Journal of Peking University (Health Sciences) ›› 2022, Vol. 54 ›› Issue (6): 1106-1111. doi: 10.19723/j.issn.1671-167X.2022.06.008
Previous Articles Next Articles
Clinical and immunological characteristics of systemic lupus erythematosus with retinopathy
Min LI1,Lin-qing HOU1,2,Yue-bo JIN1,Jing HE1,*( )
)
- 1. Department of Rheumatology and Immunology, Peking University People's Hospital, Bejing 100044, China
2. Department of Rheumatology and Immunology, The Third People's Hospital of Linfen, Linfen 041000, Shanxi, China
CLC Number:
- R593.24
| 1 |
Au A , O'Day J . Review of severe vaso-occlusive retinopathy in systemic lupus erythematosus and the antiphospholipid syndrome: Associations, visual outcomes, complications and treatment[J]. Clin Exp Ophthalmol, 2004, 32 (1): 87- 100.
doi: 10.1046/j.1442-9071.2004.00766.x |
| 2 |
Moulton VR , Suarez-Fueyo A , Meidan E , et al. Pathogenesis of human systemic lupus erythematosus: A cellular perspective[J]. Trends Mol Med, 2017, 23 (7): 615- 635.
doi: 10.1016/j.molmed.2017.05.006 |
| 3 |
Dammacco R , Procaccio P , Racanelli V , et al. Ocular involvement in systemic lupus erythematosus: The experience of two tertiary referral centers[J]. Ocul Immunol Inflamm, 2018, 26 (8): 1154- 1165.
doi: 10.1080/09273948.2018.1501495 |
| 4 |
Yen YC , Weng SF , Chen HA , et al. Risk of retinal vein occlusion in patients with systemic lupus erythematosus: A population-based cohort study[J]. Br J Ophthalmol, 2013, 97 (9): 1192- 1196.
doi: 10.1136/bjophthalmol-2013-303265 |
| 5 |
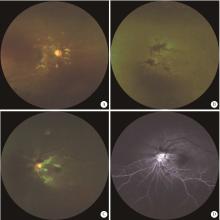
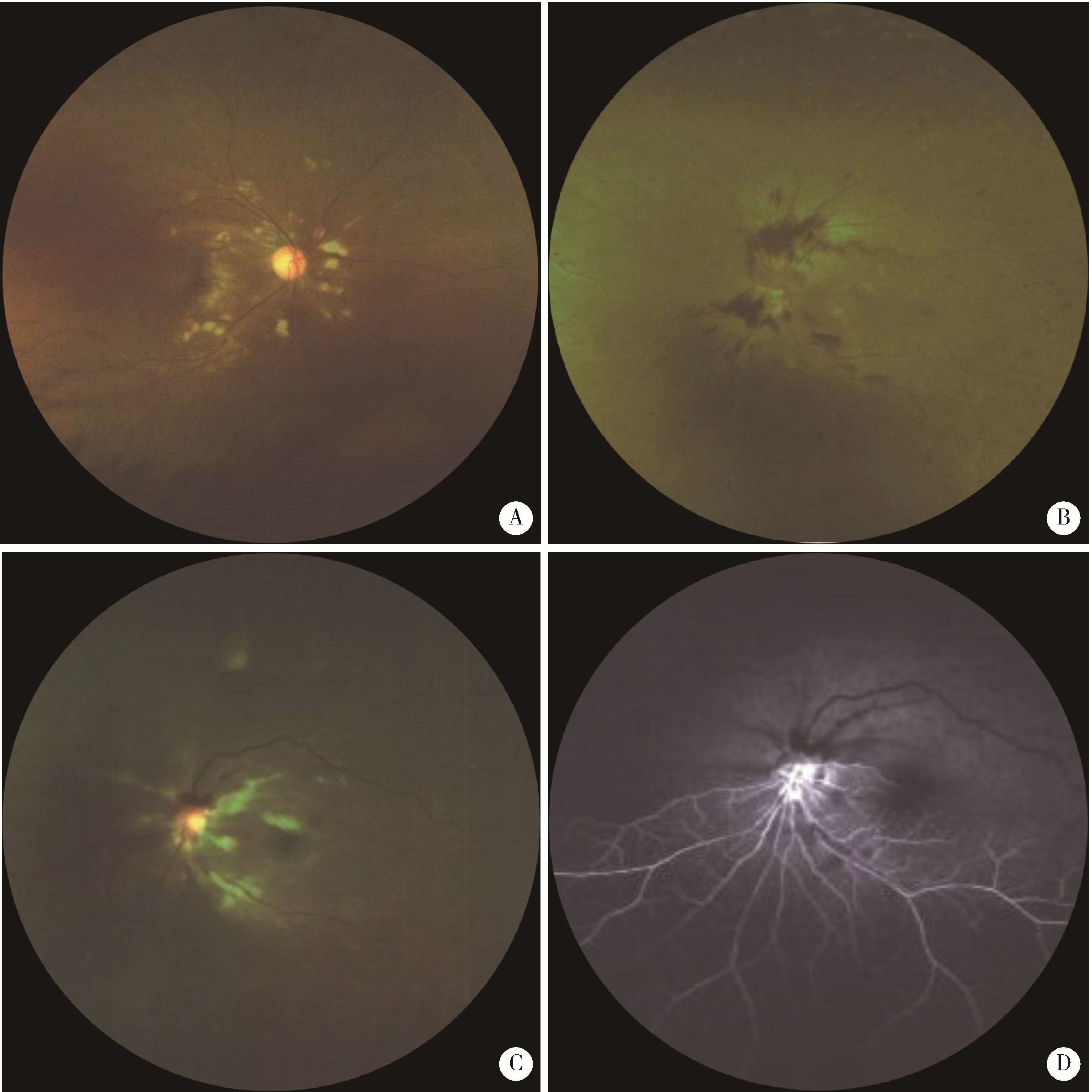
Lanham JG , Barrie T , Kohner EM , et al. SLE retinopathy: Evaluation by fluorescein angiography[J]. Ann Rheum Dis, 1982, 41 (5): 473- 478.
doi: 10.1136/ard.41.5.473 |
| 6 | Hochberg MC . Updating the American college of rheumatology revised criteria for the classification of systemic lupus erythematosus[J]. Arthritis Rheum, 1997, 40 (9): 1725. |
| 7 | Gladman DD , Ibanez D , Urowitz MB . Systemic lupus erythematosus disease activity index 2000[J]. J Rheumatol, 2002, 29 (2): 288- 291. |
| 8 |
Md Noh UK , Zahidin AZA , Yong TK . Retinal vasculitis in systemic lupus erythematosus: An indication of active disease[J]. Clinics and Practice, 2012, 2 (2): 54.
doi: 10.4081/cp.2012.e54 |
| 9 |
Stafford-Brady FJ , Urowitz MB , Gladman DD , et al. Lupus retinopathy. Patterns, associations, and prognosis[J]. Arthritis Rheum, 1988, 31 (9): 1105- 1110.
doi: 10.1002/art.1780310904 |
| 10 |
Giorgi D , Pace F , Giorgi A , et al. Retinopathy in systemic lupus erythematosus: Pathogenesis and approach to therapy[J]. Hum Immunol, 1999, 60 (8): 688- 696.
doi: 10.1016/S0198-8859(99)00035-X |
| 11 |
D'Cruz D . Vasculitis in systemic lupus erythematosus[J]. Lupus, 1998, 7 (4): 270- 274.
doi: 10.1191/096120398678920082 |
| 12 |
Kharel R , Shah DN , Singh D . Role of lupus retinopathy in systemic lupus erythematosus[J]. Ophthalmic Inflamm Infect, 2016, 6 (1): 1- 4.
doi: 10.1186/s12348-015-0068-6 |
| 13 |
Seth G , Chengappa KG , Misra DP , et al. Lupus retinopathy: A marker of active systemic lupus erythematosus[J]. Rheum Int, 2018, 38 (8): 1495- 1501.
doi: 10.1007/s00296-018-4083-4 |
| 14 |
曹绪胜, 纪海霞, 张永鹏, 等. 全身使用糖皮质激素继发中心性浆液性脉络膜视网膜病变的临床特征[J]. 眼科, 2020, 29 (3): 193- 197.
doi: 10.3969/j.issn.1006-8422.2020.03.001 |
| 15 |
Million M , Raoult D . The pathogenesis of the antiphospholipid syndrome[J]. N Engl J Med, 2013, 368 (24): 2335.
doi: 10.1056/NEJMc1300484 |
| 16 |
Jeon S , Lee WK . Aggravated capillary non-perfusion after intravitreal bevacizumab for macular edema secondary to systemic lupus erythematosus and anti-phospholipid syndrome[J]. Lupus, 2012, 21 (3): 335- 337.
doi: 10.1177/0961203311422095 |
| 17 | Zhu W , Wu Y , Xu M , et al. Correction: Antiphospholipid antibody and risk of retinal vein occlusion: A systematic review and meta-analysis[J]. PLoS One, 2016, 11 (6): e157536. |
| 18 |
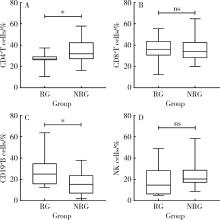
Lipsky PE . Systemic lupus erythematosus: An autoimmune disease of B cell hyperactivity[J]. Nat Immunol, 2001, 2 (9): 764- 766.
doi: 10.1038/ni0901-764 |
| 19 |
Wei C , Anolik J , Cappione A , et al. A new population of cells lacking expression of CD27 represents a notable component of the B cell memory compartment in systemic lupus erythematosus[J]. J Immunol, 2007, 178 (10): 6624- 6633.
doi: 10.4049/jimmunol.178.10.6624 |
| 20 |
Hickman RA , Denniston AK , Yee CS , et al. Bilateral retinal vasculitis in a patient with systemic lupus erythematosus and its remission with rituximab therapy[J]. Lupus, 2010, 19 (3): 327- 329.
doi: 10.1177/0961203309347332 |
| 21 |
Damato E , Chilov M , Lee R , et al. Plasma exchange and rituximab in the management of acute occlusive retinal vasculopathy secondary to systemic lupus erythematosus[J]. Ocul Immunol Inflamm, 2011, 19 (5): 379- 381.
doi: 10.3109/09273948.2011.603069 |
| 22 |
Tselios K , Lam WC , Urowitz MB , et al. Rituximab for sight-threatening lupus-related retinal vasculitis[J]. J Clin Rheumatol, 2018, 24 (2): 93- 94.
doi: 10.1097/RHU.0000000000000600 |
| 23 |
Liu M , Liu J , Zhang X , et al. Activation status of CD56(dim) natural killer cells is associated with disease activity of patients with systemic lupus erythematosus[J]. Clin Rheumatol, 2021, 40 (3): 1103- 1112.
doi: 10.1007/s10067-020-05306-x |
| [1] | Zhihui WU, Mingzhi HU, Qiaoying ZHAO, Fengfeng LV, Jingying ZHANG, Wei ZHANG, Yongfu WANG, Xiaolin SUN, Hui WANG. Immunomodulatory mechanism of umbilical cord mesenchymal stem cells modified by miR-125b-5p in systemic lupus erythematosus [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 860-867. |
| [2] | Limin REN,Chuchu ZHAO,Yi ZHAO,Huiqiong ZHOU,Liyun ZHANG,Youlian WANG,Lingxun SHEN,Wenqiang FAN,Yang LI,Xiaomei LI,Jibo WANG,Yongjing CHENG,Jiajing PENG,Xiaozhen ZHAO,Miao SHAO,Ru Li. Low disease activity and remission status of systemic lupus erythematosus in a real-world study [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 273-278. |
| [3] | Lu FENG,Jia-yu ZHAI,Jin-xia ZHAO. Medical visit status and clinical features in patients with IgG4 related disease [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1028-1032. |
| [4] | Zhi-jun LUO,Jia-jia WU,You SONG,Chun-li MEI,Rong DU. Systemic lupus erythematosus associated macrophage activation syndrome with neuropsychiatric symptoms: A report of 2 cases [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1111-1117. |
| [5] | Hai-hong YAO,Fan YANG,Su-mei TANG,Xia ZHANG,Jing HE,Yuan JIA. Clinical characteristics and diagnostic indicators of macrophage activation syndrome in patients with systemic lupus erythematosus and adult-onset Still's disease [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 966-974. |
| [6] | Xiang-ge ZHAO,Jia-qing LIU,Hui-na HUANG,Zhi-min LU,Zi-ran BAI,Xia LI,Jing-jing QI. Interferon-α mediating the functional damage of CD56dimCD57+natural killer cells in peripheral blood of systemic lupus erythematosuss [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 975-981. |
| [7] | Lin-qi ZHANG,Jing ZHAO,Hong-yan WANG,Zong-yi WANG,Ying-ni LI,Ji-yang TANG,Si-ying LI,Jin-feng QU,Ming-wei ZHAO. Relationship between anti-ENO1 antibody and systemic lupus erythematosus patients with retinopathy [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1099-1105. |
| [8] | Miao SHAO,Hui-fang GUO,Ling-yan LEI,Qing ZHAO,Yan-jie DING,Jin LIN,Rui WU,Feng YU,Yu-cui LI,Hua-li MIAO,Li-yun ZHANG,Yan DU,Rui-ying JIAO,Li-xia PANG,Li LONG,Zhan-guo LI,Ru LI. A multicenter study on the tolerance of intravenous low-dose cyclophosphamide in systemic lupus erythematosus [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1112-1116. |
| [9] | WEI Hui,Luo-zeng ##,Ci-dan-yang-zong ##,Bai-ma-yang-jin ##. Analysis of clinical characteristics of Henoch-Schonlein purpura patients from different altitudes in plateau areas [J]. Journal of Peking University (Health Sciences), 2021, 53(6): 1072-1077. |
| [10] | Jian-mei ZOU,Li-jun WU,Cai-nan LUO,Ya-mei SHI,Xue WU. Relationship of serum 25- hydroxy vitamin D and systemic lupus erythematosus [J]. Journal of Peking University (Health Sciences), 2021, 53(5): 938-941. |
| [11] | XIA Fang-fang,LU Fu-ai,LV Hui-min,YANG Guo-an,LIU Yuan. Clinical characteristics and related factors of systemic lupus erythematosus with interstitial pneumonia [J]. Journal of Peking University (Health Sciences), 2021, 53(2): 266-272. |
| [12] | ZHANG Qing-fen,ZHAO Hong,FENG Yi. Different anesthesia management in preterm infants undergoing surgeries for retinopathy of prematurity: A retrospective study [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 195-199. |
| [13] | Fang BAO,Wei-li SHI,Jing HU,Di ZHANG,Dong-han GAO,Yun-xia XIA,Hong-mei JING,Xiao-yan KE,Qing-gang GE,Ning SHEN. Analysis of the correlation between lymphocyte subsets and severity of corona virus disease 19 [J]. Journal of Peking University (Health Sciences), 2020, 52(6): 1075-1081. |
| [14] | Yan GENG,Bo-rui LI,Zhuo-li ZHANG. Musculoskeletal ultrasound findings of symptomatic joints in patients with systemic lupus erythematosus [J]. Journal of Peking University(Health Sciences), 2020, 52(1): 163-168. |
| [15] | Yu-hua WANG,Guo-hua ZHANG,Ling-ling ZHANG,Jun-li LUO,Lan GAO. Adrenal hemorrhage in a patient with systemic lupus erythematosus [J]. Journal of Peking University(Health Sciences), 2019, 51(6): 1178-1181. |
|
||