Journal of Peking University (Health Sciences) ›› 2022, Vol. 54 ›› Issue (2): 369-375. doi: 10.19723/j.issn.1671-167X.2022.02.027
Previous Articles Next Articles
Pituitary immune-related adverse events induced by programmed cell death protein 1 inhibitors in advanced lung cancer patients: A report of 3 cases
GU Yang-chun1,LIU Ying2,XIE Chao3,CAO Bao-shan1,△( )
)
- 1. Department of Medical Oncology and Radiation Sickness, Peking University Third Hospital, Beijing 100191, China
2. Department of Radiology, Peking University Third Hospital, Beijing 100191, China
3. Department of Endocrinology, Peking University Third Hospital, Beijing 100191, China
CLC Number:
- R730.51
| [1] |
Deligiorgi MV, Liapi C, Trafalis DT. Hypophysitis related to immune checkpoint inhibitors: An intriguing adverse event with many faces[J]. Expert Opin Biol Ther, 2021, 21(8):1097-1120.
doi: 10.1080/14712598.2021.1869211 |
| [2] |
Stelmachowska-Banaś M, Czajka-Oraniec I. Management of endocrine immune-related adverse events of immune checkpoint inhibitors: An updated review[J]. Endocr Connect, 2020, 9(10):R207-R228.
doi: 10.1530/EC-20-0342 pmid: 33064663 |
| [3] |
Barroso-Sousa R, Barry WT, Garrido-Castro AC, et al. Incidence of endocrine dysfunction following the use of different immune checkpoint inhibitor regimens: A systematic review and meta-analysis[J]. JAMA Oncol, 2018, 4(2):173-182.
doi: 10.1001/jamaoncol.2017.3064 pmid: 28973656 |
| [4] |
de Filette J, Andreescu CE, Cools F, et al. A systematic review and meta-analysis of endocrine-related adverse events associated with immune checkpoint inhibitors[J]. Horm Metab Res, 2019, 51(3):145-156.
doi: 10.1055/a-0843-3366 pmid: 30861560 |
| [5] | Baxi S, Yang A, Gennarelli RL, et al. Immune-related adverse events for anti-PD-1 and anti-PD-L1 drugs: Systematic review and meta-analysis[J]. BMJ, 2018(360):k793. |
| [6] |
Kobayashi T, Iwama S, Yasuda Y, et al. Pituitary dysfunction induced by immune checkpoint inhibitors is associated with better overall survival in both malignant melanoma and non-small cell lung carcinoma: A prospective study[J]. J Immunother Cancer, 2020, 8(2):e000779.
doi: 10.1136/jitc-2020-000779 |
| [7] |
Di Dalmazi G, Ippolito S, Lupi I, et al. Hypophysitis induced by immune checkpoint inhibitors: A 10-year assessment[J]. Expert Rev Endocrinol Metab, 2019, 14(6):381-398.
doi: 10.1080/17446651.2019.1701434 pmid: 31842671 |
| [8] |
Takeno A, Yamamoto M, Morita M, et al. Late-onset isolated adrenocorticotropic hormone deficiency caused by nivolumab: A case report[J]. BMC Endocr Disord, 2019, 19(1):25.
doi: 10.1186/s12902-019-0335-x pmid: 30782163 |
| [9] |
Antoniou S, Bazazo G, Röckl L, et al. Late-onset hypophysitis after discontinuation of nivolumab treatment for advanced skin melanoma: A case report[J]. BMC Endocr Disord, 2021, 21(1):191.
doi: 10.1186/s12902-021-00854-y pmid: 34544399 |
| [10] |
Kanie K, Iguchi G, Bando H, et al. Two cases of atezolizumab-induced hypophysitis[J]. J Endocr Soc, 2017, 2(1):91-95.
doi: 10.1210/js.2017-00414 |
| [11] |
Ohara N, Kobayashi M, Ohashi K, et al. Isolated adrenocorticotropic hormone deficiency and thyroiditis associated with nivolumab therapy in a patient with advanced lung adenocarcinoma: A case report and review of the literature[J]. J Med Case Rep, 2019, 13(1):88.
doi: 10.1186/s13256-019-2002-2 |
| [12] |
Iwama S, Kobayashi T, Arima H. Clinical characteristics, ma-nagement, and potential biomarkers of endocrine dysfunction induced by immune checkpoint inhibitors[J]. Endocrinol Metab (Seoul), 2021, 36(2):312-321.
doi: 10.3803/EnM.2021.1007 |
| [13] | United States National Cancer Institute. Common terminology criteria for adverse events (CTCAE)[S/OL]. (2017-11-27). [2021-11-23]. https://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/CTCAE_v5_Quick_Reference_5x7.pdf. |
| [14] |
Nguyen H, Shah K, Waguespack SG, et al. Immune checkpoint inhibitor related hypophysitis: Diagnostic criteria and recovery patterns[J]. Endocr Relat Cancer, 2021, 28(7):419-431.
doi: 10.1530/ERC-20-0513 |
| [15] |
Faje A, Reynolds K, Zubiri L, et al. Hypophysitis secondary to nivolumab and pembrolizumab is a clinical entity distinct from ipilimumab-associated hypophysitis[J]. Eur J Endocrinol, 2019, 181(3):211-219.
doi: 10.1530/EJE-19-0238 |
| [16] |
Kanie K, Iguchi G, Bando H, et al. Mechanistic insights into immune checkpoint inhibitor-related hypophysitis: A form of paraneoplastic syndrome[J]. Cancer Immunol Immunother, 2021, 70(12):3669-3677.
doi: 10.1007/s00262-021-02955-y |
| [17] |
Paz-Ares L, Luft A, Vicente D, et al. Pembrolizumab plus chemo-therapy for squamous non-small-cell lung cancer[J]. N Engl J Med, 2018, 379(21):2040-2051.
doi: 10.1056/NEJMoa1810865 |
| [18] |
Gandhi L, Rodriguez-Abreu D, Gadgeel S, et al. Pembrolizumab plus chemotherapy in metastatic non-small-cell lung cancer[J]. N Engl J Med, 2018, 378(22):2078-2092.
doi: 10.1056/NEJMoa1801005 |
| [19] |
Amereller F, Deutschbein T, Joshi M, et al. Differences between immunotherapy-induced and primary hypophysitis: A multicenter retrospective study[J]. Pituitary, 2022, 25(1):152-158.
doi: 10.1007/s11102-021-01182-z |
| [20] |
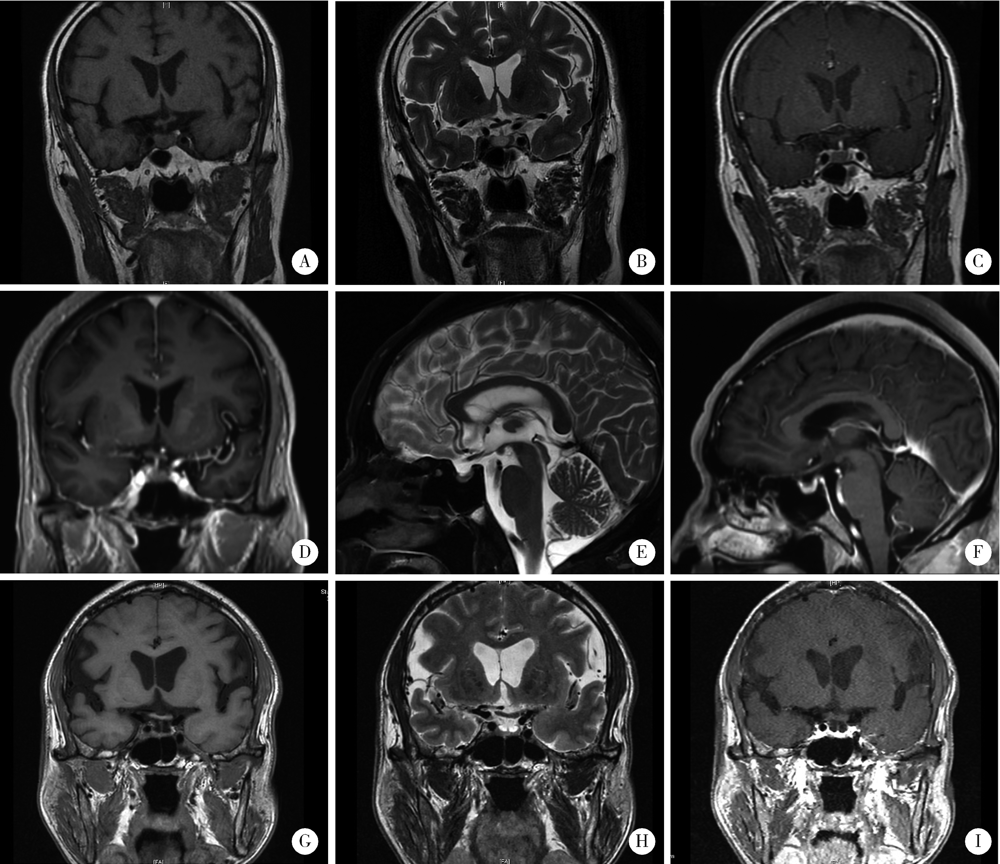
Kurokawa R, Ota Y, Gonoi W, et al. MRI findings of immune checkpoint inhibitor-induced hypophysitis: Possible association with fibrosis[J]. Am J Neuroradiol, 2020; 41(9):1683-1689.
doi: 10.3174/ajnr.A6692 pmid: 32763900 |
| [21] |
Seethapathy H, Rusibamayila N, Chute DF, et al. Hyponatremia and other electrolyte abnormalities in patients receiving immune checkpoint inhibitors[J]. Nephrol Dial Transplant, 2021, 36(12):2241-2247.
doi: 10.1093/ndt/gfaa272 |
| [22] | 中华医学会内分泌学分会免疫内分泌学组. 免疫检查点抑制剂引起的内分泌系统免疫相关不良反应专家共识(2020)[J]. 中华内分泌代谢杂志, 2021, 37(1):1-16. |
| [23] | Management of Immunotherpy-Related Toxicities. National comphrehensive cancer network (NCCN) guidelines[R/OL]. Version 4. (2021-09-27) [2021-11-23]. https://www.nccn.org/professionals/physician_gls/pdf/immunotherapy.pdf. |
| [24] | 中国临床肿瘤学会(CSCO). 免疫检查点抑制剂相关的毒性管理指南2021[R]. 北京: 人民卫生出版社, 2021. |
| [25] |
Cooksley T, Girotra M, Ginex P, et al. Multinational association of supportive care in cancer (MASCC) 2020 clinical practice re-commendations for the management of immune checkpoint inhibitor endocrinopathies and the role of advanced practice providers in the management of immune-mediated toxicities[J]. Support Care Cancer, 2020, 28(12):6175-6181.
doi: 10.1007/s00520-020-05709-1 |
| [26] |
Chang LS, Barroso-Sousa R, Tolaney SM, et al. Endocrine toxicity of cancer immunotherapy targeting immune checkpoints[J]. Endocr Rev, 2019, 40(1):17-65.
doi: 10.1210/er.2018-00006 |
| [27] | Faje AT, Lawrence D, Flaherty K, et al. High-dose glucocorticoids for the treatment of ipilimumab-induced hypophysitis is associated with reduced survival in patients with melanoma[J]. Can-cer, 2018, 124(18):3706-3714. |
| [28] |
Fernandes S, Varlamov EV, McCartney S, et al. A novel etiology of hypophysitis: Immune checkpoint inhibitors[J]. Endocrinol Metab Clin North Am, 2020, 49(3):387-399.
doi: 10.1016/j.ecl.2020.05.002 |
| [29] | Iwama S, De Remigis A, Callahan MK, et al. Pituitary expression of CTLA-4 mediates hypophysitis secondary to administration of CTLA-4 blocking antibody[J]. Sci Transl Med, 2014, 6(230): 230ra45. |
| [30] |
Caturegli P, Di Dalmazi G, Lombardi M, et al. Hypophysitis se-condary to cytotoxic T-lymphocyte-associated protein 4 blockade: Insights into pathogenesis from an autopsy series[J]. Am J Pathol, 2016, 186(12):3225-3235.
doi: S0002-9440(16)30379-0 pmid: 27750046 |
| [31] |
Mihic-Probst D, Reinehr M, Dettwiler S, et al. The role of macrophages type 2 and T-regs in immune checkpoint inhibitor related adverse events[J]. Immunobiology, 2020, 225(5):152009.
doi: 10.1016/j.imbio.2020.152009 |
| [32] |
Kobayashi T, Iwama S, Sugiyama D, et al. Anti-pituitary antibo-dies and susceptible human leukocyte antigen alleles as predictive biomarkers for pituitary dysfunction induced by immune checkpoint inhibitors[J]. J Immunother Cancer, 2021, 9(5):e002493.
doi: 10.1136/jitc-2021-002493 |
| [1] | Wei WANG,Jia-ning WANG,Wei YU,Sai-nan ZHU,Ying GAO,Jun-qing ZHANG. Comparison of coagulation function between adrenocorticotropic hormone independent Cushing syndrome and nonfunctional adrenal adenoma and its influence factors [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1062-1067. |
| [2] | Sheng-jie LIU,Hui-min HOU,Zheng-tong LV,Xin DING,Lu WANG,Lei ZHANG,Ming LIU. Bipolar androgen therapy followed by immune checkpoint inhibitors in metastatic castration resistant prostate cancer: A report of 4 cases [J]. Journal of Peking University (Health Sciences), 2022, 54(4): 766-769. |
| [3] | Cai-peng QIN,Yu-xuan SONG,Meng-ting DING,Fei WANG,Jia-xing LIN,Wen-bo YANG,Yi-qing DU,Qing LI,Shi-jun LIU,Tao XU. Establishment of a mutation prediction model for evaluating the efficacy of immunotherapy in renal carcinoma [J]. Journal of Peking University (Health Sciences), 2022, 54(4): 663-668. |
| [4] | Yi-cen YING,Qi TANG,Kai-wei YANG,Yue MI,Yu FAN,Wei YU,Yi SONG,Zhi-song HE,Li-qun ZHOU,Xue-song LI. Clinical features of immune checkpoint inhibitor-related myositis in patients with urological cancer [J]. Journal of Peking University (Health Sciences), 2022, 54(4): 644-651. |
| [5] | LIAO Xu-he,WANG Rong-fu,LIU Meng,CHEN Xue-qi,XIONG Yan,NONG Lin,YIN Lei,ZHANG Bing-ye,DU Yu-jing. Semiquantitative parameters of 18F-FDG PET/CT, gene mutation states of epidermal growth factor receptor and anaplastic lymphoma kinase in prognosis evaluation of patients with lung adenocarcinoma [J]. Journal of Peking University (Health Sciences), 2021, 53(2): 246-254. |
| [6] | Yi BAO,Juan-fen MO. Concordant point mutation of ETS-related gene (ERG) in tumor tissues from a synchronous multiple primary lung cancer: A case report [J]. Journal of Peking University (Health Sciences), 2020, 52(5): 971-974. |
| [7] | Liang GENG,Jing LV,Jing FAN. Effect of Fei-Liu-Ping ointment combined with cyclophosphamide on lung cancer cell proliferation and acidic microenvironment [J]. Journal of Peking University (Health Sciences), 2020, 52(2): 247-253. |
| [8] | MEI Fang, ZHAO Ting-ting, GAO Fei, ZHENG Jie. A rare pulmonary benign bi-phasic tumor: a case report of pulmonary adenofibroma and literature review [J]. Journal of Peking University(Health Sciences), 2017, 49(6): 1076-1080. |
| [9] | MOU Qian-qian, YU Chun-hua, LI Jun-ying. Investigation and analysis for impact factors of distress in patients with first diagnosed lung can-cer [J]. Journal of Peking University(Health Sciences), 2016, 48(3): 507-514. |
| [10] | NI Lian-Fang, LIU Xin-Min. Diagnostic value of serum tumor markers in differentiating malignant from benign solitary pulmonary nodules [J]. Journal of Peking University(Health Sciences), 2014, 46(5): 707-710. |
| [11] | LI Yan, JIANG Liang, LIU Xiao-guang, LIU Zhong-jun, WEI Feng, WU Feng-liang, DANG Lei. Efficacy and survival rate analysis of lung cancer with spinal metastases [J]. Journal of Peking University(Health Sciences), 2014, 46(1): 138-143. |
| Viewed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
Full text 301
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|
Abstract 1138
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
Cited |
|
|||||||||||||||||||||||||||||||||||||||||||||||||
| Shared | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Discussed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
||