Journal of Peking University(Health Sciences) ›› 2019, Vol. 51 ›› Issue (4): 723-727. doi: 10.19723/j.issn.1671-167X.2019.04.022
Previous Articles Next Articles
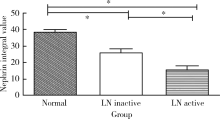
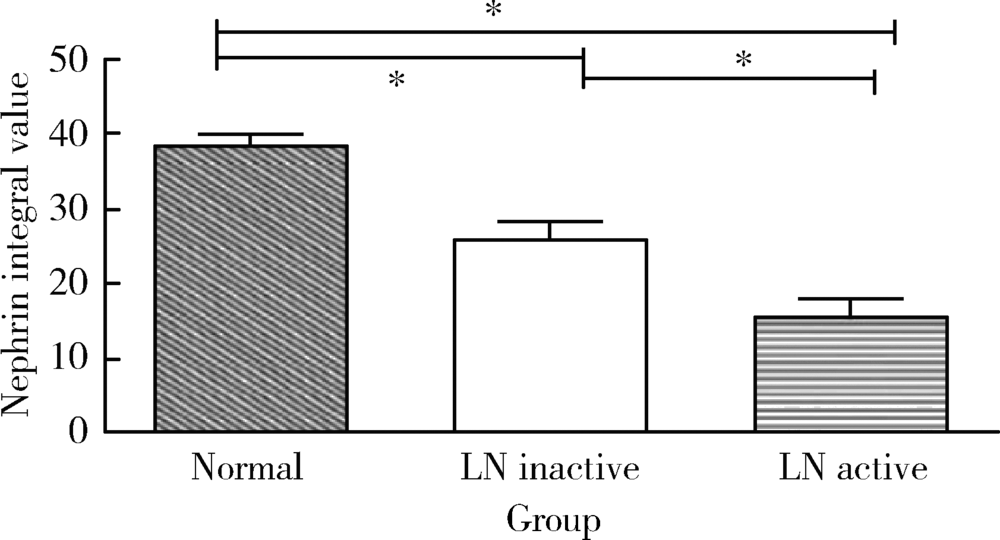
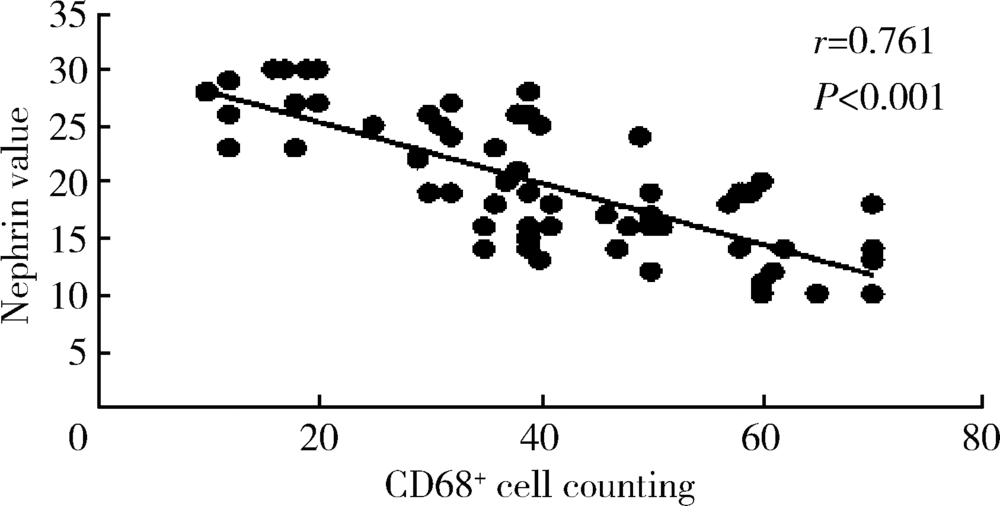
Relationship between podocyte injury and macrophage infiltration in renal tissues of patients with lupus nephritis
Ying WANG,Ming-hui LI,Yan ZHANG,Xiao-yan HU,Rui-xia MA( )
)
- Department of Nephrology, the Affiliated Hospital of Qingdao University, Qingdao 266003, Shandong, China
CLC Number:
- R593.24 +2
| [1] | Maroz N, Segal MS . Lupus nephritis and end-stage kidney disease[J]. Am J Med Sci, 2013,346(4):319-323. |
| [2] | Schiffer L, Bethunaickan R, Ramanujam M , et al. Activated renal macrophages are markers of disease onset and disease remission in lupus nephritis.[J]. J Immunol, 2008,180(3):1938-1947. |
| [3] | Koop K, Eikmans M , Baelde HJ, et a1. Expression of podocyte-associated molecules in acquired human kidney diseases[J]. J Am Soc Nephrol, 2003,14(8):2063-2071. |
| [4] | Desai N, Cimbaluk D , Lewis EJ, et a1. Proteinuria in membranous lupus nephritis: the pathology is in the podocyte[J]. Lupus, 2013,22(5):461-468. |
| [5] | 郭银凤, 赵宇, 姜彧滕 , 等. 巨噬细胞诱导糖尿病肾病足细胞凋亡及其机制[J]. 中华内分泌代谢杂志, 2017,33(8):680-686. |
| [6] | You H, Gao T, Cooper TK , et al. Macrophages directly mediate diabetic renal injury[J]. Am J Physiol Renal Physiol, 2013,305(12):F1719-F1727. |
| [7] | Hochberg MC . Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus[J]. Arthritis Rheum, 1997,40(9):1725. |
| [8] | Higgins DF, Kimura K, Bernhardt WM , et al. Hypoxia promotes fibrogenesis in vivo via HIF-1 stimulation of epithelial-to-mesenchymal transition[J]. J Clin Invest, 2007,117(12):3810-3820. |
| [9] | Mok CC. Biomarkers for lupus nephritis: a critical appraisal [J/OL]. J Biomed Biotechnol, 2010, 2010: 638413. ( 010-04-19) [2018-08-04]. . |
| [10] | Reyes-Thomas J, Blanco I, Putterman C . Urinary biomarkers in lupus nephritis[J]. Clin Rev Allergy Immunol, 2011,40(3):138-150. |
| [11] | 刘文静, 杜玄一 . 肾脏疾病足细胞保护机制研究进展[J]. 中国中西医结合肾病杂志, 2015,16(12):1112-1114. |
| [12] | Hanamura K, Tojo A, Fujita T . Urinary and glomerular podocytes in patients with chronic kidney diseases[J]. Clin Exp Nephrol, 2014,18(1):95-103. |
| [13] | 马瑞霞, 刘楠楠, 李作林 , 等. 白细胞介素-18与狼疮肾炎患者足细胞损伤关系的研究[J]. 中华风湿病学杂志, 2016,20(1):28-33. |
| [14] | 马瑞霞, 周海燕, 孙益婷 , 等. 狼疮肾炎患者肾组织淋巴细胞浸润与足细胞损伤关系的研究[J]. 中华风湿病学杂志, 2015,19(12):824-828. |
| [15] | 姜亚丽, 王媛媛, 孙世仁 , 等. 巨噬细胞在肾脏疾病治疗中的研究新进展[J]. 国际泌尿系统杂志, 2015,35(3):468-470. |
| [16] | Meng XM, Wang S, Huang XR , et al. Inflammatory macrophages can transdifferentiate into myofibroblasts during renal fibrosis[J]. Cell Death Dis, 2016,7(12):e2495. |
| [17] | Yung S, Yap DY , Chan TM. Recent advances in the understanding of renal inflammation and fibrosis in lupus nephritis [J/OL]. F1000 Res, 2017, 6 (F1000 Faculty Rev): 874. ( 2017-06-13) [2018-08-04]. . |
| [18] | Guo YF, Song ZX, Zhou M , et al. Infiltrating macrophages in diabetic nephropathy promote podocytes apoptosis via TNF-α-ROS- p38MAPK pathway[J]. Oncotarget, 2017,8(32):53276-53287. |
| [1] | Hai-hong YAO,Fan YANG,Su-mei TANG,Xia ZHANG,Jing HE,Yuan JIA. Clinical characteristics and diagnostic indicators of macrophage activation syndrome in patients with systemic lupus erythematosus and adult-onset Still's disease [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 966-974. |
| [2] | Zhi-jun LUO,Jia-jia WU,You SONG,Chun-li MEI,Rong DU. Systemic lupus erythematosus associated macrophage activation syndrome with neuropsychiatric symptoms: A report of 2 cases [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1111-1117. |
| [3] | Xiao-yan XING,Jun-xiao ZHANG,Feng-yun-zhi ZHU,Yi-fan WANG,Xin-yao ZHOU,Yu-hui LI. Clinical analysis of 5 cases of dermatomyositis complicated with macrophage activation syndrome [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1214-1218. |
| [4] | Lu ZHANG,Cheng CHEN,Mei-ting WENG,Ai-ping ZHENG,Mei-ling SU,Qing-wen WANG,Yue-ming CAI. Characteristics of serum autoantibodies in patients with lupus nephritis and tubulointerstitial damage [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1094-1098. |
| [5] | TIAN Jia-yi,ZHANG Xia,CHENG Gong,LIU Qing-hong,WANG Shi-yang,HE Jing. Serum interleukin-2 receptor α as a clinical biomarker in patients with systemic lupus erythematosus [J]. Journal of Peking University (Health Sciences), 2021, 53(6): 1083-1087. |
| [6] | Jian-mei ZOU,Li-jun WU,Cai-nan LUO,Ya-mei SHI,Xue WU. Relationship of serum 25- hydroxy vitamin D and systemic lupus erythematosus [J]. Journal of Peking University (Health Sciences), 2021, 53(5): 938-941. |
| [7] | Ying-yi CHEN,Zi-qi HU,Tian-qian HUI,He LIU. Enhancer of zeste homolog 2 affects dental pulp inflammation by regulating macrophage chemotaxis [J]. Journal of Peking University(Health Sciences), 2020, 52(1): 18-23. |
| [8] | Hai-hong YAO,Yi-ni WANG,Xia ZHANG,Jin-xia ZHAO,Yuan JIA,Zhao WANG,Zhan-guo LI. Clinical characteristics and treatment outcomes of macrophage activation syndrome in adults: A case series of 67 patients [J]. Journal of Peking University(Health Sciences), 2019, 51(6): 996-1002. |
| [9] | Yan-rui ZHAO,Yang LIU,Dong WANG,Wen-rui LV,Jun-lin ZHOU. Effects of sulfur dioxide on alveolar macrophage apoptosis in acute lung injury induced by limb ischemia/reperfusion in rats [J]. Journal of Peking University(Health Sciences), 2019, 51(2): 239-244. |
| [10] | Shuang LIU,Yu-long GUO,Jing-yi YANG,Wei WANG,Jian XU. Efficacy of mesenchymal stem cells on systemic lupus erythematosus:a meta-analysis [J]. Journal of Peking University(Health Sciences), 2018, 50(6): 1014-1021. |
| [11] | GAO Xiang, CHEN Xiang-mei, ZHANG Ting, ZHANG Jing, CHEN Mo, GUO Zheng--yang, SHI Yan-yan, LU Feng-min, DING Shi-gang. Relationship between macrophage capping protein and gastric cancer cell’s proliferation and migration ability [J]. Journal of Peking University(Health Sciences), 2017, 49(3): 489-494. |
|
||