Journal of Peking University (Health Sciences) ›› 2022, Vol. 54 ›› Issue (6): 1163-1166. doi: 10.19723/j.issn.1671-167X.2022.06.017
Previous Articles Next Articles
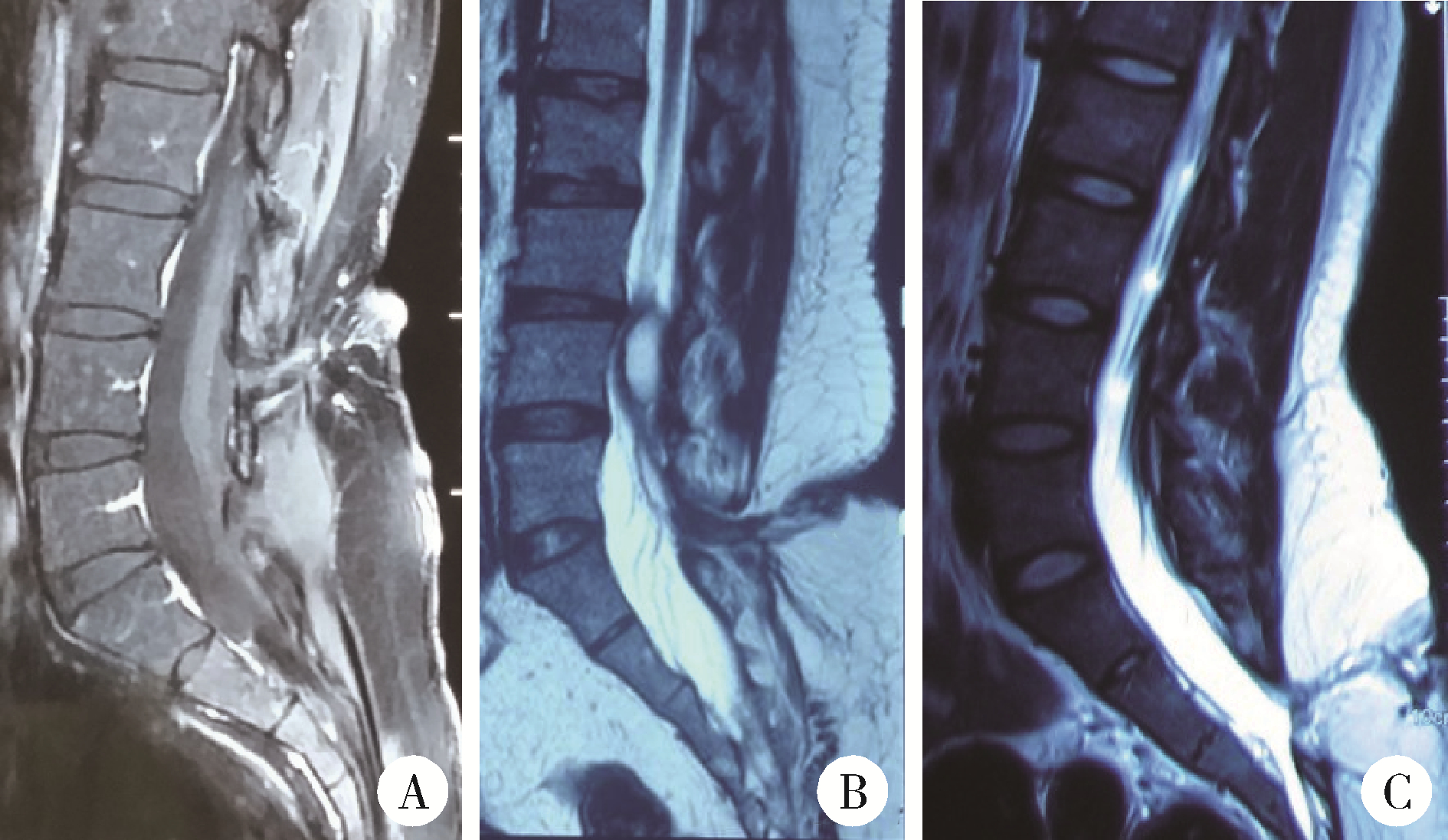
Diagnosis and surgical treatment of tethered cord syndrome accompanied by congenital dermal sinus tract in adults
Jing-cheng XIE*( ),Xiao-dong CHEN,Jun YANG
),Xiao-dong CHEN,Jun YANG
- Department of Neurosurgery, Peking University Third Hospital, Beijing 100191, China
CLC Number:
- R651.2
| 1 |
Kaufman BA . Neural tube defects[J]. Pediatr Clin North Am, 2004, 51 (2): 389- 419.
doi: 10.1016/S0031-3955(03)00207-4 |
| 2 |
Ackerman LL , Menezes AH . Spinal congenital dermal sinuses: A 30-year experience[J]. Pediatrics, 2003, 112 (3): 641- 647.
doi: 10.1542/peds.112.3.641 |
| 3 |
Gupta DK , Shastank RR , Mahapatra AK . An unusual presentation of lumbosacral dermal sinus with CSF leak and meningitis. A case report and review of the literature[J]. Pediatr Neurosurg, 2005, 41 (2): 98- 101.
doi: 10.1159/000085164 |
| 4 | Singh I , Rohilla S , Kumar P , et al. Spinal dorsal dermal sinus tract: An experience of 21 cases[J]. Surg Neurol Int, 2015, 6 (Suppl 17): S429- S434. |
| 5 |
王乐凯, 尚爱加, 乔广宇, 等. 先天性皮毛窦及其伴发神经管畸形的手术治疗[J]. 临床神经外科杂志, 2018, 15 (5): 362- 366.
doi: 10.3969/j.issn.1672-7770.2018.05.011 |
| 6 |
Hoffman HJ , Taecholarn C , Hendrick EB , et al. Management of lipomyelomeningoceles. Experience at the Hospital for Sick Children, Toronto[J]. J Neurosurg, 1985, 62 (1): 1- 8.
doi: 10.3171/jns.1985.62.1.0001 |
| 7 |
Kirollos RW , van Hille PT . Evaluation of surgery for the tethered cord syndrome using a new grading system[J]. Br J Neurosurg, 1996, 10 (3): 253- 260.
doi: 10.1080/02688699650040106 |
| 8 | Hukuda S , Mochizuki T , Ogata M , et al. Operations for cervical spondylotic myelopathy: A comparison of the results of anterior and posterior procedures[J]. J Bone Joint Surg (Br), 1985, 67 (4): 609- 615. |
| 9 |
Yamada S , Zinke DE , Sanders D . Pathophysiology of tethered cord syndrome[J]. J Neurosurg, 1981, 54 (4): 494- 498.
doi: 10.3171/jns.1981.54.4.0494 |
| 10 | Radmanesh F , Nejat F , Khashab ME . Dermal sinus tract of the spine[J]. Childs Nerv Syst, 2010, 26 (1): 349- 357. |
| 11 | Jindal A , Mahapatra AK . Spinal congenital dermal sinus: An experience of 23 cases over 7 years[J]. Neurol India, 2001, 49 (3): 243- 246. |
| 12 |
Mete M , Umur AS , Duransoy YK , et al. Congenital dermal sinus tract of the spine: experience of 16 patients[J]. J Child Neurol, 2014, 29 (10): 1277- 1282.
doi: 10.1177/0883073813520501 |
| 13 |
Tisdall MM , Hayward RD , Thompson DNP . Congenital spinal dermal tract: How accurate is clinical and radiological evaluation?[J]. J Neurosurg Pediatr, 15 (6): 651- 656.
doi: 10.3171/2014.11.PEDS14341 |
| 14 |
谢京城, 陈晓东, 杨军. 终丝牵张型脊髓拴系综合征的MRI分型及显微手术治疗的中长期效果[J]. 中国微创外科杂志, 2020, 20 (7): 577- 580.
doi: 10.3969/j.issn.1009-6604.2020.07.001 |
| 15 |
Hoving EW , Haitsma E , Oude-Ophuis CM , et al. The value of intraoperative neurophysiological monitoring in tethered cord surgery[J]. Childs Nerv Syst, 2011, 27 (9): 1445- 1452.
doi: 10.1007/s00381-011-1471-4 |
| [1] | Guo-zhong LIN,Jing-cheng XIE,Xiao-dong CHEN,Jun YANG. Classification and microsurgical treatment of primary tethered cord syndrome in adults [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 641-645. |
| [2] | YUAN Chang-wei,WANG Ying-jin,ZHANG Shu-jie,SHEN Sheng-li,DUAN Hong-zhou. Clinical outcomes following microsurgery and endovascular embolization in the management of spinal dural arteriovenous fistula: A meta-analysis study [J]. Journal of Peking University (Health Sciences), 2022, 54(2): 304-314. |
| [3] | LIN Guo-zhong, MA Chang-cheng, WANG Zhen-yu, XIE Jing-cheng, LIU Bin, CHEN Xiao-dong. Minimally invasive treatment of cervical1-2 epidural neurilemmoma [J]. Journal of Peking University (Health Sciences), 2021, 53(3): 586-589. |
| [4] | Guo-zhong LIN,Zhen-yu WANG,Jing-cheng XIE,Bin LIU,Chang-cheng MA,Xiao-dong CHEN. Clinical study of 21 cases of sacral cysts containing fila terminale [J]. Journal of Peking University (Health Sciences), 2020, 52(3): 582-585. |
| [5] | CHEN Li-hua, YANG Yi, WEI Qun, LI Yun-jun, LI Wen-de, GAO Jin-bao,YU Bin, ZHAO Hao, XU Ru-xiang. Microsurgical management of petroclival meningiomas combined trans-subtemporal and suboccipital retrosigmoid keyhole approach [J]. Journal of Peking University(Health Sciences), 2016, 48(4): 738-742. |
| [6] | DUAN Hong-Zhou, LI Liang, ZHANG Yang, ZHANG Jia-Yong, BAO Sheng-De. Surgical treatment of paraclinoid aneurysms [J]. Journal of Peking University(Health Sciences), 2015, 47(4): 679-684. |
| [7] | PENG Jing, LONG Hai, YUAN Yi-Ming, CUI Wan-Shou, ZHANG Zhi-Chao, PAN Wen-Bo. Comparison of the outcomes of microscopic varicocelectomy and laparoscopic varicocelectomy [J]. Journal of Peking University(Health Sciences), 2014, 46(4): 541-543. |
| Viewed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
Full text 169
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|
Abstract 577
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
Cited |
|
|||||||||||||||||||||||||||||||||||||||||||||||||
| Shared | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Discussed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
||