Journal of Peking University (Health Sciences) ›› 2021, Vol. 53 ›› Issue (5): 995-1001. doi: 10.19723/j.issn.1671-167X.2021.05.031
Previous Articles Next Articles
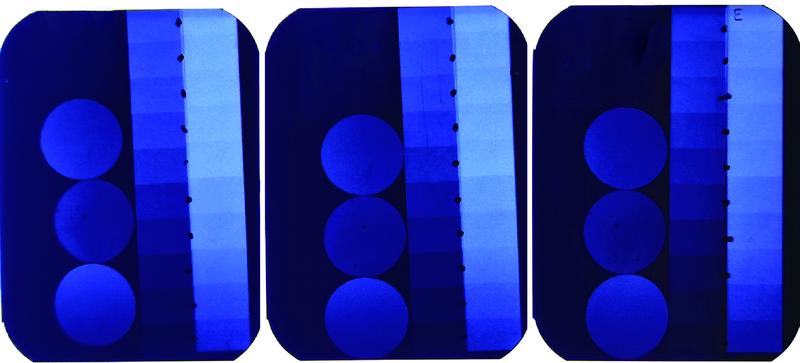
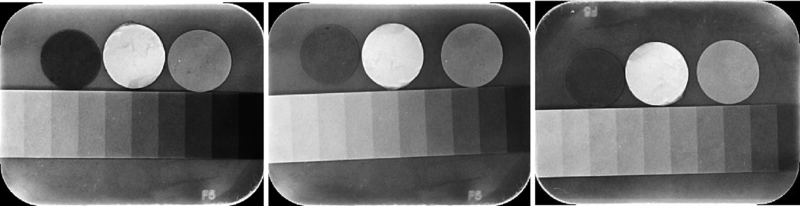
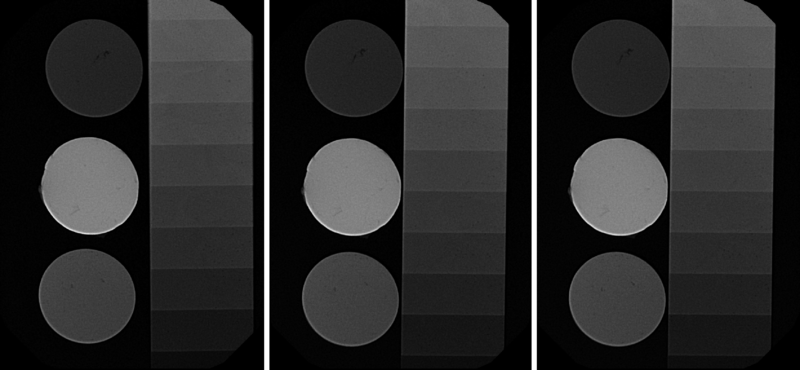
Comparative study on radio-opacity of dental composite resin materials’determination using film imaging and digital imaging
LI Yuan,LIN Hong( ),ZHANG Tie-jun
),ZHANG Tie-jun
- Department of Dental Materials & Dental Medical Devices Testing Center, Peking University School and Hospital of Stomatology & National Center of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & NMPA Key Laboratory for Dental Materials, Beijing 100081, China
CLC Number:
- R783.1
| [1] |
Poorterman JHG, Aartman IHA, Kalsbeek H. Underestimation of the prevalence of approximal caries and inadequate restorations in a clinical epidemiological study [J]. Community Dent Oral, 1999, 27(5):331-337.
pmid: 10503793 |
| [2] | Mjor IA. The location of clinically diagnosed secondary caries [J]. Quintessence Int, 1998, 29:313-317. |
| [3] |
Soares CJ, Rosatto CMP, Carvalho VF, et al. Radiopacity and porosity of bulk-fill and conventional composite posterior restorations-digital X-ray analysis [J]. Oper Dent, 2017, 42(6):616-625.
doi: 10.2341/16-146-L pmid: 28976845 |
| [4] |
Tarcin B, Gumru B, Peker S, et al. Evaluation of radiopacity of bulk-fill flowable composites using digital radiography [J]. Oper Dent, 2016, 41(4):424-431.
doi: 10.2341/15-153-L pmid: 27045286 |
| [5] |
Watts DC, McCabe JF. Aluminium radiopacity standards for dentistry: an international survey [J]. J Dent, 2006, 27(1):73-78.
doi: 10.1016/S0300-5712(98)00025-6 |
| [6] | 全国口腔材料和器械设备标准化技术委员会. 牙科学测定材料的X射线阻射性试验方法:YY/T 1646-2019 [S]. 北京: 中国标准出版社, 2019: 1. |
| [7] |
Gurdal P, Akdeniz BG. Comparison of two methods for radiometric evaluation of resin-based restorative materials [J]. Dentomaxillofac Radiol, 1998, 27(4):236-239.
doi: 10.1038/sj.dmfr.4600357 |
| [8] |
Hara AT, Serra MG, Rodrigues JA. Radiopacity of glass-ionomer composite resin hybrid materials [J]. Braz Dent J, 2001, 12(2):85-89.
pmid: 11445919 |
| [9] |
Tanomaru-Filho M, Jorge EG, Guerreiro TJ, et al. Radiopacity evaluation of new root canal filling materials by digitalization of images [J]. J Endod, 2007, 33(3):249-251.
doi: 10.1016/j.joen.2006.08.015 |
| [10] | 孙涛. DR成像技术的临床应用分析 [J]. 临床医药文献杂志, 2015, 2(8):1523. |
| [11] | 温建伟. CR与DR性能影像特点及其临床应用的比较研究 [J]. 中国继续医学教育, 2016, 8(14):53-54. |
| [12] | Arita ES, Silveira GP, Cortes AR, et al. Comparative study between the radiopacity levels of high viscosity and of flowable composite resins, using digital imaging [J]. Eur J Esthet Dent, 2012, 7(4):430-438. |
| [13] | Filling and restorative materials. ISO 4049: 2019 [S/OL]. [2021-04-13]. https://www.iso.org/obp/ui/#iso:std:iso:4049:ed-5:v1:en . |
| [14] |
Lachowski KM, Botta SB, Lascala CA, et al. Study of the radio-opacity of base and liner dental materials using a digital radiography system [J]. Dentomaxillofac Radiol, 2013, 42(2):20120153.
doi: 10.1259/dmfr.20120153 |
| [15] |
Rasimick BJ, Gu S, Deutsch AS, et al. Measuring the radiopacity of luting cements, dowels, and core build-up materials with a digital radiography system using a CCD sensor [J]. J Prosthodont, 2007, 16(5):357-364.
pmid: 17559533 |
| [16] |
Akcay I, Ilhan B, Dundar N. Comparison of conventional and digital radiography systems with regard to radiopacity of root canal filling materials [J]. Int Endod J, 2012, 45(8):730-736.
doi: 10.1111/j.1365-2591.2012.02026.x pmid: 22458866 |
| [17] |
R Kapila, Y Matsuda, K Araki, et al. Radiopacity measurement of restorative resins using film and three digital systems for comparison with ISO 4049 international standard [J]. Bull Tokyo Dent Coll, 2015, 56(4):207-214.
doi: 10.2209/tdcpublication.56.207 |
| [18] | 赵信义. 口腔材料学 [M]. 北京: 人民卫生出版社, 2020: 77. |
| [19] | 王亮亮. CR、DR系统的图像质量控制及影响因素 [J]. 黑龙江医药, 2017, 30(2):426-427. |
| [1] | Xinxin ZHAN,Lulu CAO,Dong XIANG,Hao TANG,Dandan XIA,Hong LIN. Effect of printing orientation on physical and mechanical properties of 3D printing prosthodontic base resin materials [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 345-351. |
| [2] | Si-ming ZHAO,Xiao-yan WANG. Influence of cavity design on quality of margin and marginal adaptation and microleakage of all-ceramic CAD/CAM inlays [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1105-1110. |
| [3] | Qian DING,Wen-jin LI,Feng-bo SUN,Jing-hua GU,Yuan-hua LIN,Lei ZHANG. Effects of surface treatment on the phase and fracture strength of yttria- and magnesia-stabilized zirconia implants [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 721-728. |
| [4] | Qian-mei ZHOU,Rui-yu DING,Li LI,Wei BAI,Jing-ying HU. Influence of paper mixing pads thickness on the compressive strength of glass ionomer cement [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 78-81. |
| [5] | Hao LUO,Fu-cong TIAN,Xiao-yan WANG. Surface roughness, gloss and sequential polishing times of various chairside computer aided design/manufacturing restorative materials [J]. Journal of Peking University (Health Sciences), 2022, 54(3): 565-571. |
| [6] | Yi DENG,Yi ZHANG,Bo-wen LI,Mei WANG,Lin TANG,Yu-hua LIU. Effects of different crosslinking treatments on the properties of decellularized small intestinal submucosa porous scaffolds [J]. Journal of Peking University (Health Sciences), 2022, 54(3): 557-564. |
| [7] | LI Yi,WONG Lai U,LIU Xiao-qiang,ZHOU Ti,LYU Ji-zhe,TAN Jian-guo. Marginal features of CAD/CAM laminate veneers with different materials and thicknesses [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 140-145. |
| [8] | YAN Wen-juan,ZHONG Jie,LIN Bi-chen,DING Mei-li,CHEN Xiao-xian. Application of cold flowable gutta-percha in root canal obturation after apexification [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 77-82. |
| [9] | MA Xin-rong,ZHU Xiao-ming,LI Jing,LI De-li,LI He-ping,TAN Jian-guo. Effect of a novel radio-frequency atmospheric-pressure glow discharge plasma jet treatment on crosslinking of dentin collagen [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 83-88. |
| [10] | WANG Li-xin , XU Xiao, NI Yao-feng, SUN Hai-tao, YU Ri-yue, WEI Shi-cheng. In vivo study of liposome-modified polyetheretherketone implant on bacteriostasis and osseointegration [J]. Journal of Peking University (Health Sciences), 2021, 53(4): 758-763. |
| [11] | YOU Peng-yue,LIU Yu-hua,WANG Xin-zhi,WANG Si-wen,TANG Lin. Biocompatibility and effect on bone formation of a native acellular porcine pericardium: Results of in vitro and in vivo [J]. Journal of Peking University (Health Sciences), 2021, 53(4): 776-784. |
| [12] | WANG Jing-qi,WANG Xiao. In vivo study of strontium-doped calcium phosphate cement for biological properties [J]. Journal of Peking University (Health Sciences), 2021, 53(2): 378-383. |
| [13] | MU Hai-li,TIAN Fu-cong,WANG Xiao-yan,GAO Xue-jun. Evaluation of wear property of Giomer and universal composite in vivo [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 120-125. |
| [14] | Wen-xin CHEN,Xu-dong BAO,Lin YUE. Curing method affecting the formation of oxygen inhibition layer on the surface of resin cement [J]. Journal of Peking University (Health Sciences), 2020, 52(6): 1117-1123. |
| [15] | Qiu-ju LI,Wei-yu GONG,Yan-mei DONG. Effect of bioactive glass pretreatment on the durability of dentin bonding interface [J]. Journal of Peking University (Health Sciences), 2020, 52(5): 931-937. |
|
||