Journal of Peking University(Health Sciences) ›› 2019, Vol. 51 ›› Issue (1): 53-58. doi: 10.19723/j.issn.1671-167X.2019.01.010
Previous Articles Next Articles
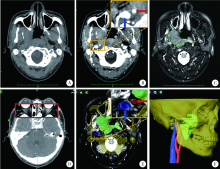
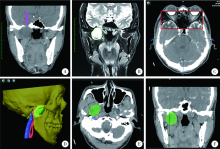
Multimodal image fusion technology for diagnosis and treatment of the skull base-infratemporal tumors
Rong YANG,Qing-xiang LI,Chi MAO,Xin PENG,Yang WANG,Yu-xing GUO( ),Chuan-bin GUO(
),Chuan-bin GUO( )
)
- Department of Oral and Maxillofacial Surgery, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
CLC Number:
- R78
| [1] |
Choudhri AF, Parmar HA, Morales RE , et al. Lesions of the skull base: imaging for diagnosis and treatment[J]. Otolaryngol Clin North Am, 2012,45(6):1385-1404.
doi: 10.1007/978-3-642-35579-0_20 |
| [2] | 魏宏权 . 咽旁隙和颞下窝肿瘤的外科治疗进展[J]. 中国耳鼻咽喉颅底外科杂志, 2018,24(2):91-96, 102. |
| [3] |
郭玉兴, 彭歆, 刘筱菁 , 等. 导航技术在颅底-颞下区肿瘤手术中的应用[J]. 中华口腔医学杂志, 2013,48(11):645-647.
doi: 10.3760/cma.j.issn.1002-0098.2013.11.002 |
| [4] |
郭传瑸, 郭玉兴 . 外科导航技术引导的颅底肿瘤穿刺活检[J]. 中国实用口腔科杂志, 2014,7(6):321-324.
doi: 10.7504/kq.2014.06.001 |
| [5] |
Guo R, Guo YX, Feng Z , et al. Application of a computer-aided navigation technique in surgery for recurrent malignant infratemporal fossa tumors[J]. J Craniofac Surg, 2015,26(2):e126-132.
doi: 10.1097/SCS.0000000000001350 pmid: 25710743 |
| [6] |
Leong JL, Batra PS, Citardi MJ . CT-MR image fusion for the management of skull base lesions[J]. Otolaryngol Head Neck Surg, 2006,134(5):868-876.
doi: 10.1016/j.otohns.2005.11.015 pmid: 16647550 |
| [7] |
Guo Y, Guo C . Maxillary-fronto-temporal approach for removal of recurrent malignant infratemporal fossa tumors: Anatomical and clinical study[J]. J Craniomaxillofac Surg, 2014,42(3):206-212.
doi: 10.1016/j.jcms.2013.05.001 pmid: 23932542 |
| [8] |
Yacoub A, Anschuetz L, Schneider D , et al. Minimally invasive lateral endoscopic multiport approach to the infratemporal fossa: a cadaveric study[J]. World Neurosurg, 2018,112:e489-e496.
doi: 10.1016/j.wneu.2018.01.065 pmid: 29391297 |
| [9] | 李成才, 姚国杰, 杜威 , 等. 多模态影像融合在颅底肿瘤的诊断、治疗中的应用价值[J]. 中国临床神经外科杂志, 2018,23(3):145-148. |
| [10] |
O'Neill BE, Hochhalter CB, Carr C , et al.Advances in neuro-oncology imaging techniques[J]. Ochsner J, 2018,18(3):236-241.
doi: 10.31486/toj.17.0062 |
| [11] |
赵岩, 孙健, 杨学军 . 多模态影像融合技术在神经外科的应用及进展[J]. 中国现代神经疾病杂志, 2012,12(6):645-650.
doi: 10.3969/j.issn.1672-6731.2012.06.004 |
| [12] |
顾恒乐, 聂生东 . 多模医学图像配准和融合方法及其临床应用进展[J]. 中华放射肿瘤学杂志, 2016,25(8):902-906.
doi: 10.3760/cma.j.issn.1004-4221.2016.08.024 |
| [13] |
Inoue HK, Nakajima A, Sato H , et al. Image fusion for radiosurgery, neurosurgery and hypofractionated radiotherapy[J]. Cureus, 2015,7(3):e252.
doi: 10.7759/cureus.252 pmid: 26180676 |
| [14] |
Nemec SF, Donat MA, Mehrain S , et al. Ct-mr image data fusion for computer assisted navigated neurosurgery of temporal bone tumors[J]. Eur J Radiol, 2007,62(2):192-198.
doi: 10.1016/j.ejrad.2006.11.029 pmid: 17229539 |
| [15] |
Zhang SX, Han PH, Zhang GQ , et al. Comparison of spect/ct, mri and ct in diagnosis of skull base bone invasion in nasopharyngeal carcinoma[J]. Biomed Mater Eng, 2014,24(1):1117-1124.
doi: 10.3233/BME-130911 pmid: 24092081 |
| [16] |
Guo YX, Sun ZP, Liu XJ , et al. Surgical safety distances in the infratemporal fossa: three-dimensional measurement study[J]. Int J Oral Maxillofac Surg, 2015,44(5):555-561.
doi: 10.1016/j.ijom.2014.06.004 pmid: 25441861 |
| [17] |
吴东东, 卜博, 陈晓雷 , 等. 融合MRI与CT图像的多模态神经导航技术在颅底显微外科手术中的应用[J]. 解放军医学院学报, 2015, ( 5):411-414.
doi: 10.3969/j.issn.2095-5227.2015.05.002 |
| [18] |
Hayashi N, Kurimoto M, Hirashima Y , et al. Efficacy of navigation in skull base surgery using composite computer graphics of magnetic resonance and computed tomography images[J]. Neurol Med Chir (Tokyo), 2001,41(7):335.
doi: 10.2176/nmc.41.335 pmid: 11487996 |
| [1] | Jiajun LIU, Guokang LIU, Yuhu ZHU. Immune-related severe pneumonia: A case report [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 932-937. |
| [2] | Kewei CHEN,Zhuo LIU,Shaohui DENG,Fan ZHANG,Jianfei YE,Guoliang WANG,Shudong ZHANG. Clinical diagnosis and treatment of renal angiomyolipoma with inferior vena cava tumor thrombus [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 617-623. |
| [3] | Shuai LIU,Lei LIU,Zhuo LIU,Fan ZHANG,Lulin MA,Xiaojun TIAN,Xiaofei HOU,Guoliang WANG,Lei ZHAO,Shudong ZHANG. Clinical treatment and prognosis of adrenocortical carcinoma with venous tumor thrombus [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 624-630. |
| [4] | Jie YANG,Jieli FENG,Shudong ZHANG,Lulin MA,Qing ZHENG. Clinical effects of transesophageal echocardiography in different surgical methods for nephrectomy combined with Mayo Ⅲ-Ⅳ vena tumor thrombectomy [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 631-635. |
| [5] | Binshuai WANG,Min QIU,Qianjin ZHANG,Maofeng TIAN,Lei LIU,Guoliang WANG,Min LU,Xiaojun TIAN,Shudong ZHANG. Experience in diagnosis and treatment of 6 cases of renal Ewing's sarcoma with venous thrombus [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 636-639. |
| [6] | Xiaodong CHAI,Ziwen SUN,Haishuang LI,Liangyi ZHU,Xiaodan LIU,Yantao LIU,Fei PEI,Qing CHANG. Clinicopathological characteristics of the CD8+ T lymphocytes infiltration and its mechanism in distinct molecular subtype of medulloblastoma [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 512-518. |
| [7] | Guozhong LIN,Changcheng MA,Chao WU,Yu SI,Jun YANG. Application of microchannel technique in minimally invasive resection of cervical intraspinal tumors [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 318-321. |
| [8] | Xiaotong LING,Liuyang QU,Danni ZHENG,Jing YANG,Xuebing YAN,Denggao LIU,Yan GAO. Three-dimensional radiographic features of calcifying odontogenic cyst and calcifying epithelial odontogenic tumor [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 131-137. |
| [9] | Ying ZHOU,Ning ZHAO,Hongyuan HUANG,Qingxiang LI,Chuanbin GUO,Yuxing GUO. Application of double-layer soft tissue suture closure technique in the surgical treatment of patients with mandible medication-related osteonecrosis of the jaw of early and medium stages [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 51-56. |
| [10] | Zi-xuan XUE,Shi-ying TANG,Min QIU,Cheng LIU,Xiao-jun TIAN,Min LU,Jing-han DONG,Lu-lin MA,Shu-dong ZHANG. Clinicopathologic features and prognosis of young renal tumors with tumor thrombus [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 802-811. |
| [11] | Dong LAN,Zhuo LIU,Yu-xuan LI,Guo-liang WANG,Xiao-jun TIAN,Lu-lin MA,Shu-dong ZHANG,Hong-xian ZHANG. Risk factors for massive hemorrhage after radical nephrectomy and removal of venous tumor thrombus [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 825-832. |
| [12] | Zhong CAO,Hong-bing CEN,Jian-hong ZHAO,Jun MEI,Ling-zhi QIN,Wei LIAO,Qi-lin AO. Expression and significance of INSM1 and SOX11 in pancreatic neuroendocrine tumor and solid pseudopapillary neoplasm [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 575-581. |
| [13] | Bin CHEN,Chao WU,Bin LIU,Tao YU,Zhen-yu WANG. Prognosis of patients with spinal intramedullary cavernous hemangioma by different treatments [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 652-657. |
| [14] | Li LIANG,Xin LI,Lin NONG,Ying DONG,Ji-xin ZHANG,Dong LI,Ting LI. Analysis of microsatellite instability in endometrial cancer: The significance of minimal microsatellite shift [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 254-261. |
| [15] | Yu-mei LAI,Zhong-wu LI,Huan LI,Yan WU,Yun-fei SHI,Li-xin ZHOU,Yu-tong LOU,Chuan-liang CUI. Clinicopathological features and prognosis of anorectal melanoma: A report of 68 cases [J]. Journal of Peking University (Health Sciences), 2023, 55(2): 262-269. |
|
||