Journal of Peking University (Health Sciences) ›› 2021, Vol. 53 ›› Issue (3): 549-554. doi: 10.19723/j.issn.1671-167X.2021.03.018
Previous Articles Next Articles
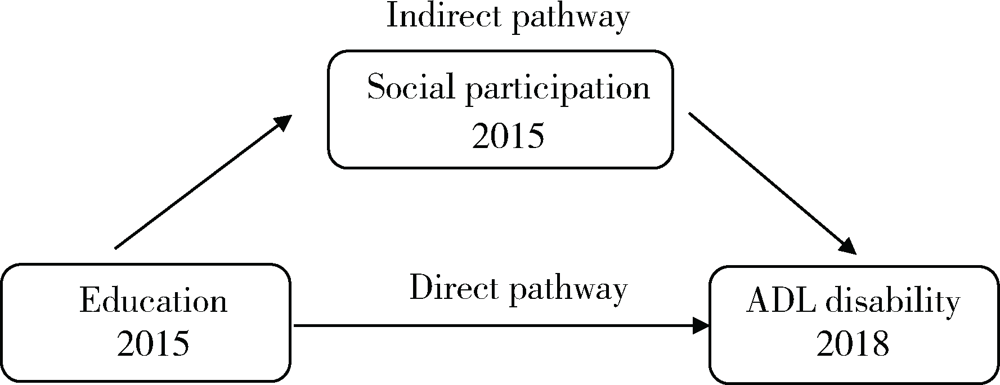
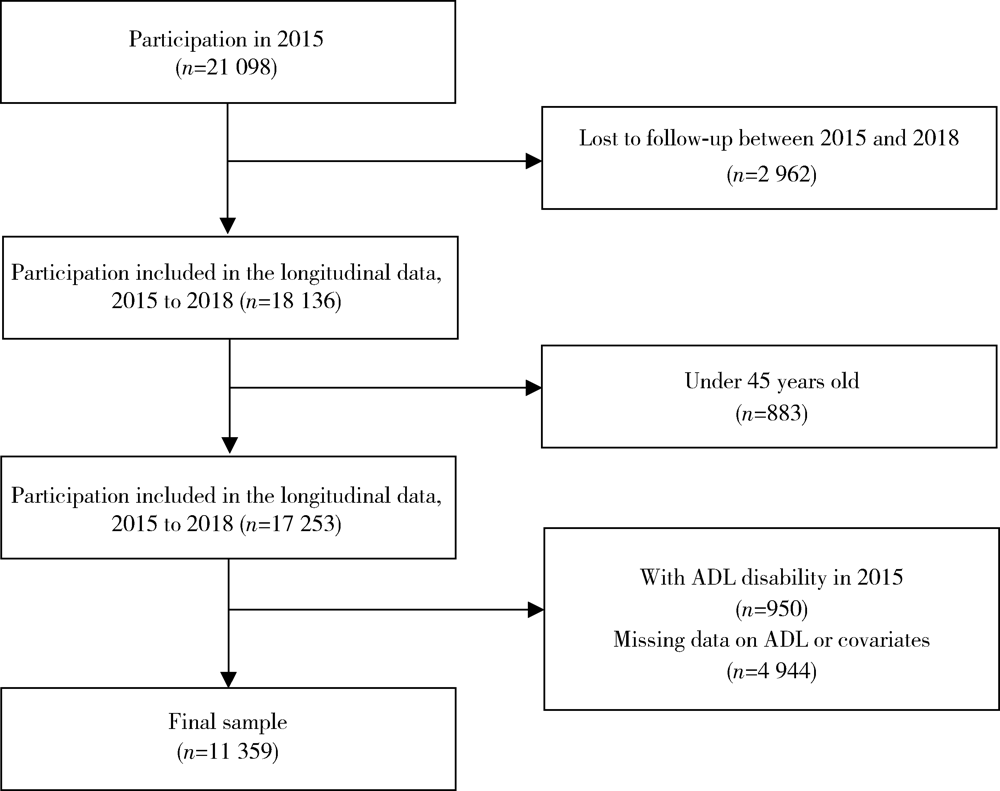
Association between education and the onset of disability in activities of daily living in middle-aged and older Chinese adults: The mediator role of social participation
PENG Shun-zhuang,FU Xi-xi,FENG Xing-linΔ( )
)
- Department of Health Policy and Management, Peking University School of Public Health, Beijing 100191, China
CLC Number:
- R195
| [1] | 中华人民共和国国家统计局. 中国统计年鉴 [M]. 北京: 中国统计出版社, 2019: 9-24. |
| [2] | 中华人民共和国民政部. 三部门发布第四次中国城乡老年人生活状况抽样调查成果 [EB/OL]. (2016-10-09) [2021-02-10]. http://jnjd.mca.gov.cn/article/zyjd/xxck/201610/20161000886652.shtml. |
| [3] |
Minkler M, Fuller-Thomson E, Guralnik JM. Gradient of disability across the socioeconomic spectrum in the United States[J]. N Engl J Med, 2006,355(7):695-703.
doi: 10.1056/NEJMsa044316 |
| [4] | 张文娟, 魏蒙. 中国老年人的失能水平和时间估计: 基于合并数据的分析[J]. 人口研究, 2015,39(5):3-14. |
| [5] | 尹志勤, 杨玉霞, 陈丽莉, 等. 浙江省农村老年人健康状况及影响因素分析[J]. 中国公共卫生, 2012,28(3):293-295. |
| [6] |
Zimmer Z, House JS. Education, income, and functional limitation transitions among American adults: contrasting onset and progression[J]. Int J Epidemiol, 2003,32(6):1089-1097.
doi: 10.1093/ije/dyg254 |
| [7] | 朱春燕, 郭晴, 田庆丰, 等. 河南省老年人综合能力失能现况及影响因素研究[J]. 中国全科医学, 2021,24(12):1500-1505. |
| [8] |
Ma X, Piao X, Oshio T. Impact of social participation on health among middle-aged and elderly adults: evidence from longitudinal survey data in China[J]. BMC Public Health, 2020,20(1):502.
doi: 10.1186/s12889-020-08650-4 |
| [9] |
Aida J, Kondo K, Kawachi I, et al. Does social capital affect the incidence of functional disability in older Japanese? A prospective population-based cohort study[J]. J Epidemiol Community Health, 2013,67(1):42-47.
doi: 10.1136/jech-2011-200307 pmid: 22760221 |
| [10] |
Katz S, Ford AB, Moskowitz RW, et al. Studies of illness in the aged: The index of ADL: A standardized measure of biological and psychosocial function[J]. JAMA, 1963,185(12):914-919.
doi: 10.1001/jama.1963.03060120024016 |
| [11] |
Liu N, Cadilhac DA, Kilkenny MF, et al. Changes in the prevalence of chronic disability in China: evidence from the China Health and Retirement Longitudinal Study[J]. Public Health, 2020,185:102-109.
doi: S0033-3506(20)30104-9 pmid: 32603874 |
| [12] |
Liu GG, Xue X, Yu C, et al. How does social capital matter to the health status of older adults? Evidence from the China Health and Retirement Longitudinal Survey[J]. Econ Hum Biol, 2016,22:177-189.
doi: 10.1016/j.ehb.2016.04.003 |
| [13] |
Kohler U, Karlson KB, Holm A. Comparing coefficients of nested nonlinear probability models[J]. Stata J, 2011,11(3):420-438.
doi: 10.1177/1536867X1101100306 |
| [14] |
Xu X, Yang L, Miao X, et al. An investigation and analysis of the activities of daily living of older adults living at home in Ningxia Hui Autonomous Region of China: A cross-sectional study[J]. BMC Geriatr, 2020,20(1):369.
doi: 10.1186/s12877-020-01765-8 |
| [15] |
Enroth L, Veenstra M, Aartsen M, et al. Are there educational disparities in health and functioning among the oldest old? Evidence from the Nordic countries[J]. Eur J Ageing, 2019,16(4):415-424.
doi: 10.1007/s10433-019-00517-x pmid: 31798367 |
| [16] | 林雁, 董正娇, 许传志, 等. 昆明市社区60岁以上老年人失能状况、影响因素及与健康效用的关系[J]. 昆明医科大学学报, 2020,41(4):44-50. |
| [17] |
Xin Y, Ren X. Social capital as a mediator through the effect of education on depression and obesity among the elderly in China[J]. Int J Environ Res Public Health, 2020,17(11):3977.
doi: 10.3390/ijerph17113977 |
| [18] | Eikemo TA, Bambra C, Huijts T, et al. The first pan-European sociological health inequalities survey of the general population: The European social survey rotating module on the social determinants of health[J]. Eur Sociol Rev, 2016,33(1):137-153. |
| [19] | Feng Z, Cramm JM, Jin C, et al. The longitudinal relationship between income and social participation among Chinese older people[J]. SSM Popul Health, 2020,11:100636. |
| [20] |
Scheffler RM, Brown TT. Social capital, economics, and health: new evidence[J]. Health Econ Policy Law, 2008,3(Pt 4):321-331.
doi: 10.1017/S1744133108004593 pmid: 18793475 |
| [21] | 中华人民共和国中央人民政府. 中共中央国务院印发《“健康中国2030”规划纲要》 [EB/OL]. (2016-10-25) [2021-02-10]. http://www.gov.cn/zhengce/2016-10/25/content_5124174.htm. |
| [22] | 中华人民共和国中央人民政府. 健康中国行动(2019—2030年) [EB/OL]. (2019-07-15) [2021-02-10]. http://www.gov.cn/xinwen/2019-07/15/content_5409694.htm. |
| [1] | Haoyu ZHANG,Yiwen SHI,Wei PAN,Aiping LIU,Xinying SUN,Man LI,Xuxi ZHANG. Factors associated with the care needs of the older adults based on different disability levels [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 431-440. |
| [2] | Ting JING,Hua JIANG,Ting LI,Qianqian SHEN,Lan YE,Yindan ZENG,Wenxin LIANG,Gang FENG,Man-Yau Szeto Ignatius,Yumei ZHANG. Relationship between serum 25-hydroxyvitamin D and handgrip strength in middle-aged and elderly people in five cities of Western China [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 448-455. |
| [3] | Yuting LIN,Huali WANG,Yu TIAN,Litong GONG,Chun CHANG. Factors influencing cognitive function among the older adults in Beijing [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 456-461. |
| [4] | Huameng TANG,Dianqi YUAN,Mingxing WANG,Hanbing YANG,Chao GUO. Sequential mediating role of digital participation and health lifestyle in the relationship between socioeconomic status and depression of older adults [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 230-238. |
| [5] | Hui-li LIU,Yan-han LV,Xiao-xiao WANG,Min LI. Factors influencing the chronic post-surgical pain after laparoscopic surgery for elderly patients with urinary tract tumors [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 851-856. |
| [6] | Chun-su ZHU,Zhi-wei LIAN,Yi-min CUI. Association between depression and chronic diseases among middle-aged and older Chinese adults [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 606-611. |
| [7] | Guang-qi LIU,Yuan-jie PANG,Jiang WU,Min LV,Meng-ke YU,Yu-tong LI,Yang-mu HUANG. Trend analysis of influenza vaccination among hospitalized elderly people in Beijing, 2013-2019 [J]. Journal of Peking University (Health Sciences), 2022, 54(3): 505-510. |
| [8] | LI Jia,XU Yu,WANG You-ya,GAO Zhan-cheng. Clinical characteristics of influenza pneumonia in the elderly and relationship between D-dimer and disease severity [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 153-160. |
| [9] | LI Zhi-chang,HOU Yun-fei,ZHOU Zhi-wei,JIANG Long,ZHANG Shu,LIN Jian-hao. Patient factors influencing preoperative expectations of patients undergoing total knee arthroplasty [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 170-176. |
| [10] | Jia-li CHEN,Yue-bo JIN,Yi-fan WANG,Xiao-ying ZHANG,Jing LI,Hai-hong YAO,Jing HE,Chun LI. Clinical characteristics and risk factors of cardiovascular disease in patients with elderly-onset rheumatoid arthritis: A large cross-sectional clinical study [J]. Journal of Peking University (Health Sciences), 2020, 52(6): 1040-1047. |
| [11] | Zhe-bin WANG,Zhi-jie ZHENG. Research on equity and influencing factors of disability among Chinese middle-aged and old people [J]. Journal of Peking University (Health Sciences), 2020, 52(3): 500-505. |
| [12] | Yi SONG,Dong-mei LUO,Pei-jin HU,Xiao-jin YAN,Jing-shu ZHANG,Yuan-ting LEI,Bing ZHANG,Jun MA. Trends of prevalence of excellent health status and physical fitness among Chinese Han students aged 13 to 18 years from 1985 to 2014 [J]. Journal of Peking University (Health Sciences), 2020, 52(2): 317-322. |
| [13] | XU Xiao-feng, CHEN Qian, ZHAO Yi-pu, HU Xiu-ying. Investigation and analysis of the activities of daily living of the aged at home in wes-tern China [J]. Journal of Peking University(Health Sciences), 2018, 50(3): 457-462. |
| [14] | ZHANG Yi-xiao, FENG Wen. Decision tree analysis in determinants of elderly visits in poor rural areas [J]. Journal of Peking University(Health Sciences), 2018, 50(3): 450-456. |
| [15] | ZHANG Lu-feng, LING Yun-peng, YANG Hang, GONG Yi-chen, SONG Zhi-ming, WAN Feng. Comparison of outcomes of two minimally invasive approaches for multi-vessel coronary revascularization [J]. Journal of Peking University(Health Sciences), 2017, 49(6): 1066-1070. |
|
||