Journal of Peking University (Health Sciences) ›› 2022, Vol. 54 ›› Issue (6): 1117-1122. doi: 10.19723/j.issn.1671-167X.2022.06.010
Previous Articles Next Articles
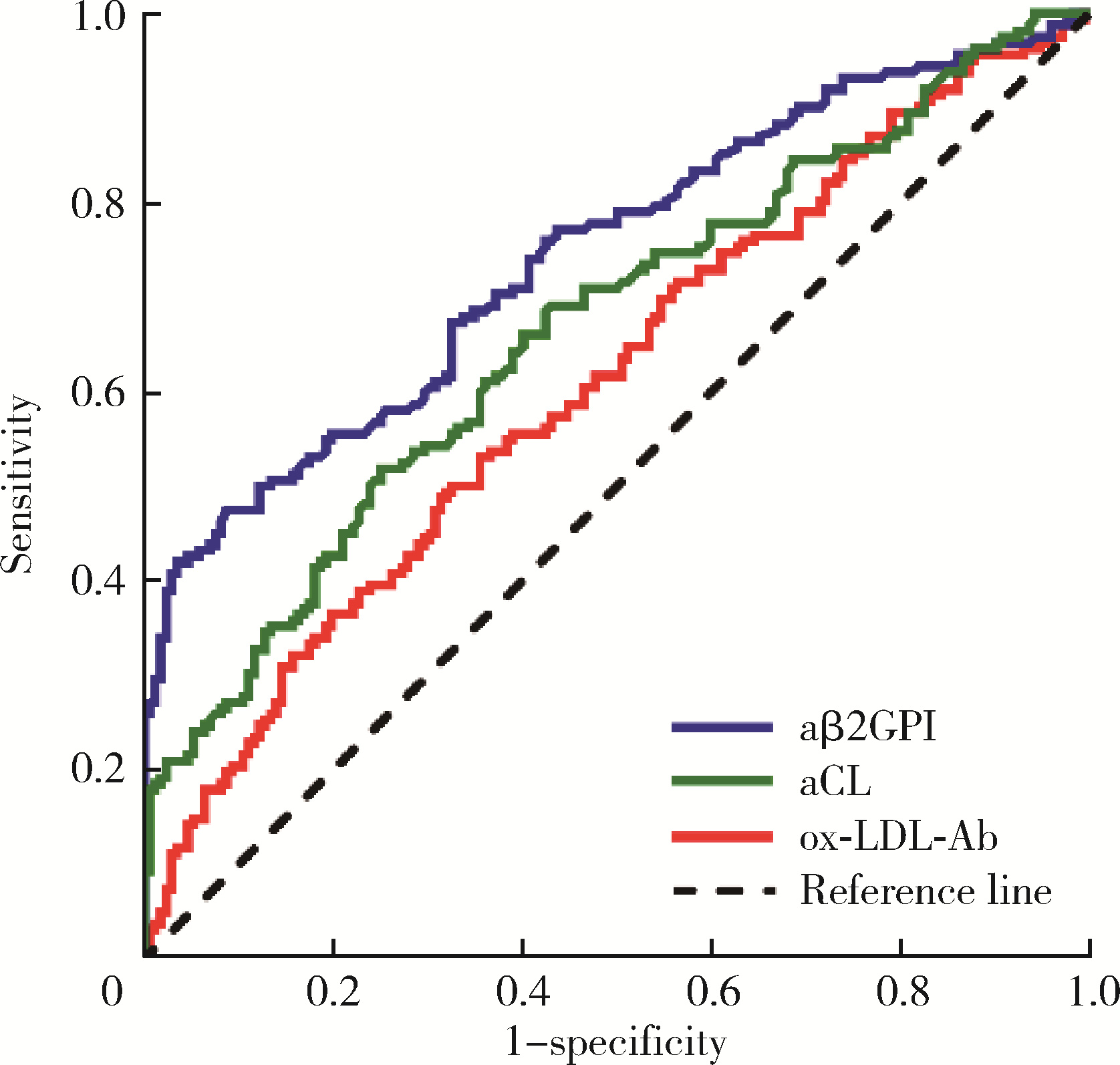
Clinical significance of oxidized low-density lipoprotein antibody in antiphospholipid syndrome
Yu-ke HOU,Qing-meng CAI,Xiang-jun LIU,Ze-lin YUN,Chun LI*( ),Xue-wu ZHANG*(
),Xue-wu ZHANG*( )
)
- Department of Rheumatology and Immunology, Peking University People's Hospital, Beijing 100044, China
CLC Number:
- R593.2
| 1 |
Devreese KMJ , Ortel TL , Pengo V , et al. Laboratory criteria for antiphospholipid syndrome: Communication from the SSC of the ISTH[J]. J Thromb Haemost, 2018, 16 (4): 809- 813.
doi: 10.1111/jth.13976 |
| 2 |
Conti F , Andreoli L , Crisafulli F , et al. Does seronegative obstetric APS exist? "pro" and "cons"[J]. Autoimmun Rev, 2019, 18 (12): 102407.
doi: 10.1016/j.autrev.2019.102407 |
| 3 |
Abreu MM , Danowski A , Wahl DG , et al. The relevance of "non-criteria" clinical manifestations of antiphospholipid syndrome: 14th International Congress on Antiphospholipid Anti-bodies Technical Task Force Report on Antiphospholipid Syndrome Clinical Features[J]. Autoimmun Rev, 2015, 14 (5): 401- 414.
doi: 10.1016/j.autrev.2015.01.002 |
| 4 | Hulthe J . Antibodies to oxidized LDL in atherosclerosis development: Clinical and animal studies[J]. Clin Chim Acta, 2004, 348 (1/2): 1- 8. |
| 5 |
Steinberg D . Low density lipoprotein oxidation and its pathobio-logical significance[J]. J Biol Chem, 1997, 272 (34): 20963- 20966.
doi: 10.1074/jbc.272.34.20963 |
| 6 |
Salonen JT , Ylä-Herttuala S , Yamamoto R , et al. Autoantibody against oxidised LDL and progression of carotid atherosclerosis[J]. Lancet, 1992, 339 (8798): 883- 887.
doi: 10.1016/0140-6736(92)90926-T |
| 7 |
Vaarala O . Antiphospholipid antibodies and atherosclerosis[J]. Lupus, 1996, 5 (5): 442- 447.
doi: 10.1177/096120339600500522 |
| 8 |
Ryan M , Owens D , Kilbride B , et al. Antibodies to oxidized lipoproteins and their relationship to myocardial infarction[J]. QJM, 1998, 91 (6): 411- 415.
doi: 10.1093/qjmed/91.6.411 |
| 9 |
Bellomo G , Maggi E , Poli M , et al. Autoantibodies against oxidatively modified low-density lipoproteins in NIDDM[J]. Diabetes, 1995, 44 (1): 60- 66.
doi: 10.2337/diab.44.1.60 |
| 10 | Lopez D , Kobayashi K , Merrill JT , et al. IgG autoantibodies against beta2-glycoprotein Ⅰ complexed with a lipid ligand derived from oxidized low-density lipoprotein are associated with arterial thrombosis in antiphospholipid syndrome[J]. Clin Dev Immunol, 2003, 10 (2/3/4): 203- 211. |
| 11 |
Romero FI , Amengual O , Atsumi T , et al. Arterial disease in lupus and secondary antiphospholipid syndrome: association with anti-beta2-glycoprotein Ⅰ antibodies but not with antibodies against oxidized low-density lipoprotein[J]. Br J Rheumatol, 1998, 37 (8): 883- 888.
doi: 10.1093/rheumatology/37.8.883 |
| 12 | Bec'arevic' M , Andrejevic' S , Miljic' P , et al. Serum lipids and anti-oxidized LDL antibodies in primary antiphospholipid syndrome[J]. Clin Exp Rheumatol, 2007, 25 (3): 361- 366. |
| 13 |
Miyakis S , Lockshin MD , Atsumi T , et al. International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS)[J]. J Thromb Haemost, 2006, 4 (2): 295- 306.
doi: 10.1111/j.1538-7836.2006.01753.x |
| 14 |
Rezende L , Couto NFD , Fernandes-Braga W , et al. OxLDL induces membrane structure rearrangement leading to biomechanics alteration and migration deficiency in macrophage[J]. Biochim Biophys Acta Biomembr, 2022, 1864 (9): 183951.
doi: 10.1016/j.bbamem.2022.183951 |
| 15 |
Hartley A , Haskard D , Khamis R . Oxidized LDL and anti-oxidized LDL antibodies in atherosclerosis: Novel insights and future directions in diagnosis and therapy[J]. Trends Cardiovasc Med, 2019, 29 (1): 22- 26.
doi: 10.1016/j.tcm.2018.05.010 |
| 16 |
Itakura H , Yokoyama M , Matsuzaki M , et al. Relationships between plasma fatty acid composition and coronary artery disease[J]. J Atheroscler Thromb, 2011, 18 (2): 99- 107.
doi: 10.5551/jat.5876 |
| 17 |
Yang SH , Li YT , Du DY . Oxidized low-density lipoprotein-induced CD147 expression and its inhibition by high-density lipoprotein on platelets in vitro[J]. Thromb Res, 2013, 132 (6): 702- 711.
doi: 10.1016/j.thromres.2013.10.003 |
| 18 |
Strobel NA , Fassett RG , Marsh SA , et al. Oxidative stress biomarkers as predictors of cardiovascular disease[J]. Int J Cardiol, 2011, 147 (2): 191- 201.
doi: 10.1016/j.ijcard.2010.08.008 |
| 19 |
Jiang D , Lim W , Crowther M , et al. A systematic review of the association between anti-beta-2 glycoprotein Ⅰ antibodies and APS manifestations[J]. Blood Adv, 2021, 5 (20): 3931- 3936.
doi: 10.1182/bloodadvances.2021005205 |
| 20 |
Hayem G , Nicaise-Roland P , Palazzo E , et al. Anti-oxidized low-density-lipoprotein (OxLDL) antibodies in systemic lupus erythematosus with and without antiphospholipid syndrome[J]. Lupus, 2001, 10 (5): 346- 351.
doi: 10.1191/096120301667475689 |
| 21 | Li J , Chi Y , Liu S , et al. Recombinant domain V of β2-glycoprotein Ⅰ inhibits the formation of atherogenic oxLDL/β2-glycoprotein Ⅰ complexes[J]. J Clin Immunol, 2014, 34 (6): 669- 676. |
| 22 | Matsuura E , Lopez LR . Autoimmune-mediated atherothrombosis[J]. Lupus, 2008, 17 (10): 878- 887. |
| 23 | 白玲, 谭雪峰, 刘平. 冠心病患者抗心磷脂抗体与PON、ox-LDL、MDA和SOD的相关性[J]. 心脏杂志, 2014, 26 (4): 453- 455. |
| [1] | Xiaofei TANG,Yonghong LI,Qiuling DING,Zhuo SUN,Yang ZHANG,Yumei WANG,Meiyi TIAN,Jian LIU. Incidence and risk factors of deep vein thrombosis in patients with rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 279-283. |
| [2] | Li-rong HONG,Yu-jia CHEN,Qing-lai JIANG,Ru-lin JIA,Chun LI,Liang-hua FENG. Predictive value of four items of new thrombus markers combined with conventional coagulation tests for thrombosis in antiphospholipid syndrome [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1033-1038. |
| [3] | Jin-man ZHUANG,Tian-run LI,Xuan LI,Jing-yuan LUAN,Chang-ming WANG,Qi-chen FENG,Jin-tao HAN. Application of Rotarex catheter system in femoropopliteal artery stenosis accompanied with thrombosis [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 328-332. |
| [4] | Rui LIU,Jin-xia ZHAO,Liang YAN. Clinical characteristics of patients with rheumatoid arthritis complicated with venous thrombosis of lower extremities [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1079-1085. |
| [5] | Yu-hua WANG,Guo-hua ZHANG,Ling-ling ZHANG,Jun-li LUO,Lan GAO. Adrenal hemorrhage in a patient with systemic lupus erythematosus [J]. Journal of Peking University(Health Sciences), 2019, 51(6): 1178-1181. |
| [6] | Jie-yu GU,Cui LU,Hui SHI,Cheng-de YANG. Case series and clinical analysis of 14 cases of catastrophic antiphospholipid syndrome [J]. Journal of Peking University(Health Sciences), 2018, 50(6): 1033-1038. |
| [7] | Ji LI,Li ZHENG,Lian-jie SHI,Jing XU,Jian-long SHU,Xue-wu ZHANG. Increased serum soluble-endoglin level and its clinical significance in antiphospholipid syndrome [J]. Journal of Peking University(Health Sciences), 2018, 50(6): 1027-1032. |
| [8] | ZHENG Xiao-Juan, DENG Xiao-Li, LIU Xiang-Yuan. Pregnancy outcome in 54 patients with antiphospholipid syndrome:a retrospective clinical study [J]. Journal of Peking University(Health Sciences), 2014, 46(2): 323-328. |
|
||