Journal of Peking University(Health Sciences) ›› 2019, Vol. 51 ›› Issue (2): 277-282. doi: 10.19723/j.issn.1671-167X.2019.02.015
Previous Articles Next Articles
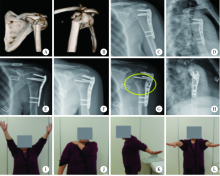
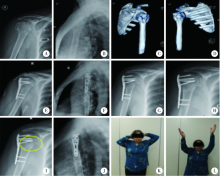
Application of the modified internal fixation method of minimally invasive percuta-neous plate osteosynthesis in treatment of proximal humeral fracture
Bing-chuan LIU,Zhong-wei YANG,Fang ZHOU,Hong-quan JI,Zhi-shan ZHANG,Yan GUO,Yun TIAN( )
)
- Department of Orthopedics, Peking University Third Hospital, Beijing 100191, China
CLC Number:
- R683.4
| [1] |
Roux A, Decroocq L, Batti SE , et al. Epidemiology of proximal humerus fractures managed in a trauma center[J]. Orthop Traumatol Surg Res, 2012,98(6):715-719.
doi: 10.1016/j.otsr.2012.05.013 |
| [2] |
Jost B, Spross C, Grehn H , et al. Locking plate fixation of fractures of the proximal humerus: analysis of complications, revision strategies and outcome[J]. J Shoulder Elbow Surg, 2013,22(4):542-549.
doi: 10.1016/j.jse.2012.06.008 |
| [3] | Maier D, Jäger M, Strohm PC , et al. Treatment of proximal humeral fractures: a review of current concepts enlightened by basic principles[J]. Acta Chir Orthop Traumatol Cech, 2012,79(4):307-316. |
| [4] | Burkhart KJ, Dietz SO, Bastian L , et al. The treatment of proximal humeral fracture in adults[J]. Dtsch Arztebl Int, 2013,110(35):591-597. |
| [5] |
Jung SW . Indirect reduction maneuver and minimally invasive approach for displaced proximal humerus fractures in elderly patients[J]. Clin Orthop Surg, 2013,5(1):66-73.
doi: 10.4055/cios.2013.5.1.66 |
| [6] |
Sohn HS, Shin SJ . Minimally invasive plate osteosynjournal for proximal humeral fractures: clinical and radiologic outcomes according to fracture type[J]. J Shoulder Elbow Surg, 2014,23(9):1334-1340.
doi: 10.1016/j.jse.2013.12.018 |
| [7] | 赵弟庆, 张丽娜, 杨广忠 , 等. MIPPO技术结合PHILOS治疗老年骨质疏松性肱骨近端骨折[J]. 中国矫形外科杂志, 2014,22(6):508-511. |
| [8] |
Gavaskar AS, Muthukumar S, Chowdary N . Biological osteosynjournal of complex proximal humerus fractures: surgical technique and results from a prospective single center trial[J]. Arch Orthop Trauma Surg, 2010,130(5):667-672.
doi: 10.1007/s00402-009-1028-0 |
| [9] | 刘振东, 马梦然 . 骨折愈合理论研究现状[J]. 中国矫形外科杂志, 2010,18(16):87-91. |
| [10] |
Parren SM . Evolution of the internal fixation of long bong fracture. The scientific basis of biological internal fixation: choosing a new balance between stability and biology[J]. J Bone Joint Surg Br, 2002,84(8):1093-1110.
doi: 10.1302/0301-620X.84B8.13752 |
| [11] |
Sonderegger J, Grob KR, Kuster MS . Dynamic plate osteosynjournal for fracture stabilization: how to do it[J]. Orthop Rev, 2010,2(1):e4.
doi: 10.4081/or.2010.e4 |
| [12] | 夏和桃, 李刚 . 现代骨外固定概念的生物学基础及应用原则[J]. 中华创伤骨科杂志, 2011,13(10):964-968. |
| [13] |
Koljonen PA, Fang C, Lau TW , et al. Minimally invasive plate osteosynjournal for proximal humeral fractures[J]. J Orthop Surg, 2015,23(2):160-163.
doi: 10.1177/230949901502300208 |
| [14] | Gardner MJ, Griffith MH, Dines JS , et al. The extended anterolateral acromial approach allows minimally invasive access to the proximal humerus[J]. Clin Orthop, 2005,434(434):123-129. |
| [15] |
Falez F, Papalia M, Greco A , et al. Minimally invasive plate osteosynjournal in proximal humeral fractures: one-year results of a prospective multicenter study[J]. Int Orthop, 2016,40(3):579-585.
doi: 10.1007/s00264-015-3069-z |
| [1] | Shi-kai XIONG,Wei-li SHI,An-hong WANG,Xing XIE,Qin-wei GUO. Radiographic diagnosis of distal fibula avulsion fractures: Comparison of ankle X-ray and three-dimensional reconstruction of CT [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 156-159. |
| [2] | Guo-jin HOU,Fang ZHOU,Yun TIAN,Hong-quan JI,Zhi-shan ZHANG,Yan GUO,yang LV,Zhong-wei YANG. Related factors of revision of distal femoral fractures treated with lateral locking plate [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1172-1177. |
| [3] | Zhong-di LIU,Ting-min XU,Yu DANG,Dian-ying ZHANG,Zhong-guo FU. Clinical effectiveness of less invasive intramedullary nail fixation combined with titanium cable cerclage for subtrochanteric fractures [J]. Journal of Peking University (Health Sciences), 2020, 52(6): 1102-1106. |
| [4] | Bing-chuan LIU,Chuan SUN,Yong XING,Fang ZHOU,Yun TIAN,Hong-quan JI,Zhi-shan ZHANG,Yan GUO,Yang LV,Zhong-wei YANG,Guo-jin HOU,Shan GAO. Analysis of risk factors for necrosis of femoral head after internal fixation surgery in young and mid-aged patients with femoral neck fracture [J]. Journal of Peking University (Health Sciences), 2020, 52(2): 290-297. |
| [5] | Yun-peng CUI,Chuan MI,Bing WANG,Yuan-xing PAN,Yun-fei LIN,Xue-dong SHI. Perioperative clinical characteristics of patients with pathological fracture of proximal femur [J]. Journal of Peking University(Health Sciences), 2019, 51(5): 875-880. |
| [6] | LIU Zhong-di, MA Ming-tai, CHEN Jian-hai, FU Zhong-guo, JIANG Bao-guo. “Time-angle measurement” reduction evaluation technique and clinical evaluation of proximal humerus fracture [J]. Journal of Peking University(Health Sciences), 2017, 49(6): 1003-1007. |
| [7] | ZHANG Bo-song, LI Wen-yi, LIU Xing-hua, WEI Jie, HE Liang, WANG Man-yi. Comparative results of non-operative and operative treatment of humeral shaft fractures [J]. Journal of Peking University(Health Sciences), 2017, 49(5): 851-854. |
| [8] | LI Xu, LI Feng-long, LU Yi, ZHU Yi-ming, GUO Si-yi, LI Yi-jun, JIANG Chun-yan. Clinical study on locking plate for the treatment of non-osteoporotic complex proximal humeral fractures [J]. Journal of Peking University(Health Sciences), 2017, 49(5): 855-860. |
| [9] | ZHANG Bo-song, LI Wen-yi, LIU Xing-hua, WEI Jie, HE Liang, WANG Man-yi. Comparative results of non-operative and operative treatment of humeral shaft fractures [J]. Journal of Peking University(Health Sciences), 0, (): 851-854. |
| [10] | LI Xu, LI Feng-long, LU Yi, ZHU Yi-ming, GUO Si-yi, LI Yi-jun, JIANG Chun-yan. Clinical study on locking plate for the treatment of non-osteoporotic complex proximal humeral fractures#br# [J]. Journal of Peking University(Health Sciences), 0, (): 855-860. |
| [11] | GAO Zhi-qiang, AN Gui-sheng, LI Shao-liang. Treatment of complicated intra-articular distal radius fractures with extended flexor carpi radialis approach [J]. Journal of Peking University(Health Sciences), 2017, 49(2): 349-353. |
| [12] | LI Ying, CHA Ye-jun, LI Ting, GONG Mao-qi, JIANG Xie-yuan. Analysis of anterolateral approach and lateral approach for the treatment of coronal shear fracture of the distal humeral [J]. Journal of Peking University(Health Sciences), 2016, 48(6): 1026-1031. |
| [13] | WU Jing-wei, SHEN Hui-liang, LIU Li-min, GAO Zhi-hua. Analysis of early failure of the PHILOS in proximal humerus fractures [J]. Journal of Peking University(Health Sciences), 2016, 48(4): 683-685. |
| [14] | . [J]. Journal of Peking University(Health Sciences), 2016, 48(4): 751-封三. |
| [15] | ZHANG Jian, JIANG Xie-yuan, HUANG Xiao-wen. Separate vertical wiring combined with tension band and Kirschner-wire plus cerclage wire in the treatment of displaced inferior pole fractures of the patella [J]. Journal of Peking University(Health Sciences), 2016, 48(3): 534-538. |
|
||