Journal of Peking University (Health Sciences) ›› 2025, Vol. 57 ›› Issue (4): 748-752. doi: 10.19723/j.issn.1671-167X.2025.04.019
Previous Articles Next Articles
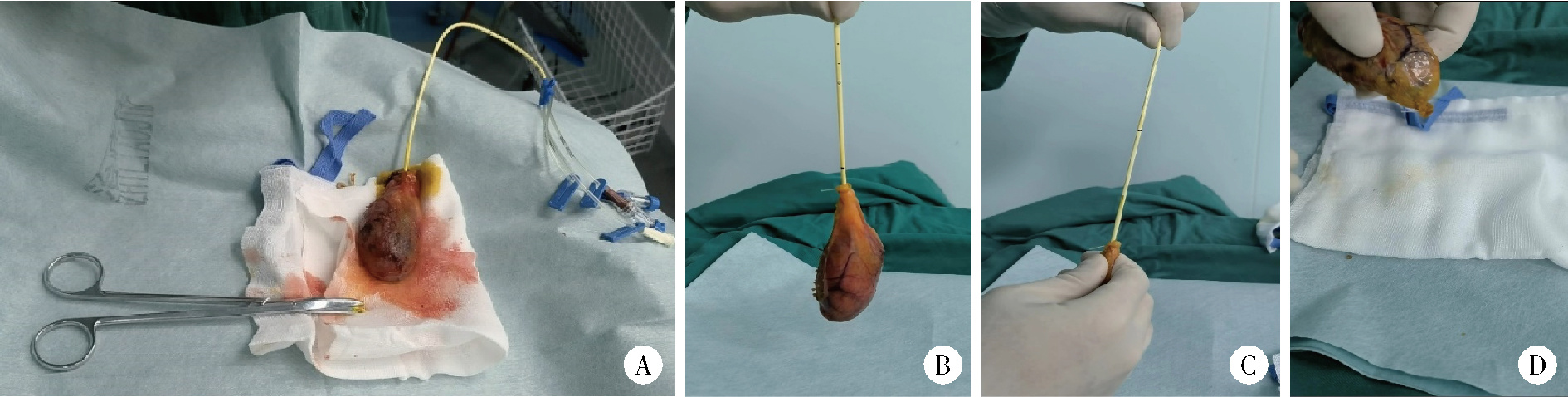
Laparoscopic modified transcystic biliary drainage for the treatment of biliary stones and diagnosis of biliary disease
Lingfu ZHANG, Gang WANG, Chunsheng HOU*( ), Long CUI, Lixin WANG, Xiaofeng LING, Zhi XU
), Long CUI, Lixin WANG, Xiaofeng LING, Zhi XU
- Department of General Surgery, Peking University Third Hospital, Beijing 100191, China
CLC Number:
- R657.4
| 1 |
管辉球, 景岚, 徐锁青. 胆总管一期缝合经胆囊管胆管引流与鼻胆管引流的对比研究[J]. 中华外科杂志, 2018, 56 (2): 130- 134.
|
| 2 |
|
| 3 |
张铃福, 侯纯升, 徐智, 等. 腹腔镜下经胆囊管胆管引流联合胆总管探查取石术治疗复杂胆管结石的临床效果[J]. 北京大学学报(医学版), 2022, 54 (6): 1185- 1189.
doi: 10.19723/j.issn.1671-167X.2022.06.021 |
| 4 |
张铃福, 辛春艳, 王立新, 等. 腹腔镜改进C管技术联合术后十二指肠镜下取石治疗急诊胆囊结石合并胆总管结石[J]. 中国微创外科杂志, 2023, 23 (4): 294- 297.
|
| 5 |
|
| 6 |
|
| 7 |
|
| 8 |
|
| [1] | Huanrui WANG, Shicong LAI, Haopu HU, Zehua DING, Tao XU, Hao HU. Efficacy analysis of laparoscopy combined with flexible ureteroscope in the treatment of complex ureteral stricture [J]. Journal of Peking University (Health Sciences), 2025, 57(4): 784-788. |
| [2] | Min QIU,You-long ZONG,Bin-shuai WANG,Bin YANG,Chu-xiao XU,Zheng-hui SUN,Min LU,Lei ZHAO,Jian LU,Cheng LIU,Xiao-jun TIAN,Lu-lin MA. Treatment outcome of laparoscopic partial nephrectomy in patients with renal tumors of moderate to high complexity [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 833-837. |
| [3] | Hui-li LIU,Yan-han LV,Xiao-xiao WANG,Min LI. Factors influencing the chronic post-surgical pain after laparoscopic surgery for elderly patients with urinary tract tumors [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 851-856. |
| [4] | Ling-fu ZHANG,Chun-sheng HOU,Zhi XU,Li-xin WANG,Xiao-feng LING,Gang WANG,Long CUI,Dian-rong XIU. Clinical effect of laparoscopic transcystic drainage combined with common bile duct exploration for the patients with difficult biliary stones [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1185-1189. |
| [5] | Li-zhe AN,Liu-lin XIONG,Liang CHEN,Huan-rui WANG,Wei-nan CHEN,Xiao-bo HUANG. Laparoscopic pyeloplasty combined with ultrasonic lithotripsy via nephroscope for treatment of ureteropelvic junction obstruction with renal calculi [J]. Journal of Peking University (Health Sciences), 2022, 54(4): 746-750. |
| [6] | ZHANG Fan,CHEN Qu,HAO Yi-chang,YAN Ye,LIU Cheng,HUANG Yi,MA Lu-lin. Relationship between recovery of urinary continence after laparoscopic radical prostatectomy and preoperative/postoperative membranous urethral length [J]. Journal of Peking University (Health Sciences), 2022, 54(2): 299-303. |
| [7] | ZHANG Fan,HUANG Xiao-juan,YANG Bin,YAN Ye,LIU Cheng,ZHANG Shu-dong,HUANG Yi,MA Lu-lin. Relationship between prostate apex depth and early recovery of urinary continence after laparoscopic radical prostatectomy [J]. Journal of Peking University (Health Sciences), 2021, 53(4): 692-696. |
| [8] | Bing-wei HUANG,Jie WANG,Peng ZHANG,Zhe LI,Si-cheng BI,Qiang WANG,Cai-bo YUE,Kun-lin YANG,Xue-song LI,Li-qun ZHOU. Application of indocyanine green in complex upper urinary tract repair surgery [J]. Journal of Peking University (Health Sciences), 2020, 52(4): 651-656. |
| [9] | Shu-dong ZHANG,Peng HONG,Bin-shuai WANG,Shao-hui DENG,Fan ZHANG,Li-yuan TAO,Cai-guang CAO,Zhen-hua HU,Lu-lin MA. Usefulness of the indocyanine green fluorescence imaging technique in laparoscopic partial nephrectomy [J]. Journal of Peking University (Health Sciences), 2020, 52(4): 657-662. |
| [10] | Si-da CHENG,Xin-fei LI,Sheng-wei XIONG,Shu-bo FAN,Jie WANG,Wei-jie ZHU,Zi-ao LI,Guang-pu DING,Ting YU,Wan-qiang LI,Yong-ming SUN,Kun-lin YANG,Lei ZHANG,Han HAO,Xue-song LI,Li-qun ZHOU. Robot-assisted laparoscopic upper urinary tract reconstruction surgery: A review of 108 cases by a single surgeon [J]. Journal of Peking University (Health Sciences), 2020, 52(4): 771-779. |
| [11] | Hai-wen HUANG,Bing YAN,Mei-xia SHANG,Li-bo LIU,Han HAO,Zhi-jun XI. Propensity-matched comparison of laparoscopic and open radical cystectomy for female patients with bladder cancer [J]. Journal of Peking University(Health Sciences), 2019, 51(4): 698-705. |
| [12] | Hai-yue ZHAO,Xiong-jun YE,Wei-nan CHEN,Li-zhe AN,Jun LIU,Liu-lin XIONG,Xiao-bo HUANG. Treatment of crossing vessels in laparoscopic pyeloplasty [J]. Journal of Peking University(Health Sciences), 2019, 51(4): 660-664. |
| [13] | Si-da CHENG,Wan-qiang LI,Li MU,Guang-pu DING,Bo ZHANG,Cheng SHEN,Ze-wei YING,Kun-lin YANG,Han HAO,Xue-song LI,Li-qun ZHOU. Application of totally extraperitoneal renal autotransplantation with Boari flap-pelvis anastomosis in upper urinary tract urothelial carcinomas treatment [J]. Journal of Peking University(Health Sciences), 2019, 51(4): 758-763. |
| [14] | Ling-fu ZHANG,Chun-sheng HOU,Yong-hui HUANG,Zhi XU,Li-xin WANG,Xiao-feng LING,Gang WANG,Long CUI,Dian-rong XIU. Comparison of the minimally invasive treatments of laparoscopic and endosopic for common bile duct stones after gastrojejunostomy [J]. Journal of Peking University(Health Sciences), 2019, 51(2): 345-348. |
| [15] | Xiao-jun TIAN,Min QIU,Zhuo LIU,Ruo-tao XIAO,Yi HUANG,Guo-liang WANG,Xiao-fei HOU,Shu-dong ZHANG,Shen-rong ZHUANG,Lu-lin MA. Single-center study of laparoscopic radical nephrectomy with Mayo 0-2 level inferior vena cava thrombectomy [J]. Journal of Peking University(Health Sciences), 2018, 50(6): 1053-1056. |
|
||