1 资料与方法
1.1 研究对象
1.2 治疗方法
1.2.1 数据获取及处理
1.2.2 试验组的手术设计及术中实现
1.2.3 对照组的手术设计及术中实现
1.3 术后随访
1.4 评价方法
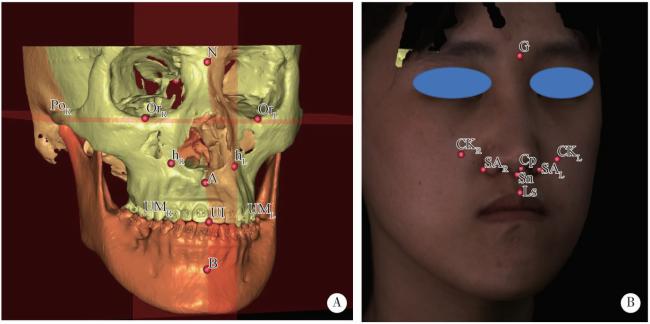
图1 三维头影测量标志点示意图Figure 1 Diagram of main landmarks in three-dimensional cephalometry A, landmarks of hard tissue; B, landmarks of soft tissue. The full names and explanations of all landmarks were listed in Table 1. |
表1 三维头影测量中解剖标志点及参考平面的定义Table 1 Definition of the three-dimensional anatomical landmarks and reference planes |
| Parameters | Abbreviation | Definition |
| Bone and dental landmarks | ||
| Sella | S | The center of the hypophyseal fossa |
| Nasion | N | The midpoint of the frontonasal suture |
| Orbitale | OrL, OrR | The most inferior point of each infraorbital rim |
| Porion | PoL, PoR | The most superior point of each external acoustic meatus |
| Subspinale | A | The point of maximum concavity in the midline of the dento-alveolar process of the maxilla |
| Upper incisor | UI | The most mesial point of the tip of the crown of the right upper central incisor |
| Upper incisor apex | UIa | The apex of the right upper central incisor |
| Upper molar | UML, UMR | The mesial buccal cusp of the first upper molar |
| Supramental | B | The point of maximum concavity in the midline of the dento-alveolar process of the mandible |
| Point h | hL, hR | Point on the left/right maxilla directly below the soft tissue alar base on axial view |
| Soft tissue landmarks | ||
| Glabella | G | The most anterior midpoint on the fronto-orbital soft tissue contour |
| Subalare | SAL, SAR | Labial insertion of each alar base |
| Cheek mass | CKL, CKR | The most anterior point on the mid-pupillary plane (MPP) under infraorbital area and ahead of cornea perpendicular plane (CPP) |
| Subnasale | Sn | The midpoint of the angle at the columella base where the lower border of the nasal septum and the surface of the upper lip meet |
| Labiale superius | Ls | Midpoint of the upper vermillion border |
| Columella peak | Cp | Most superior point of the columella |
| Cornea | CL, CR | The most anterior point of the cornea |
| Reference planes | ||
| Frankfort horizontal plane | FHP | The plane passes bilateral Orbitale and the midpoint between bilateral porion |
| Midsagittal plane | MSP | The plane perpendicular to the FHP plane and passing through sella and nasion |
| Facial plane | FP | The plane perpendicular to the FHP and MSP planes and passing through glabella |
| Occlusal plane | OP | The plane passes the midpoint between UI and the midpoint between UML and UMR |
| Mid-pupillary plane | MPP | The plane perpendicular to the FHP and FP planes and passing through cornea |
| Cornea perpendicular plane | CPP | The plane perpendicular to the FHP and MSP planes and passing through cornea |
1.5 统计学分析
2 结果
2.1 基本信息及术前三维头影测量结果对比
表2 试验组和对照组的基线特征和T0期三维头影测量值Table 2 General characteristic and preoperative 3D cephalometric values of test group and control group |
| Parameters | Test group(n=11) | Control group(n=10) | t | P value |
| Female | 9 (81.8) | 8 (80.0) | -0.101 | 0.921 |
| Age/years | 24.91±6.20 | 24.00±5.06 | 0.366 | 0.719 |
| SNA/(°) | 82.47±2.28 | 81.26±2.89 | 1.067 | 0.299 |
| SNB/(°) | 85.90±2.46 | 86.45±2.74 | -0.489 | 0.631 |
| OP-SN/(°) | 8.68±5.17 | 8.33±3.19 | 0.182 | 0.857 |
| UI-SN/(°) | 122.59±7.56 | 123.32±7.11 | 0.229 | 0.821 |
| SNhR/(°) | 72.07±2.91 | 71.50±4.30 | 0.364 | 0.720 |
| SNhL/(°) | 71.66±2.68 | 70.92±4.41 | 0.468 | 0.645 |
| CKR-FP/mm | -2.22±2.68 | -3.04±3.44 | 0.614 | 0.546 |
| CKL-FP /mm | -3.01±3.26 | -3.79±2.93 | 0.580 | 0.569 |
| SAR-FP /mm | -3.23±3.15 | -4.51±3.20 | 0.921 | 0.369 |
| SAL-FP /mm | -4.16±3.01 | -4.87±3.38 | 0.512 | 0.615 |
| NL angle/(°) | 87.61±14.62 | 84.63±12.97 | 0.491 | 0.629 |
| UI-FP/mm | 0.37±4.06 | -1.42±3.96 | 1.020 | 0.320 |
The genetic ratio is presented as n (%) and other parameters are present as $\bar x \pm s$. Compared between groups by Student-t test, α=0.05, P<0.05 is considered statistically significant. SNA, the angle formed by point S, N and A; SNB, the angle formed by point S, N and B; SN, the skull base line connecting sella and nasion; OP-SN, angle of the occlusal plane and SN line; UI-SN, angle of the axis of the right upper incisor and SN line; SNhR, angle formed by point S, N and hR; SNhL, angle formed by point S, N and hL; CKR-FP, CKL-FP, SAR-FP, SAL-FP and UI-FP means the sagittal distance between CKR, CKL, SAR, SAL, UI and the facial plane, negative values means the points are behind the facial plane and positive values means the points are in front of the facial plane; NL angle, nasolabial angle compromised of Ls, Sn and Cp. |
2.2 手术干预对比
2.3 鼻旁区软硬组织变化对比
表3 T2期试验组和对照组的三维头影测量值对比Table 3 3D cephalometric values at T2 of test group and control group |
| Parameters | Test group (n=11) | Control group (n=10) | t | P value |
| SNA/(°) | 84.29±2.66 | 84.02±2.78 | 0.225 | 0.824 |
| SNB/(°) | 82.69±1.85 | 82.84±2.73 | -0.142 | 0.889 |
| OP-SN/(°) | 10.26±4.64 | 11.62±3.92 | -0.723 | 0.479 |
| UI-SN/(°) | 112.15±5.40 | 122.38±8.83 | -3.237 | 0.004** |
| SNhR/(°) | 78.48±2.77 | 76.16±3.83 | 1.600 | 0.126 |
| SNhL/(°) | 78.44±2.55 | 75.97±4.18 | 1.657 | 0.114 |
| CKR-FP/mm | 2.78±2.92 | -1.21±3.31 | 2.932 | 0.009** |
| CKL-FP /mm | 2.33±3.20 | -1.60±3.25 | 2.793 | 0.012* |
| SAR-FP/mm | 2.03±3.17 | -1.32±2.95 | 2.507 | 0.021 |
| SAL-FP/mm | 2.23±3.73 | -1.71±2.91 | 2.682 | 0.015* |
| NL angle/(°) | 106.54±12.82 | 93.90±12.46 | 2.288 | 0.034* |
| UI-FP/mm | 0.84±4.87 | 1.79±3.89 | -0.494 | 0.627 |
All results are in normal distribution and presented as $\bar x \pm s$. Student-t test, * P<0.05,* * P<0.01. The definition of the parameters were listed under Table 2. |
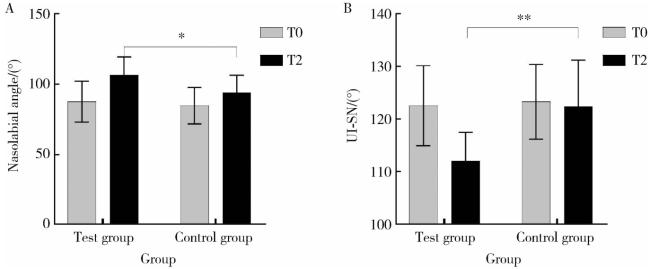
图2 T0期到T2期两组鼻唇角和上前牙唇倾角度的变化Figure 2 Nasolabial angle and UI-SN of T0 and T2 in test group and control group A, variations of nasolabial angle from T0 to T2 of test group and control group; B, variations of UI-SN from T0 to T2 of test group and control group. Student-t test, * P<0.05,* * P<0.01. UI-SN, angle of the axis of the right upper incisor and SN line. |
表4 T0期到T2期试验组和对照组的三维头影测量变化值对比Table 4 Variation of 3D cephalometric values from T0 to T2 of test group and control group |
| Parameters | Test group (n=11) | Control group (n=10) | t | P value |
| SNA/(°) | 1.82±1.59 | 2.76±1.87 | -1.245 | 0.228 |
| SNB/(°) | -3.21±1.04 | -3.62±2.44 | 0.495 | 0.629 |
| OP-SN/(°) | 1.58±2.91 | 3.29±1.81 | -1.597 | 0.127 |
| UI-SN/(°) | -10.43±4.28 | -0.94±4.89 | -4.746 | <0.001** |
| SNhR/(°) | 6.4±1.88 | 4.67±1.91 | 2.098 | 0.049* |
| SNhL/(°) | 6.79±1.48 | 5.05±2.23 | 2.122 | 0.047* |
| CKR-FP/mm | 4.78±1.22 | 1.83±1.55 | 4.886 | <0.001** |
| CKL-FP /mm | 5.15±1.74 | 2.19±1.63 | 4.005 | <0.001** |
| SAR-FP /mm | 5.24±1.71 | 3.18±1.67 | 2.782 | 0.012* |
| SAL-FP /mm | 6.1±1.94 | 3.17±1.99 | 3.421 | 0.003** |
| NL angle/(°) | 12.01±8.17 | 9.27±13.28 | 0.576 | 0.571 |
| UI-FP/mm | -0.03±1.95 | 3.05±2.44 | -3.210 | 0.005** |
All results are in normal distribution and presented as $\bar x \pm s$. Student-t test, * P<0.05,* * P<0.01. The definition of the parameters were listed under Table 2. |
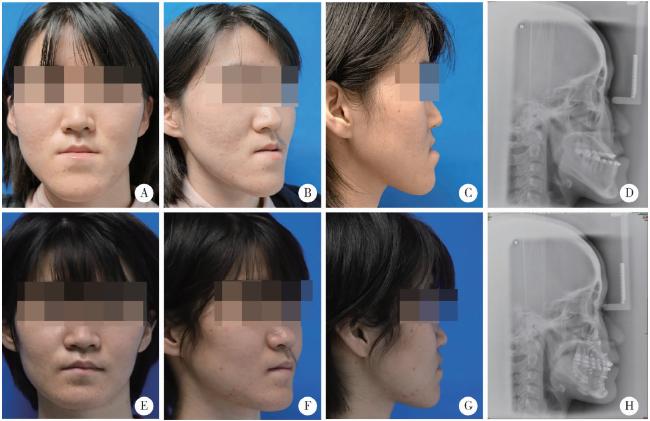
2.4 病例展示
图4 试验组患者术前(T0)和术后6个月(T2)对比Figure 4 Photographs and X-ray of a patient in test group before (T0) and 6 months after surgery (T2) A-D, frontal photograph, 45° right side photograph, right lateral photograph and cephalometric lateral radiographs of T0; E-H, frontal photograph, 45° right side photograph, right lateral photograph and cephalometric lateral radiographs of T2. |
图5 对照组患者术前(T0)和术后6个月(T2)对比Figure 5 Photographs and X-ray of a patient in control group before (T0) and 6 months after surgery (T2) A-D, frontal photograph, 45° right side photograph, right lateral photograph and cephalometric lateral radiographs of T0; E-H, frontal photograph, 45° right side photograph, right lateral photograph and cephalometric lateral radiographs of T2. |