Journal of Peking University (Health Sciences) ›› 2021, Vol. 53 ›› Issue (5): 1002-1006. doi: 10.19723/j.issn.1671-167X.2021.05.032
Previous Articles Next Articles
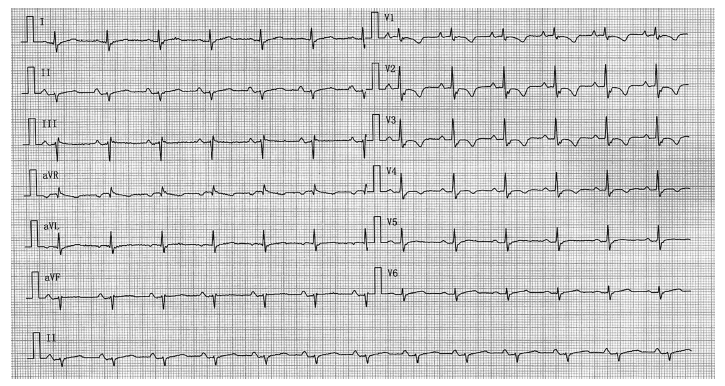
Arrhythmogenic right ventricular cardiomyopathy associated with arrhythmia-induced cardiomyopathy: A case report
CHEN Shao-min,SUN Chao( ),WANG Xin-yu,ZHANG Yuan,LIU Shu-wang
),WANG Xin-yu,ZHANG Yuan,LIU Shu-wang
- Beijing Key Laboratory of Cardiovascular Receptors Research, Beijing 100191, China
CLC Number:
- R541
| [1] |
Gandjbakhch E, Redheuil A, Pousset F, et al. Clinical diagnosis, imaging, and genetics of arrhythmogenic right ventricular cardiomyopathy/dysplasia: JACC state-of-the-art review [J]. J Am Coll Cardiol, 2018, 72(7):784-804.
doi: S0735-1097(18)35284-7 pmid: 30092956 |
| [2] | 中华医学会心血管病学分会精准心血管病学学组, 中国医疗保健国际交流促进会, 精准心血管病分会, 等. 单基因遗传性心血管疾病基因诊断指南 [J]. 中华心血管病杂志, 2019, 47(3):175-196. |
| [3] |
Marcus FI, McKenna WJ, Sherrill D, et al. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: Proposed modification of the task force criteria [J]. Circulation, 2010, 121(13):1533-1541.
doi: 10.1161/CIRCULATIONAHA.108.840827 |
| [4] |
Morimoto S, Sekiguchi M, Okada R, et al. Two autopsied cases of arrhythmogenic right ventricular dysplasia [J]. J Cardiol, 1990, 20(4):1025-1036.
pmid: 2133713 |
| [5] |
Vila J, Pariaut R, Moise NS, et al. Structural and molecular pathology of the atrium in boxer arrhythmogenic right ventricular cardiomyopathy [J]. J Vet Cardiol, 2017, 19(1):57-67.
doi: S1760-2734(16)30073-X pmid: 27769725 |
| [6] |
Wu L, Bao J, Liang E, et al. Atrial involvement in arrhythmo-genic right ventricular cardiomyopathy patients referred for ventri-cular arrhythmias ablation [J]. J Cardiovasc Electrophysiol, 2018, 29(10):1388-1395.
doi: 10.1111/jce.2018.29.issue-10 |
| [7] |
Cardona-Guarache R, Åström-Aneq M, Oesterle A, et al. Atrial arrhythmias in patients with arrhythmogenic right ventricular cardiomyopathy: Prevalence, echocardiographic predictors, and treatment [J]. J Cardiovasc Electrophysiol, 2019, 30(10):1801-1810.
doi: 10.1111/jce.v30.10 |
| [8] |
Saguner AM, Ganahl S, Kraus A, et al. Clinical role of atrial arrhythmias in patients with arrhythmogenic right ventricular dysplasia [J]. Circ J, 2014, 78(12):2854-2861.
pmid: 25327952 |
| [9] |
Camm CF, James CA, Tichnell C, et al. Prevalence of atrial arrhythmias in arrhythmogenic right ventricular dysplasia/cardio-myopathy [J]. Heart Rhythm, 2013, 10(11):1661-1668.
doi: 10.1016/j.hrthm.2013.08.032 |
| [10] |
Sugumar H, Prabhu S, Voskoboinik A, et al. Arrhythmia induced cardiomyopathy [J]. J Arrhythm, 2018, 34(4):376-383.
doi: 10.1002/joa3.2018.34.issue-4 |
| [11] | Corrado D, Wichter T, Link MS, et al. Treatment of arrhythmogenic right ventricular cardiomyopathy/dysplasia: An international task force consensus statement [J]. Eur Heart J, 2015, 36(46):3227-3237. |
| [12] |
Haugaa KH, Haland TF, Leren IS, et al. Arrhythmogenic right ventricular cardiomyopathy, clinical manifestations, and diagnosis [J]. Europace, 2016, 18(7):965-972.
doi: 10.1093/europace/euv340 |
| [1] | Yuanmei LIU, Yicheng FU, Jingxin HAO, Fuchun ZHANG, Huilin LIU. Construction and validation of a nomogram for predicting in-hospital postoperative heart failure in elderly patients with hip fracture [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 874-883. |
| [2] | Ying WEI,Ming CUI,Shuwang LIU,Haiyi YU,Wei GAO,Lei LI. Different levels and clinical significance of growth differentiation factor-15 in patients with atrial fibrillation [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 715-721. |
| [3] | Shengjia PENG,Yu QI,Lijie SUN,Dan LI,Xinyu WANG,Jiangli HAN,Baoxia CHEN,Yuan ZHANG. Afferent baroreflex failure with hyponatremia: A case report [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 357-361. |
| [4] | XU Hao,ZHANG Guo-dong,FAN Guang-pu,CHEN Yu. Preoperative plasma predictive factors of new-onset atrial fibrillation after coronary artery bypass graft surgery: A propensity score matching study [J]. Journal of Peking University (Health Sciences), 2021, 53(6): 1139-1143. |
| [5] | Huan LIU,Ying-dong HE,Jin-bo LIU,Wei HUANG,Na ZHAO,Hong-wei ZHAO,Xiao-hua ZHOU,Hong-yu WANG. Predictive value of vascular health indicators on newly cardiovascular events: Preliminary validation of Beijing vascular health stratification system [J]. Journal of Peking University (Health Sciences), 2020, 52(3): 514-520. |
| [6] | Chuan REN,Xiao-yue WU,Wei ZHAO,Li-yuan TAO,Ping LIU,Wei GAO. Protective effect of cardiopulmonary fitness on patients with high risk of atherosclerotic cardiovascular disease [J]. Journal of Peking University(Health Sciences), 2020, 52(1): 152-157. |
| [7] | Wen-qiang SUN,Zhou ZHAO,Qing GAO,Zeng-qiang HAN,Wei YANG,Bo LIAN,Gang LIU,Sheng-long CHEN,Yu CHEN. Effects of intraoperative graft flow measurements on the early mid-term outcomes after off-pump coronary artery bypass grafting [J]. Journal of Peking University(Health Sciences), 2019, 51(5): 851-855. |
| [8] | Jing ZHANG,Su-fang LI,Hong CHEN,Jun-xian SONG. Role of miR-106b-5p in the regulation of gene profiles in endothelial cells [J]. Journal of Peking University(Health Sciences), 2019, 51(2): 221-227. |
| [9] | ZHAO Can, HU Jing-Min, GUO Dan-Jie. Diagnostic value of D-dimer combined with Wells score for suspected pulmonary embolism [J]. Journal of Peking University(Health Sciences), 2018, 50(5): 828-832. |
| [10] | REN Shu-tang, WANG Yong, ZHOU Jian-hua, LONG Jin, WANG Cui-hua, LI Dong-bei, HUANG Yun-zhou. Echocardiographic diagnosis of infracardiac total anomalous pulmonary venous connection [J]. Journal of Peking University(Health Sciences), 0, (): 883-888. |
| [11] | REN Shu-tang, WANG Yong, ZHOU Jian-hua, LONG Jin, WANG Cui-hua, LI Dong-bei, HUANG Yun-zhou. Echocardiographic diagnosis of infracardiac total anomalous pulmonary venous connection [J]. Journal of Peking University(Health Sciences), 2017, 49(5): 883-888. |
| [12] | FENG Qi-chen, LI Xuan, LUAN Jing-yuan, WANG Chang-ming, LI Tian-run. Significance of renal filtration fraction evaluation of renal artery stenting for atherosclerotic renal artery stenosis treatment [J]. Journal of Peking University(Health Sciences), 2017, 49(1): 158-163. |
| [13] | LIU Teng-fei, ZHANG Jing-wei, CHEN Xia-huan, FENG Xue-ru, BAI Zhong-sheng, LIU Mei-lin. Association between CMTM5 gene rs723840 single nucleotide polymorphism and high on asprin platelet reactivity [J]. Journal of Peking University(Health Sciences), 2015, 47(6): 905-909. |
| [14] | LIU Teng-fei, ZHANG Jing-wei, CHEN Xia-huan, FENG Xue-ru, BAI Zhong-sheng, LIU Mei-lin. Correlation between the level of the urinary 11-dehydrothromboxane B2 and the clinical efficacy of aspirin in patients with type 2 diabete and coronary artery disease [J]. Journal of Peking University(Health Sciences), 2015, 47(6): 920-924. |
|
||