Journal of Peking University(Health Sciences) ›› 2019, Vol. 51 ›› Issue (6): 1048-1051. doi: 10.19723/j.issn.1671-167X.2019.06.012
Previous Articles Next Articles
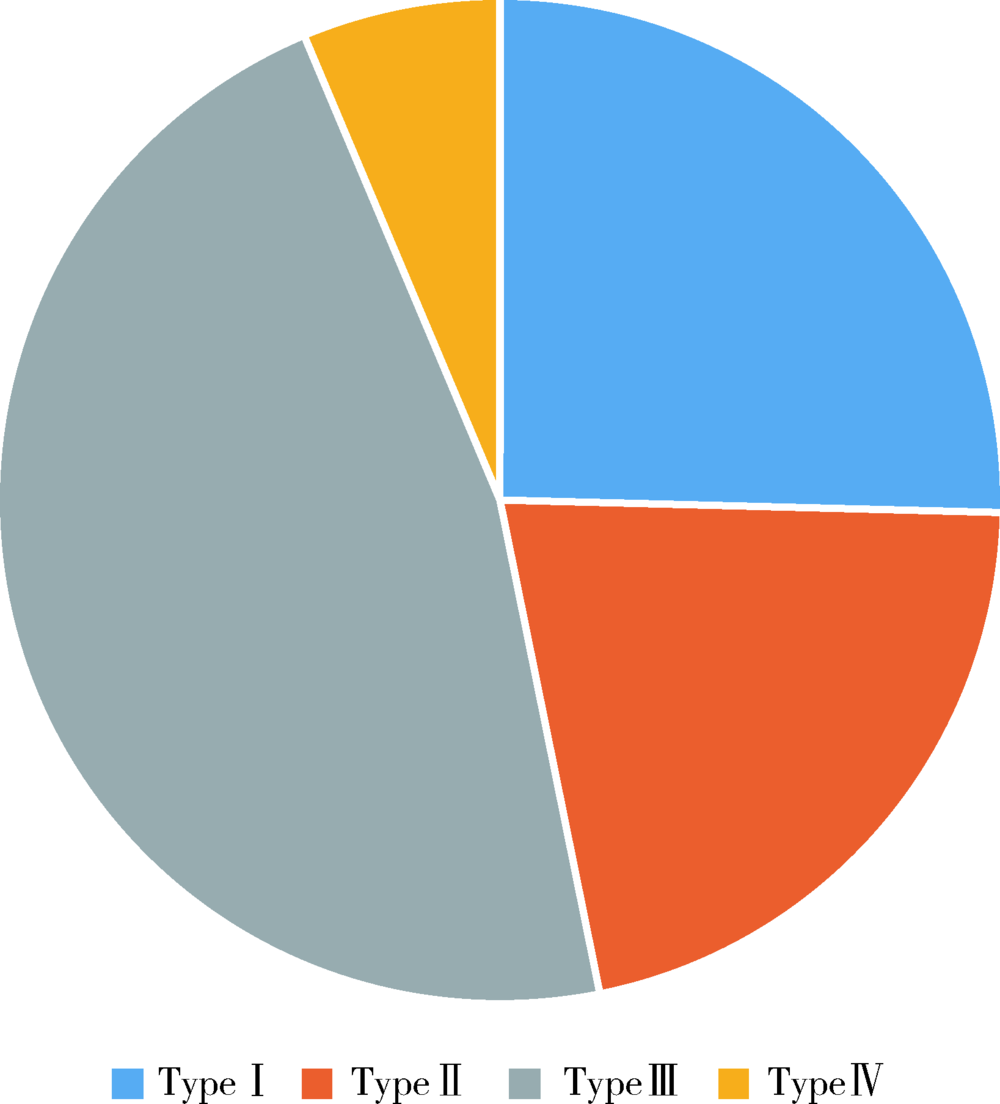
Urodynamic classification of male patients with symptoms of overactive bladder and the outcome classification
Tao WANG,Ke-xin XU,Wei-yu ZHANG,Hao HU,Xiao-wei ZHANG,Huan-rui WANG,Xian-hui LIU,Jing-wen CHEN,Xiao-peng ZHANG( )
)
- Department of Urology, Peking University People’s Hospital, Beijing 100044, China
CLC Number:
- R694
| [1] | Abrams P, Cardoz L, Fall M , et al. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society[J]. Neurourol Urodyn, 2002,21(2):167-178. |
| [2] | Kurosch M, Mager R, Gust K , et al. Diagnosis of overactive bladder (OAB)[J]. Urologe A, 2015,54(3):421-427. |
| [3] | Chen SL, Ng SC, Huang YH, Chen GD . Are patients with bladder oversensitivity different from those with urodynamically proven detrusor overactivity in female overactive bladder syndrome?[J]. J Chin Med Assoc, 2017,80(10):644-650. |
| [4] | D’Ancona CA, Bassani JW, Querne FA , et al. New method for minimally invasive urodynamic assessment in men with lower urinary tract symptoms[J]. Urology, 2008,71(1):75-78. |
| [5] | Flisser AJ, Walmsley K, Blaivas JG . Urodynamic classification of patients with symptoms of overactive bladder[J]. J Urol, 2003,169(2):529-533. |
| [6] | Fall M, Geirsson G, Lindstrom S . Toward a new classification of overactive bladders[J]. Neurourol Urodyn, 1995,14(6):635-646. |
| [7] | Yamaguchi O, Nishizawa O, Takeda M , et al. Clinical guidelines for overactive bladder[J]. Int J Urol, 2009,16(2):126-142. |
| [8] | Höfner K . Terminology and pathophysiology of overactive bladder (OAB)[J]. Aktuelle Urol, 2016,47(6):468-474. |
| [9] | Daly D, Chapple C . Relationship between overactive bladder (OAB) and irritable bowel syndrome (IBS): concurrent disorders with a common pathophysiology?[J]. BJU Int, 2013,111(4):530-531. |
| [10] | Vahabi B, Drake MJ . Physiological and pathophysiological implications of micromotion activity in urinary bladder function[J]. Acta Physiol (Oxf), 2015,213(2):360-370. |
| [11] | Bothig R, Domurath B, Kaufmann A , et al. Neuro-urological diagnosis and therapy of lower urinary tract dysfunction in patients with spinal cord injury: S2k Guideline of the German-Speaking Medical Society of Paraplegia (DMGP)[J]. Urologe A, 2017,56(6):785-792. |
| [12] | Mehnert U, Nehiba M . Neuro-urological dysfunction of the lower urinary tract in CNS diseases: pathophysiology, epidemiology, and treatment options[J]. Urologe A, 2012,51(2):189-197. |
| [13] | Gill BC, Pizarro-Berdichevsky J, Bhattacharyya PK , et al. Real-time changes in brain activity during sacral neuromodulation for overactive bladder[J]. J Urol, 2017,198(6):1379-1385. |
| [14] | Sakakibara R, Panicker J, Fowler CJ , et al. Is overactive bladder a brain disease? The pathophysiological role of cerebral white matter in the elderly[J]. Int J Urol, 2014,21(1):33-38. |
| [15] | Elser DM . Stress urinary incontinence and overactive bladder syndrome: current options and new targets for management[J]. Postgrad Med, 2012,124(3):42-49. |
| [1] | Hanwei KE, Qi WANG, Kexin XU. Optimization study of an animal model for interstitial cystitis/bladder pain syndrome based on the dose effect of cyclophosphamide [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 908-912. |
| [2] | Ye YAN,Xiaolong LI,Haizhui XIA,Xuehua ZHU,Yuting ZHANG,Fan ZHANG,Ke LIU,Cheng LIU,Lulin MA. Analysis of risk factors for long-term overactive bladder after radical prostatectomy [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 589-593. |
| [3] | Yuqing LI,Biao WANG,Peng QIAO,Wei WANG,Xing GUAN. Medium to long-term efficacy of tension-free vaginal tape procedure in the treatment of female recurrent stress urinary incontinence [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 600-604. |
| [4] | Yifan WU,Yingxiang YU,Lan XIE,Zhida ZHANG,Cuiqing CHANG. Characteristics of resting energy expenditure and evaluation of prediction formulas in young men with different body mass indexes [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 247-252. |
| [5] | Zi-kai WANG,Jia-li MO,Meng ZHANG,Ji-ping LIAO. Epidemiology and hospitalization costs analysis of female inpatients with acute exacerbation of chronic obstructive pulmonary disease in Beijing from 2013 to 2020 [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1074-1081. |
| [6] | Xue-zhao JI,Shan LIU,Wan-zhou WANG,Ye-tong ZHAO,Lu-yi LI,Wen-lou ZHANG,Guo-feng SHEN,Fu-rong DENG,Xin-biao GUO. Associations between indoor volatile organic compounds and nocturnal heart rate variability of young female adults: A panel study [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 488-494. |
| [7] | Hao LIN,Jing-hua LI,Xiao YANG,Xiao-ting CHEN,Yu-hui SHI,Chun CHANG,Yuan-tao HAO,Wang-nan CAO. Discrepancy between behavioral-indicated and perceived candidacy for HIV pre-exposure prophylaxis among men who have sex with men in Chengdu, China [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 511-520. |
| [8] | Xi-ya SUN,Yi-lu CHEN,Lin ZENG,Li-ying YAN,Jie QIAO,Rong LI,Xu ZHI. Correlation analysis of vitamin D level and anti-Müllerian hormone in infertile female and the role in predicting pregnancy outcome [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 167-173. |
| [9] | Lin ZHU,Wei-yu ZHANG,Ke-xin XU. Urodynamic and histological evaluation of cyclophosphamide-induced bladder pain syndrome in SD rats [J]. Journal of Peking University (Health Sciences), 2022, 54(4): 735-740. |
| [10] | DU Qiang,HONG Kai,PAN Bo-chen. Comparison of two methods for detection of Chlamydia trachomatis and Ureaplasma urealyticum in male reproductive tract [J]. Journal of Peking University (Health Sciences), 2021, 53(4): 785-788. |
| [11] | WANG Qi,ZHANG Wei-yu,LIU Xian-hui,WANG Ming-rui,LAI Jin-hui,HU Hao,XU Tao,XU Ke-xin. Therapeutic effects of sacral neuromodulation on detrusor underactivity [J]. Journal of Peking University (Health Sciences), 2021, 53(4): 671-674. |
| [12] | Wei-yu ZHANG,Qiu-xiang XIA,Hao HU,Jing-wen CHEN,Yi-ran SUN,Ke-xin XU,Xiao-peng ZHANG. Analysis of urodynamic study of female outpatients with lower urinary tract symptoms and follow-up of the patients with detrusor underactive [J]. Journal of Peking University(Health Sciences), 2019, 51(5): 856-862. |
| [13] | Xin-yan CHE,Shi-liang WU,Yu-ke CHEN,Yan-bo HUANG,Yang YANG. A survey of risk factors and quality of life in female medical staff with urinary incontinence [J]. Journal of Peking University(Health Sciences), 2019, 51(4): 706-710. |
| [14] | DAI Xiao-wei, XU Ying, ZHENG Lian-wen, LI Ling-yun, LI Dan-dan1 TAN Xin, GAO Fei, WANG Yan, WU Gui-jie. Analysis of chromosome in 1 324 patients with oligozoospermia or azoosperm [J]. Journal of Peking University(Health Sciences), 2018, 50(5): 774-777. |
| [15] | WU Gui-jie, MA Shuai, ZHENG Lian-wen, XU Ying, MENG Fan-he, DAI Xiao-wei. A complex chromosome translocation with male infertility of karyotype analysis and literature review [J]. Journal of Peking University(Health Sciences), 2018, 50(4): 729-731. |
|
||