Table 1 Anatomical risk factors and chondral lesion |
| Parameters | Data |
| Dejour classification | |
| Type B | 17 (37.0) |
| Type C | 20 (43.5) |
| Type D | 9 (19.6) |
| Patellar height (Insall-Salvati index) | 1.2±0.2 |
| < 1.2 | 21 (45.7) |
| ≥ 1.2 | 25 (54.3) |
| TT-TG distance | 19.6±3.5 |
| < 20 mm | 24 (52.2) |
| ≥ 20 mm | 22 (47.8) |
| Patellar tilt/(°) | 30.9±10.5 |
| Chondral lesion | |
| Patella > ICRS Ⅱ | 23 (50.0) |
| Trochlea > ICRS Ⅱ | 1 (2.2) |
| Lateral femoral condyle > ICRS Ⅱ | 8 (17.3) |
Data are presented as ${\bar x}$±s or n(%). Kappa value of four-grade Dejour classification was 0.703, indicating fair to good inter-observer agreement. For the discrepancies between the two observers, opinion of ano-ther senior doct or was sought to determine the classification. TT-TG, tibial tubercle-trochlear groove; ICRS, International Cartilage Repair Society. |
表2 Dejour B~D型间解剖学危险因素的比较Table 2 Comparison of anatomical risk factors among Dejour type B, C and D dysplasia |
| Parameters | Type B (n=17) | Type C (n=20) | Type D (n=9) | F | P |
| Insall-Salvati index | 1.1±0.2 | 1.2±0.2 | 1.3±0.1 | 2.641 | 0.083 |
| TT-TG distance/mm | 19.0±3.3 | 19.4±3.9 | 21.2±2.5 | 1.232 | 0.302 |
| Patellar tilt/(°) | 30.2±9.1 | 31.2±12.7 | 31.9±8.7 | 0.066 | 0.936 |
Data are presented as ${\bar x}$±s. TT-TG, tibial tubercle-trochlear groove. |
2.2 膝关节功能评分
表3 术前及术后膝关节功能评分对比Table 3 Comparison of patient-reported outcome measures before and after surgery |
| Outcome measures | Preoperative score | Postoperative score | Z | P |
| IKDC score | 56.3±15.1 | 86.2±8.1 | -5.896 | < 0.001 |
| Kujala score | 58.9±15.6 | 92.6±5.4 | -5.906 | < 0.001 |
| Lysholm score | 63.7±15.0 | 94.0±5.7 | -5.906 | < 0.001 |
| Tegner score | 3.1±1.4 | 4.7±1.4 | -4.867 | < 0.001 |
| Subjective satisfaction | 9.1±1.0 |
Data are presented as ${\bar x}$±s. IKDC, International Knee Documentation Committee. |
表4 Dejour B~D型间膝关节功能评分改善量比较Table 4 Comparison of improvements in patient-reported outcome measures among Dejour type B-D dysplasia |
| Outcome measures | Type B (n=17) | Type C (n=20) | Type D (n=9) | F | P |
| ΔIKDC score | 27.2±17.7 | 29.1±15.2 | 37.0±13.7 | 1.173 | 0.319 |
| ΔKujala score | 27.5±12.8 | 30.8±13.9 | 34.4±13.5 | 1.378 | 0.263 |
| ΔLysholm score | 31.6±14.8 | 32.1±14.9 | 41.0±14.6 | 0.815 | 0.449 |
| ΔTegner score | 1.4±1.5 | 1.5±1.7 | 2.2±1.4 | 0.896 | 0.416 |
Data are presented as ${\bar x}$±s. Δ refers to the improvements of patient-reported outcome measures. IKDC, International Knee Documentation Committee. |
2.3 运动恢复
2.4 并发症
表5 术后膝关节疼痛与软骨损伤程度相关性分析Table 5 Relationship between postoperative symptomatic knee pain and stages of chondral lesion |
| Chondral lesion | No lesion | ICRS Ⅰ | ICRS Ⅱ | ICRS Ⅲ | ICRS Ⅳ | P |
| Patella | 0.869 | |||||
| Symptomatic knee pain (-) | 3 | 2 | 13 | 9 | 8 | |
| Symptomatic knee pain (+) | 2 | 0 | 3 | 3 | 3 | |
| Trochlea facet | 0.287 | |||||
| Symptomatic knee pain (-) | 12 | 2 | 21 | 0 | 0 | |
| Symptomatic knee pain (+) | 5 | 0 | 5 | 1 | 0 | |
| Lateral femoral condyle | >0.995 | |||||
| Symptomatic knee pain (-) | 26 | 1 | 1 | 2 | 5 | |
| Symptomatic knee pain (+) | 10 | 0 | 0 | 0 | 1 |
Data are presented as n; ICRS, International Cartilage Repair Society. |
2.5 影像学评估
表6 术前及术后髌股关节CT参数对比Table 6 Comparison between preoperative and postoperative CT parameters of the patellofemoral joint |
| Parameters | Preoperative value | Postoperative value | Z | P |
| Patellar tilt/(°) | 30.9±10.5 | 9.8±6.0 | -5.443 | < 0.001 |
| Lateral patellar displacement/mm | 10.4±8.1 | -8.7±7.1 | -5.442 | < 0.001 |
| Bisect offset ratio | 1.1±0.3 | 0.6±0.2 | -5.442 | < 0.001 |
Data are presented as ${\bar x}$±s. Postoperative CT scans were feasible in 39 knees (84.8%). CT, computed tomography. |
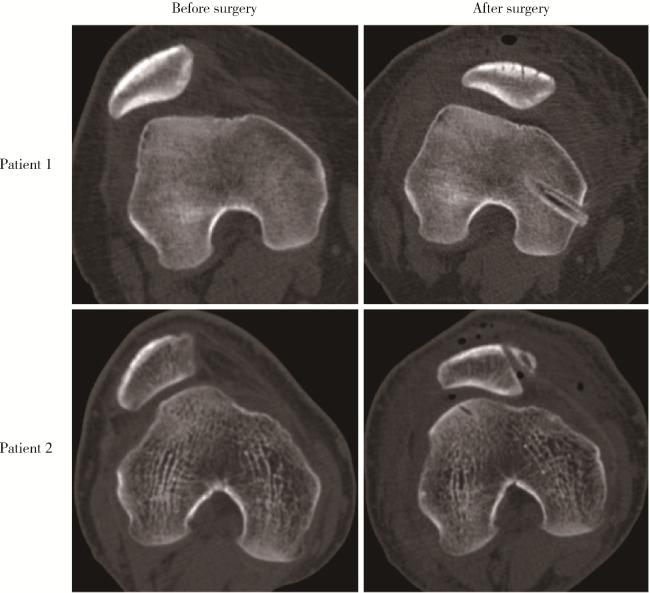
图4 内侧髌股复合体重建前后髌股关节轴位CT对比Figure 4 Comparison of axial CT scans of the patellofemoral joint before and after MPFC reconstruction Patient 1 was a 17-year-old male diagnosed with recurrent patellar dislocation of the right knee. Preoperative CT scan showed significant patellar tilt and lateral displacement, which were both corrected on postoperative scan. Patient 2 was a 16-year-old male diagnosed with recurrent patellar dislocation of the right knee. Preoperative CT scan demonstrated a dislocated patella with remarkable tilt and lateral translation, while the patellofemoral congruence was restored on postoperative scan. CT, computed tomography; MPFC, medial patellofemoral complex reconstruction. |