Journal of Peking University(Health Sciences) ›› 2019, Vol. 51 ›› Issue (3): 542-547. doi: 10.19723/j.issn.1671-167X.2019.03.025
Previous Articles Next Articles
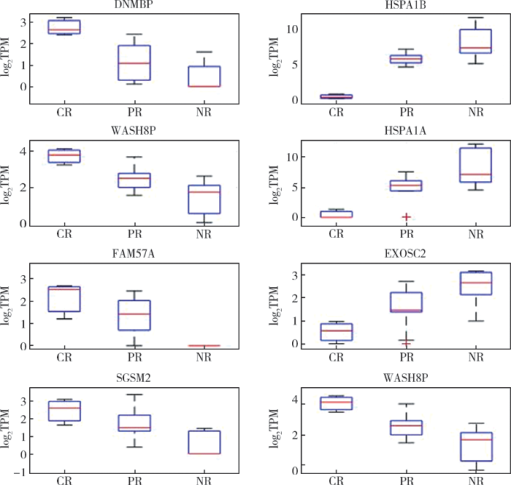
Detection of preoperative chemoradiotherapy sensitivity molecular characteristics of rectal cancer by transcriptome second generation sequencing
Wei ZHANG1,Ying-jiang YE2,Xian-wen REN3,Jing HUANG4,Zhan-long SHEN1△( )
)
CLC Number:
- R735.3
| [1] |
Park IJ, You YN, Agarwal A , et al. Neoadjuvant treatment response as an early response indicator for patients with rectal cancer[J]. J Clin Oncol, 2012,30(15):1770-1776.
doi: 10.1200/JCO.2011.39.7901 |
| [2] |
Dworak O, Keilholz L, Hoffmann A . Pathological features of rectal cancer after preoperative radiochemotherapy[J]. Int J Colorectal Dis, 1997,12(1):19-23.
doi: 10.1007/s003840050072 |
| [3] |
Rödel C, Martus P, Papadoupolos T , et al. Prognostic significance of tumor regression after preoperative chemoradiotherapy for rectal cancer[J]. J Clin Oncol, 2005,23(34):8688-8696.
doi: 10.1200/JCO.2005.02.1329 |
| [4] |
Fokas E, Liersch T, Fietkau R , et al. Tumor regression grading after preoperative chemoradiotherapy for locally advanced rectal carcinoma revisited: updated results of the CAO/ARO/AIO-94 trial[J]. J Clin Oncol, 2014,32(15):1554-1562.
doi: 10.1200/JCO.2013.54.3769 |
| [5] |
Smith JD, Ruby JA, Goodman KA , et al. Nonoperative management of rectal cancer with complete clinical response after neoadjuvant therapy[J]. Ann Surg, 2012,256(6):965-972.
doi: 10.1097/SLA.0b013e3182759f1c |
| [6] |
Postmus I, Trompet S, Deshmukh HA , et al. Pharmacogenetic meta-analysis of genome-wide association studies of LDL choleste-rol response to statins[J]. Nat Commun, 2014,5:5068.
doi: 10.1038/ncomms6068 |
| [7] | Williamson JS, Jones HG, Williams N , et al. Extramural vascular invasion and response to neoadjuvant chemoradiotherapy in rectal cancer: influence of the CpG island methylator phenotype[J]. World J Gastrointest Oncol, 2017,9(5):209-217. |
| [8] |
Chand M, Swift RI, Tekkis PP , et al. Extramural venous invasion is a potential imaging predictive biomarker of neoadjuvant treatment in rectal cancer[J]. Br J Cancer, 2014,110(1):19-25.
doi: 10.1038/bjc.2013.603 |
| [9] |
Birlik B, Obuz F, Elibol FD , et al. Diffusion-weighted MRI and MR-volumetry: in the evaluation of tumor response after preoperative chemoradiotherapy in patients with locally advanced rectal cancer[J]. Magn Reson Imaging, 2015,33(2):201-212.
doi: 10.1016/j.mri.2014.08.041 |
| [10] |
McCawley N, Clancy C, O’Neill BD , et al. Mucinous rectal adenocarcinoma is associated with a poor response to neoadjuvant chemoradiotherapy: A systematic review and meta-analysis[J]. Dis Colon Rectum, 2016,59(12):1200-1208.
doi: 10.1097/DCR.0000000000000635 |
| [11] |
Agarwal A, Chang GJ, Hu CY , et al. Quantified pathologic response assessed as residual tumor burden is a predictor of recurrence-free survival in patients with rectal cancer who undergo resection after neoadjuvant chemoradiotherapy[J]. Cancer, 2013,119(24):4231-4241.
doi: 10.1002/cncr.28331 |
| [12] |
Maas M, Nelemans PJ, Valentini V , et al. Long-term outcome in patients with a pathological complete response after chemoradiation for rectal cancer: a pooled analysis of individual patient data[J]. Lancet Oncol, 2010,11(9):835-844.
doi: 10.1016/S1470-2045(10)70172-8 |
| [13] |
Gérard JP, Chamorey E, Gourgou-Bourgade S , et al. Clinical complete response (cCR) after neoadjuvant chemoradiotherapy and conservative treatment in rectal cancer. Findings from the ACCORD 12/PRODIGE 2 randomized trial[J]. Radiother Oncol, 2015,115(2):246-252.
doi: 10.1016/j.radonc.2015.04.003 |
| [14] |
Chen MB, Wu XY, Yu R , et al. P53 status as a predictive biomarker for patients receiving neoadjuvant radiation-based treatment: a meta-analysis in rectal cancer[J]. PLoS One, 2012,7(9):e45388.
doi: 10.1371/journal.pone.0045388 |
| [15] |
D’Angelo E, Zanon C, Sensi F , et al. miR-194 as predictive biomarker of responsiveness to neoadjuvant chemoradiotherapy in patients with locally advanced rectal adenocarcinoma[J]. J Clin Pathol, 2018,71(4):344-350.
doi: 10.1136/jclinpath-2017-204690 |
| [16] |
Agostini M, Zangrando A, Pastrello C , et al. A functional biological network centered on XRCC3: a new possible marker of chemoradiotherapy resistance in rectal cancer patients[J]. Cancer Biol Ther, 2015,16(8):1160-1171.
doi: 10.1080/15384047.2015.1046652 |
| [17] | Scott JG, Berglund A, Schell MJ , et al. A genome-based model for adjusting radiotherapy dose (GARD): a retrospective, cohort-based study[J]. Lancet Oncol, 2016,18(2):202-211. |
| [18] |
Regine WF, Winter KA, Abrams RA , et al. Fluorouracil vs gemcitabine chemotherapy before and after fluorouracil-based chemoradiation following resection of pancreatic adenocarcinoma: a randomized controlled trial[J]. JAMA, 2008,299(9):1019-1026.
doi: 10.1001/jama.299.9.1019 |
| [19] |
Coveler AL, Richard P, Apisarnthanarax S , et al. Is there a best radiosensitizing agent in the treatment of locally advanced rectal cancer?[J]. Current Colorectal Cancer Reports, 2016,12(4):189-200.
doi: 10.1007/s11888-016-0324-7 |
| [20] |
Aschele C, Cionini L, Lonardi S , et al. Primary tumor response to preoperative chemoradiation with or without oxaliplatin in locally advanced rectal cancer: pathologic results of the star-01 rando-mized phase Ⅲ trial[J]. J Clin Oncol, 2011,29(20):2773-2780.
doi: 10.1200/JCO.2010.34.4911 |
| [1] | Yan XIONG,Bo ZHANG,Li-gong NIE,Shi-kai WU,Hu ZHAO,Dong LI,Ji-ting DI. Thoracic SMARCA4-deficient undifferentiated tumor-pathological diagnosis and combined immune checkpoint inhibitor treatment [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 351-356. |
| [2] | Li LIANG,Xin LI,Lin NONG,Ying DONG,Ji-xin ZHANG,Dong LI,Ting LI. Analysis of microsatellite instability in endometrial cancer: The significance of minimal microsatellite shift [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 254-261. |
| [3] | DING Ting-ting,ZENG Chu-xiong,HU Li-na,YU Ming-hua. Establishment of a prediction model for colorectal cancer immune cell infiltration based on the cancer genome atlas (TCGA) database [J]. Journal of Peking University (Health Sciences), 2022, 54(2): 203-208. |
| [4] | Xu-chu ZHANG,Jian-hua ZHANG,Rong-fu WANG,Yan FAN,Zhan-li FU,Ping YAN,Guang-yu ZHAO,Yan-xia BAI. Diagnostic value of 18F-FDG PET/CT and tumor markers (CEA, CA19-9, CA24-2) in recurrence and metastasis of postoperative colorectal moderately differentiated adenocarcinoma [J]. Journal of Peking University(Health Sciences), 2019, 51(6): 1071-1077. |
| [5] | CHEN Yang, WANG Yan-rong, SHI Yan, DAI Guang-hai. Prognostic value of chemotherapy-induced neutropenia in metastatic colon cancer patients undergoing first-line chemotherapy with FOLFOX [J]. Journal of Peking University(Health Sciences), 2017, 49(4): 669-674. |
| [6] | LIU Yan-xia, YANG Xue-song, FU Wei, YAO Hong-wei. Association of single nucleotide polymorphism rs6983267 with ulcerative colitis and colorectal cancer [J]. Journal of Peking University(Health Sciences), 2016, 48(6): 994-999. |
| [7] | SI Jing-wen, WANG Li, BA Xiao-jun, ZHANG Xu, DONG Ying, ZHANG Ji-xin, LI Wen-ting, LI Ting. Clinicopathological screening of Lynch syndrome: a report of 2 cases and literature review [J]. Journal of Peking University(Health Sciences), 2015, 47(5): 858-864. |
| [8] | LI Zhi-Hong, LIU Dan, HE Zi-Jing, FAN Zhi-Yi. Influence of dexamethasone on the incidence of postoperative nausea and vomiting in breast cancer patients with neoadjuvant chemotherapy [J]. Journal of Peking University(Health Sciences), 2015, 47(4): 685-689. |
| [9] | YUAN Chun-hui, XIU Dian-rong, GE Hui-yu, TAN Shi, WANG Hang-yan, ZHANG Li, ZHANG Tong-lin. Ultrasound guided ablation therapy of hepatic colorectal metastases: initial experience of real time virtual sonography navigation system [J]. Journal of Peking University(Health Sciences), 2013, 45(6): 956-959. |
|
||