Journal of Peking University (Health Sciences) ›› 2026, Vol. 58 ›› Issue (1): 145-152. doi: 10.19723/j.issn.1671-167X.2026.01.019
Previous Articles Next Articles
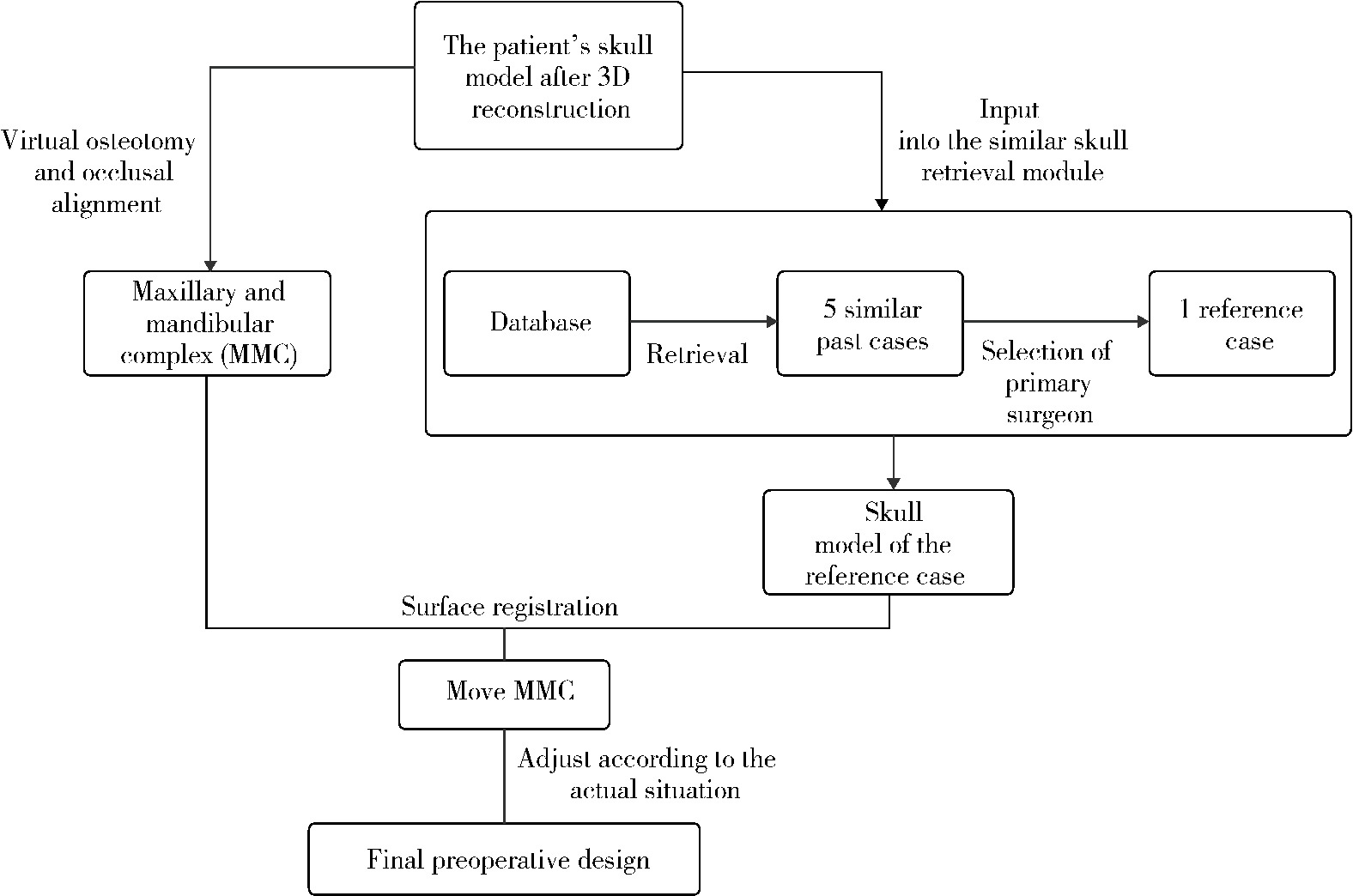
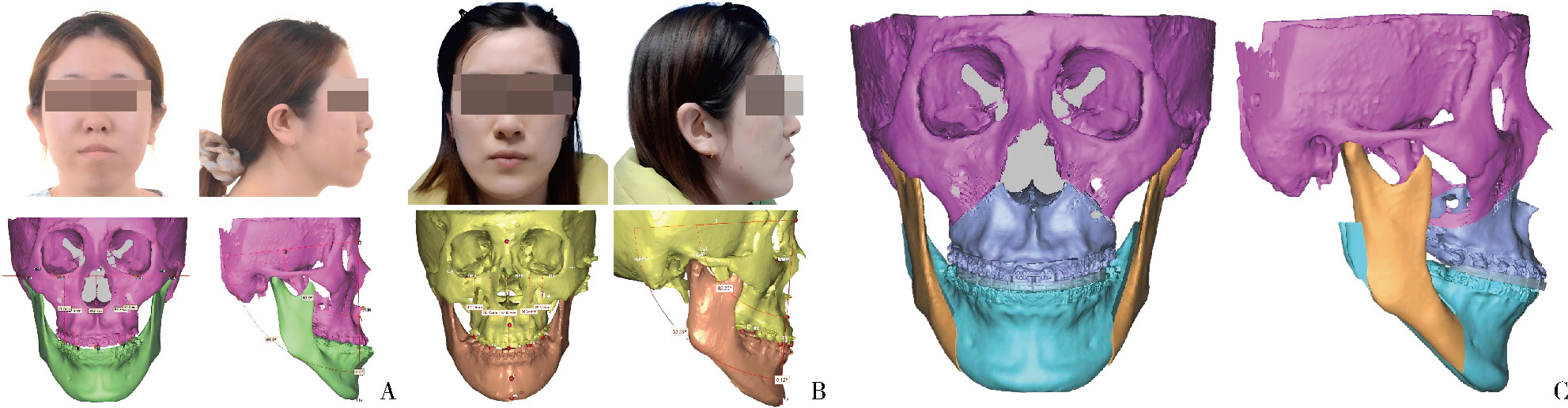
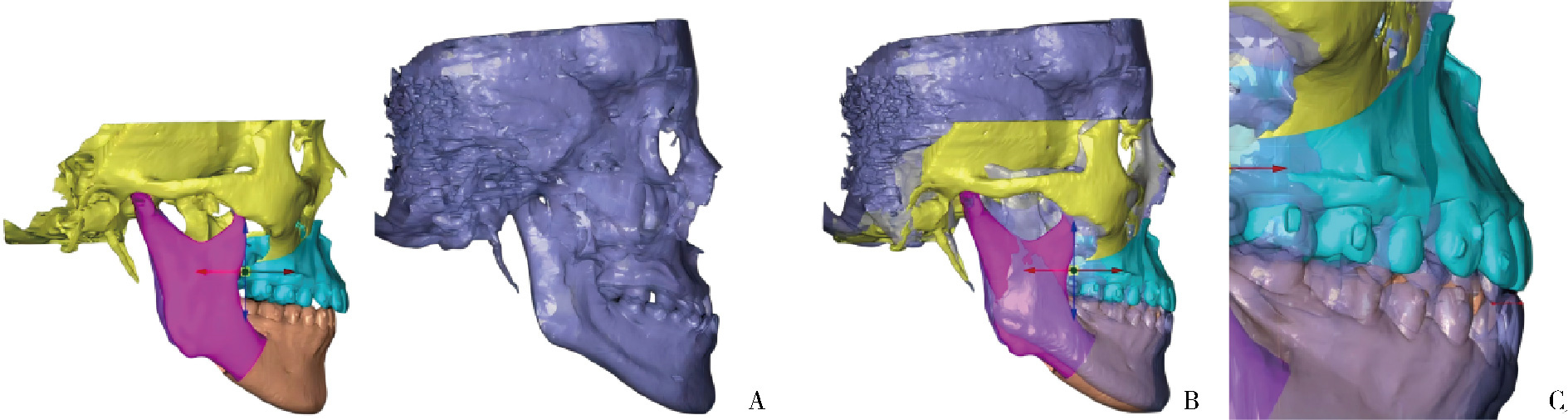
Feasibility study of a surgical planning protocol for orthognathic surgery utilizing similarity retrieval from database: A randomized controlled trial
Lu YU, Ling WU, Xiaojing LIU*( ), Zili LI*(
), Zili LI*( )
)
- Department of Oral and Maxillofacial Surgery, Peking University School and Hospital of Stomatology & National Center for Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Research Center of Oral Biomaterials and Digital Medical Devices, Beijing 100081, China
CLC Number:
- R782.2
| 1 |
|
| 2 |
doi: 10.1016/j.joms.2024.06.168 |
| 3 |
doi: 10.1007/s00784-018-2609-5 |
| 4 |
doi: 10.1016/j.jcms.2014.01.032 |
| 5 |
doi: 10.1007/s10006-012-0330-0 |
| 6 |
doi: 10.5927/jjjd1991.15.87 |
| 7 |
doi: 10.1016/S0278-2391(99)90481-0 |
| 8 |
doi: 10.1016/j.compbiomed.2025.110529 |
| 9 |
|
| 10 |
doi: 10.1007/s00056-021-00294-2 |
| 11 |
doi: 10.1186/s40902-021-00323-5 |
| 12 |
doi: 10.3390/bioengineering11070679 |
| 13 |
doi: 10.1016/j.ijom.2022.10.010 |
| 14 |
|
| 15 |
doi: 10.1002/ksa.12085 |
| 16 |
Deng HH, Wang L, Ren Y, et al. Patient-specific reference model for planning orthognathic surgery[M]//Machine learning in dentistry. Cham, Switzerland: Springer International Publishing, 2021: 105-114.
|
| 17 |
吴灵, 方嘉琨, 刘筱菁, 等. 基于牙颌面畸形患者三维颅面特征相似性度量模型的建立及评估[J]. 北京大学学报(医学版), 2025, 57 (1): 128- 135.
doi: 10.19723/j.issn.1671-167X.2025.01.019 |
| 18 |
doi: 10.1016/j.ijom.2019.04.003 |
| 19 |
doi: 10.1136/bmjoq-2021-001491 |
| 20 |
Luo Y. Study on personalized medical decision support system based on big data[C]//Proceedings of the 2024 4th International Conference on Bioinformatics and Intelligent Computing. Beijing, China: ACM, 2024: 293-296.
|
| [1] | Lijuan MA, Yonghui TENG, Yong WANG, Yijiao ZHAO, Xinyue ZHANG, Qingzhao QIN, Dong YIN. Three-dimensional finite element analysis of digital wire loop space maintainers for missing deciduous teeth [J]. Journal of Peking University (Health Sciences), 2025, 57(2): 376-383. |
| [2] | Ling WU, Jiakun FANG, Xiaojing LIU, Zili LI, Yang LI, Xiaoxia WANG. Establishment and evaluation of a similarity measurement model for orthognathic patients based on the 3D craniofacial features [J]. Journal of Peking University (Health Sciences), 2025, 57(1): 128-135. |
| [3] | Xinyu XU,Ling WU,Fengqi SONG,Zili LI,Yi ZHANG,Xiaojing LIU. Mandibular condyle localization in orthognathic surgery based on mandibular movement trajectory and its preliminary accuracy verification [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 57-65. |
| [4] | Sui LI,Wenjie MA,Shimin WANG,Qian DING,Yao SUN,Lei ZHANG. Trueness of different digital design methods for incisal guidance of maxillary anterior implant-supported single crowns [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 81-87. |
| [5] | FENG Sha-wei,GUO Hui,WANG Yong,ZHAO Yi-jiao,LIU He. Initial establishment of digital reference standardized crown models of the primary teeth [J]. Journal of Peking University (Health Sciences), 2022, 54(2): 327-334. |
| [6] | LI Yi,WONG Lai U,LIU Xiao-qiang,ZHOU Ti,LYU Ji-zhe,TAN Jian-guo. Marginal features of CAD/CAM laminate veneers with different materials and thicknesses [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 140-145. |
| [7] | QIU Shu-ting,ZHU Yu-jia,WANG Shi-min,WANG Fei-long,YE Hong-qiang,ZHAO Yi-jiao,LIU Yun-song,WANG Yong,ZHOU Yong-sheng. Preliminary clinical application verification of complete digital workflow of design lips symmetry reference plane based on posed smile [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 193-199. |
| [8] | XU Xiao-xiang,CAO Ye,ZHAO Yi-jiao,JIA Lu,XIE Qiu-fei. In vitro evaluation of the application of digital individual tooth tray in the impression making of mandibular full-arch crown abutments [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 54-61. |
| [9] | YUE Zhao-guo,ZHANG Hai-dong,YANG Jing-wen,HOU Jian-xia. Comparison of residual cement between CAD/CAM customized abutments and stock abutments via digital measurement in vitro [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 69-75. |
| [10] | LI Zheng,LIU Yu-shu,WANG Shi-min,ZHANG Rui,JIA Lu,YE Hong-qiang,HU Wen-jie,ZHAO Wen-yan,LIU Yun-song,ZHOU Yong-sheng. Application of biocopy function of temporary crown occlusal morphology in patients with severe attrition [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 62-68. |
| [11] | FANG Shuo-bo,YANG Guang-ju,KANG Yan-feng,SUN Yu-chun,XIE Qiu-fei. Method and accuracy of determining the jaw position of repositioning splint with the aid of digital technique [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 76-82. |
| [12] | Lang YOU,Ke-hui DENG,Wei-wei LI,Yi-jiao ZHAO,Yu-chun SUN,Yong-sheng ZHOU. Visual sensitivity threshold of lateral view of nasolabial Angle changes in edentulous jaw patients [J]. Journal of Peking University(Health Sciences), 2020, 52(1): 107-112. |
| [13] | Lei HOU,Guo-hua YE,Xiao-jing LIU,Zi-li LI. Evaluation of mandibular stability and condylar volume after orthognathic surgery in patients with severe temporomandibular joint osteoarthrosis [J]. Journal of Peking University(Health Sciences), 2020, 52(1): 113-118. |
| [14] | Xian-tao SUN,Wei HE,Xiao-jing LIU,Zi-li LI,Xing WANG. Feasibility of Delaire cephalometric analysis to predict the ideal sagittal position of the maxilla and chin for surgery-first patients in orthognathic surgery [J]. Journal of Peking University(Health Sciences), 2020, 52(1): 90-96. |
| [15] | Shuo CHEN,Yang HE,Jin-gang AN,Yi ZHANG. Application of computer-aided virtual mandibular position in the simultaneous treatment of children with temporomandibular joint ankylosis and jaw deformity [J]. Journal of Peking University(Health Sciences), 2019, 51(5): 954-958. |
|
||