Journal of Peking University (Health Sciences) ›› 2020, Vol. 52 ›› Issue (5): 863-869. doi: 10.19723/j.issn.1671-167X.2020.05.011
Previous Articles Next Articles
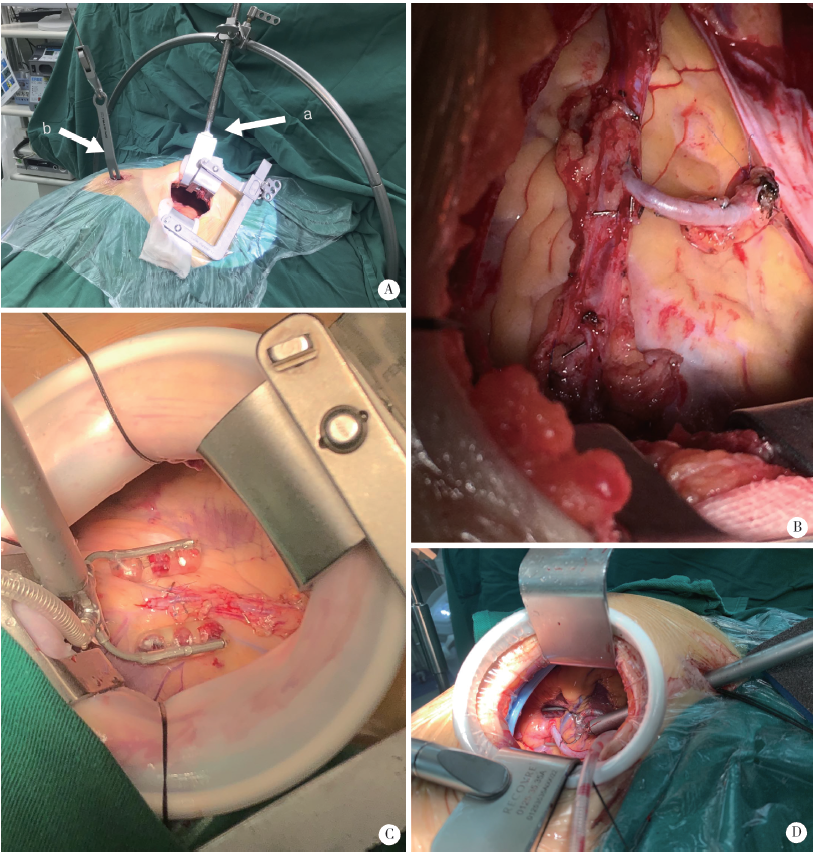
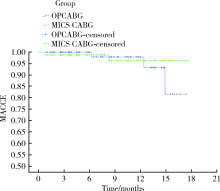
Feasibility and safety of minimally invasive cardiac coronary artery bypass grafting surgery for patients with multivessel coronary artery disease: Early outcome and short-mid-term follow up results
Zhi-feng XU1,2,Yun-peng LING2,∆( ),Zhong-qi CUI2,hong ZHAO2,Yi-chen GONG2,Yuan-hao FU2,Hang YANG2,Feng WAN2
),Zhong-qi CUI2,hong ZHAO2,Yi-chen GONG2,Yuan-hao FU2,Hang YANG2,Feng WAN2
- 1. Department of Cardiac Surgery, Peking University Shenzhen Hospital, Shenzhen 518036, Guangdong, China
2. Department of Cardiac Surgery, Peking University Third Hospital, Beijing 100191, China
CLC Number:
- R654
| [1] |
Yi G, Shine B, Rehman SM, et al. Effect of bilateral internal mammary artery grafts on long-term survival: a meta-analysis approach[J]. Circulation, 2014,130(7):539-545.
doi: 10.1161/CIRCULATIONAHA.113.004255 |
| [2] |
Ahn M, Park DW, Lee CW, et al. Comparison of stenting versus bypass surgery according to the completeness of revascularization in severe coronary artery disease: patient-level pooled analysis of the SYNTAX, PRECOMBAT, and BEST trials[J]. JACC Cardiovasc Interv, 2017,10(14):1415-1424.
doi: 10.1016/j.jcin.2017.04.037 pmid: 28728654 |
| [3] | 郑宝荣, 王联群, 刘建实, 等. 探讨Sino SCORE系统对非体外循环下冠状动脉旁路移植术风险评估的价值[J]. 中国循环杂志, 2013,28(5):375-378. |
| [4] |
Kikuchi K, Chen X, Mori M, et al. Perioperative outcomes of off-pump minimally invasive coronary artery bypass grafting with bilateral internal thoracic arteries under direct vision[J]. Interact Cardiovasc Thorac Surg, 2017,24(5):696-701.
doi: 10.1093/icvts/ivw431 pmid: 28329064 |
| [5] |
Nambiar P, Kumar S, Mittal CM, et al. Minimally invasive coronary artery bypass grafting with bilateral internal thoracic arteries: will this be the future[J]. J Thorac Cardiovasc Surg, 2017,155(1):190-197.
pmid: 29102209 |
| [6] | 张希涛, 高杰, 刘岩, 等. 腔镜获取大隐静脉在糖尿病患者心脏不停跳冠状动脉旁路移植术的应用[J]. 中华胸心血管外科杂志, 2016,32(3):159-161. |
| [7] |
Chan V, Lapierre H, Sohmer B, et al. Handsewn proximal anastomoses onto the ascending aorta through a small left thoracotomy during minimally invasive multivessel coronary artery bypass grafting: a stepwise approach to safety and reproducibility[J]. Semin Thorac Cardiov Surg, 2012,24(1):79-83.
doi: 10.1053/j.semtcvs.2011.12.010 |
| [8] | 杨威, 凌云鹏, 陈彧. 左胸前外侧小切口冠状动脉旁路移植术学习曲线[J]. 中国微创外科杂志, 2015,15(11):990-994. |
| [9] |
Dijk DV, Nierich AP, Jansen EWL, et al. Early outcome after off-pump vs. on-pump coronary bypass surgery results from a randomized study[J]. Circulation, 2001,104(15):1761-1766.
doi: 10.1161/hc4001.097036 pmid: 11591611 |
| [10] |
Kim YH, Oh HC, Choi JW, et al. No-touch saphenous vein harvesting may improve further the patency of saphenous vein com-posite grafts: early outcomes and 1-year angiographic results[J]. Ann Thorac Surg, 2017,103(5):1489-1497.
doi: 10.1016/j.athoracsur.2016.09.024 pmid: 27916241 |
| [11] | Kikuchi K, Une D, Suzuki K, et al. Off-pump minimally invasive coronary artery bypass grafting with a heart positioner: direct retraction for a better exposure[J]. Innovations, 2015,10(5):183-187. |
| [12] | Nambiar P, Mittal C. Minimally invasive coronary bypass using internal thoracic arteries via a left minithoracotomy: “the Nambiar Technique”[J]. Innovations, 2013,8(2):420-426. |
| [13] | 杨俊峰, 顾承雄, 韦华, 等. 非体外循环下双侧乳内动脉Y型桥的冠状动脉旁路移植术125例[J]. 中华外科杂志, 2006,44(22):1529-1531. |
| [14] | Glineur D, Etienne PY, Kuschner CE, et al. Bilateral internal mammary artery Y construct with multiple sequential grafting improves survival compared to bilateral internal mammary artery with additional vein grafts: 10-year experience at 2 different institutions[J]. Eur J Cardio-Thorac, 2017,51(2):368-375. |
| [15] |
Kikuchi K, Mori M. Less-invasive coronary artery bypass grafting international landscape and progress[J]. Curr Opin Cardiol, 2017,32(6):715-721.
doi: 10.1097/HCO.0000000000000461 pmid: 28858911 |
| [1] | Yun-peng CUI,Xue-dong SHI,Jia LIU,Chuan MI,Bing WANG,Yuan-xing PAN,Yun-fei LIN. Percutaneous pedicle screw fixation combined expandable tubular retractor in the treatment of spinal metastases [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 530-536. |
| [2] | LIN Guo-zhong,MA Chang-cheng,WU Chao,SI Yu. Microscopic resection of lumbar intraspinal tumor through keyhole approach: A clinical study of 54 cases [J]. Journal of Peking University (Health Sciences), 2022, 54(2): 315-319. |
| [3] | YUE Lei,WANG Yue-tian,BAI Chun-bi,CHEN Hao,FU Hao-yong,YU Zheng-rong,LI Chun-de,SUN Hao-lin. Analysis of surgical strategy of percutaneous endoscopic lumbar discectomy in young and middle-aged double-segment patients with lumbar disc herniation [J]. Journal of Peking University (Health Sciences), 2021, 53(4): 734-739. |
| [4] | Sheng-wei XIONG,Jie WANG,Wei-jie ZHU,Si-da CHENG,Lei ZHANG,Xue-song LI,Li-qun ZHOU. Advance in re-do pyeloplasty for the management of recurrent ureteropelvic junction obstruction after surgery [J]. Journal of Peking University (Health Sciences), 2020, 52(4): 794-798. |
| [5] | Duan YI,Wei ZHU,Xiu-li MENG,Xiao-guang LIU,Shui-qing LI,Bin ZHU,Dong-lin JIA. Analysis of anxiety, depression and related factors in patients with chronic lumbocrural pain before minimally invasive surgery [J]. Journal of Peking University (Health Sciences), 2020, 52(2): 285-289. |
| [6] | Ling-fu ZHANG,Chun-sheng HOU,Yong-hui HUANG,Zhi XU,Li-xin WANG,Xiao-feng LING,Gang WANG,Long CUI,Dian-rong XIU. Comparison of the minimally invasive treatments of laparoscopic and endosopic for common bile duct stones after gastrojejunostomy [J]. Journal of Peking University(Health Sciences), 2019, 51(2): 345-348. |
| [7] | Bing-chuan LIU,Zhong-wei YANG,Fang ZHOU,Hong-quan JI,Zhi-shan ZHANG,Yan GUO,Yun TIAN. Application of the modified internal fixation method of minimally invasive percuta-neous plate osteosynthesis in treatment of proximal humeral fracture [J]. Journal of Peking University(Health Sciences), 2019, 51(2): 277-282. |
| [8] | ZHANG Lu-feng, LING Yun-peng, YANG Hang, GONG Yi-chen, SONG Zhi-ming, WAN Feng. Comparison of outcomes of two minimally invasive approaches for multi-vessel coronary revascularization [J]. Journal of Peking University(Health Sciences), 2017, 49(6): 1066-1070. |
| [9] | ZHAO Li-ping, ZHAN Ya-lin, HU Wen-jie, WANG Hao-jie, WEI Yi-ping, ZHEN Min, Xu Tao, LIU Yun-song. Dental implantation and soft tissue augmentation after ridge preservation in a molar site: a case report [J]. Journal of Peking University(Health Sciences), 2016, 48(6): 1090-1094. |
| [10] | LIU Bo, CHEN Shan-lin, ZHU Jin, WANG Zhi-xin, YANG Chen, SHEN Jie, TIAN Guan-lei. Arthroscopic management of lesser arc perilunate injuries [J]. Journal of Peking University(Health Sciences), 2016, 48(2): 234-236. |
| [11] | HUANG Guang-Lin, MAN Li-Bo, WANG Hai, WANG Jian-Wei, DI Jian-Po, ZHU Xiao-Fei, ZHOU Ning, XU Xiao. Management of female urethral obliteration with the rotary excision appliance [J]. Journal of Peking University(Health Sciences), 2014, 46(4): 574-577. |
|
||