Journal of Peking University(Health Sciences) ›› 2019, Vol. 51 ›› Issue (6): 1178-1181. doi: 10.19723/j.issn.1671-167X.2019.06.036
Previous Articles Next Articles
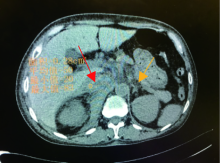
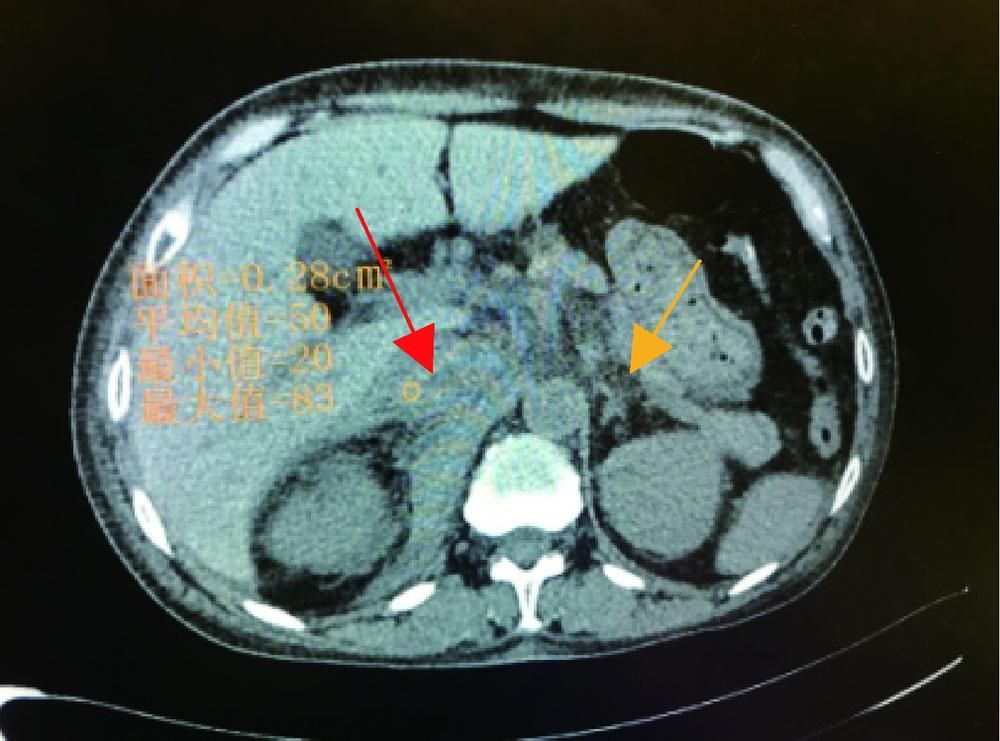
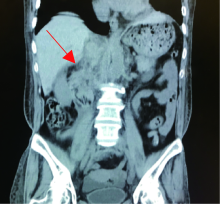
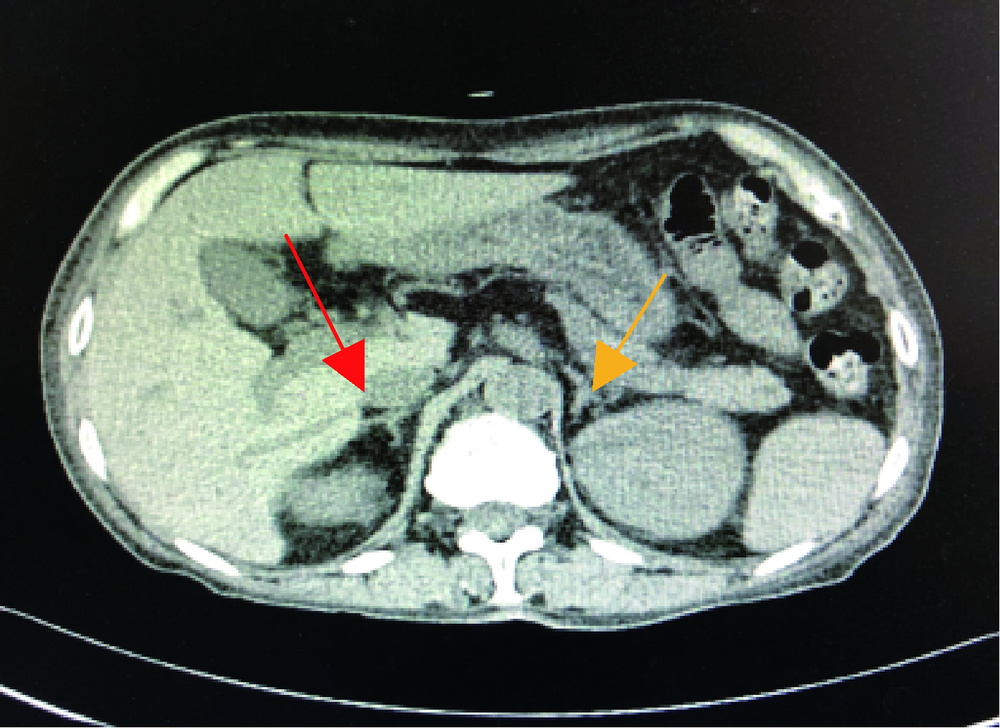
Adrenal hemorrhage in a patient with systemic lupus erythematosus
Yu-hua WANG( ),Guo-hua ZHANG,Ling-ling ZHANG,Jun-li LUO,Lan GAO
),Guo-hua ZHANG,Ling-ling ZHANG,Jun-li LUO,Lan GAO
- Department of Rheumatology, Beijing Shijitan Hospital, Capital Medical University, Beijing 100038, China
CLC Number:
- R593
| [1] | Presotto F, Fornasini F, Betterle C , et al. Acute adrenal failure as the heralding symptom of primary antiphospholipid syndrome:report of a case and review of the literature[J]. Eur J Endocrinol, 2005,153(4):507-514. |
| [2] | 张逸箫, 孔垂泽, 姜元军 . 肾上腺出血的诊断与治疗[J]. 国际外科学杂志, 2019,46(1):44-47. |
| [3] | Ruiz-Irastorza G, Cuadrado MJ, Ruiz-Arruza I , et al. Evidence-based recommendations for the prevention and long-term management of thrombosis in antiphospholipid antibody-positive patients:report of a task force at the 13th international congress on antiphospholipid antibodies[J]. Lupus, 2011,20(2):206-218. |
| [4] | 高辉, 姚海红, 安媛 , 等. 抗磷脂抗体综合征合并肾上腺血肿一例[J]. 中华风湿病学杂志, 2017,21(8):556-557. |
| [5] | Aldaajani H, Albahrani S, Saleh K , et al. Bilateral adrenal hemorrhage in antiphospholipid syndrome. Anticoagulation for the treatment of hemorrhage[J]. Saudi Med J, 2018,39(8):829-833. |
| [6] | Fukui S, Iwamoto N, Tsuji S , et al. Diffuse alveolar hemorrhage emerging one week after starting high-dose corticosteroid therapy for granulomatosis with polyangiitis (GPA) with systemic lupus erythematosus (SLE). Intern Med, 2015,54(20):2681-2686. |
| [7] | Xu J, Zhou Q, Jiang N , et al. Bilateral adrenal hemorrhage revealed antiphospholipid syndrome in a male patient: benefit from comprehensive treatment[J]. Curr Med Res Opin, 2018,34(12):2165-2168. |
| [8] | Abdulla MC, Alungal J, Hashim S . SLE presenting as multiple hemorrhagic complications[J]. Lupus, 2015,24(10):1103-1106. |
| [9] | Heller T, Bergholtz M, Martin F , et al. Bilateral adrenal hemorrhage occurring two times in primary antiphospholipid syndrome (APS). Anticoagulation as treatment of hemorrhage[J]. Dtsch Med Wochenschr, 2002,127(33):1695-1698. |
| [10] | Sanford Z, Nanjundappa A, Annie FH , et al. Adrenal hemorrhage in a patient anticoagulated with apixaban with antiphospholipid syndrome[J]. Cureus, 2019,11(7):e5108. |
| [1] | Li-rong HONG,Yu-jia CHEN,Qing-lai JIANG,Ru-lin JIA,Chun LI,Liang-hua FENG. Predictive value of four items of new thrombus markers combined with conventional coagulation tests for thrombosis in antiphospholipid syndrome [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1033-1038. |
| [2] | Yu-ke HOU,Qing-meng CAI,Xiang-jun LIU,Ze-lin YUN,Chun LI,Xue-wu ZHANG. Clinical significance of oxidized low-density lipoprotein antibody in antiphospholipid syndrome [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1117-1122. |
| [3] | Jie-yu GU,Cui LU,Hui SHI,Cheng-de YANG. Case series and clinical analysis of 14 cases of catastrophic antiphospholipid syndrome [J]. Journal of Peking University(Health Sciences), 2018, 50(6): 1033-1038. |
| [4] | Ji LI,Li ZHENG,Lian-jie SHI,Jing XU,Jian-long SHU,Xue-wu ZHANG. Increased serum soluble-endoglin level and its clinical significance in antiphospholipid syndrome [J]. Journal of Peking University(Health Sciences), 2018, 50(6): 1027-1032. |
| [5] | ZHENG Xiao-Juan, DENG Xiao-Li, LIU Xiang-Yuan. Pregnancy outcome in 54 patients with antiphospholipid syndrome:a retrospective clinical study [J]. Journal of Peking University(Health Sciences), 2014, 46(2): 323-328. |
|
||