Journal of Peking University(Health Sciences) ›› 2019, Vol. 51 ›› Issue (2): 283-287. doi: 10.19723/j.issn.1671-167X.2019.02.016
Previous Articles Next Articles
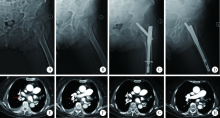
Comparison of the effects of two cephalomedullary nails (zimmer natural nail and proximal femoral nail antirotation) in treatment of elderly intertrochan teric fractures
Jian CHEN1,Cai-hong ZUO1,Cai-yi ZHANG1,Ming YANG2,Pei-xun ZHANG2,∆( )
)
- 1. Department of Orthopaedics, People’s Hospital of Xuancheng City, Xuancheng 242000, Anhui, China;
2. Department of Traumatology and Orthopaedics, Peking University People’s Hospital, Beijing 100044, China;
CLC Number:
- R683
| [1] | Haidukewych GJ . Intertrochanteric fractures: ten tips to improve results[J]. J Bone Joint Surg Am, 2009,91(3):712-719. |
| [2] |
Roberts KC, Brox WT, Jevsevar DS , et al. Management of hip fractures in the elderly[J]. J Am Acad Orthop Surg, 2015,23(2):131-137.
doi: 10.5435/JAAOS-D-14-00432 |
| [3] |
Jensen JS . Classification of trochanteric fractures[J]. Acta Orthop Scand, 1980,51(5):803-810.
doi: 10.3109/17453678008990877 |
| [4] |
杨明, 张晓萌, 张培训 , 等. 经皮导入导针结合纯侧位透视简化股骨近端防旋髓内钉操作[J]. 北京大学学报(医学版), 2015,47(2):258-262.
doi: 10.3969/j.issn.1671-167X.2015.02.013 |
| [5] |
Stern R, Lübbeke A, Suva D , et al. Prospective randomised study comparing screw versus helical blade in the treatment of low-energy trochanteric fractures[J]. Int Orthop, 2011,35(12):1855-1861.
doi: 10.1007/s00264-011-1232-8 |
| [6] |
Harris WH . Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplast. An end-result study using a new method of result evaluation[J]. J Bone Joint Surg Am, 1969,51(4):737-755.
doi: 10.2106/00004623-196951040-00012 |
| [7] | Tucker A, Donnelly KJ, McDonald S , et al. The changing face of fractures of the hip in Northern Ireland: a 15-year review[J]. Bone Joint J, 2017,99B(9):1223-1231. |
| [8] | 张树, 张继源, 杨杜明 , 等. 矢状位不稳定转子间骨折的形态特征和复位技术[J]. 北京大学学报(医学版), 2017,49(2):236-241. |
| [9] | Chatterton BD, Moores TS, Ahmad S , et al. Cause of death and factors associated with early in-hospital mortality after hip fracture[J]. Bone Joint J, 2015,97B(2):246-251. |
| [10] |
Thaler HW, Gosch M, Kammerlander C . Orthogeriatrics: hip fracture and its implications[J]. Wien Med Wochenschr, 2013,163(19/20):433-434.
doi: 10.1007/s10354-013-0229-x |
| [11] |
Pedersen SJ, Borgbjerg FM, Schousboe B , et al. A comprehensive hip fracture program reduces complication rates and mortality[J]. J Am Geriatr Soc, 2008,56(10):1831-1838.
doi: 10.1111/jgs.2008.56.issue-10 |
| [12] |
Evaniew N, Bhandari M . Cochrane in CORR®: intramedullary nails for extracapsular hip fractures in adults (review)[J]. Clin Orthop Relat Res, 2015,473(3):767-774.
doi: 10.1007/s11999-014-4123-7 |
| [13] |
Shin YS, Chae JE, Kang TW , et al. Prospective randomized study comparing two cephalomedullary nails for elderly intertrochanteric fractures: Zimmer Natural nail versus proximal femoral femoral nail antirotation Ⅱ[J]. Injury, 2017,48(7):1550-1557.
doi: 10.1016/j.injury.2017.04.011 |
| [14] | 刘中邸, 徐海林, 陈建海 , 等. 解剖型股骨近端髓内钉治疗老年转子间骨折的初步疗效[J]. 中华老年骨科与康复电子杂志, 2017,3(5):265-269. |
| [15] |
Parmar DS, Porecha MM, Chudasama S . Long proximal femoral nails versus short proximal femoral nails for the management of proximal femoral fractures: a retrospective study of 124 patients[J]. Eur J Orthop Surg Traumatol, 2011,21(3):159-164.
doi: 10.1007/s00590-010-0683-8 |
| [16] |
Chang SM, Song DL, Ma Z , et al. Mismatch of the short straight cephalomedullary nail (PFNA-Ⅱ) with the anterior bow of the femur in an Asian population[J]. J Orthop Trauma, 2014,28(1):17-22.
doi: 10.1097/BOT.0000000000000022 |
| [17] |
戴尅戎, 戴闵, 郭晓山 , 等. 中国骨科大手术静脉血栓栓塞症预防指南[J]. 中华骨科杂志, 2016,36(2):65-71.
doi: 10.3760/cma.j.issn.0253-2352.2016.02.001 |
| [18] |
García-Fuster MJ, Fabia MJ, Furió E , et al. Should we look for silent pulmonary embolism in patients with deep venous thrombosis[J]. BMC Cardiovasc Disord, 2014,14(1):178.
doi: 10.1186/1471-2261-14-178 |
| [19] |
Nosher JL, Patel A, Jagpal S , et al. Endovascular treatment of pulmonary embolism: selective review of available techniques[J]. World J Radiol, 2017,9(12):426-437.
doi: 10.4329/wjr.v9.i12.426 |
| [20] |
Najafzadeh M, Kim SC, Patterson C , et al. Patients’ perception about risks and benefits of venous thromboembolism (VTE) after orthopedic surgery: a qualitative study[J]. BMC Musculoskelet Disord, 2015,16(1):1-8.
doi: 10.1186/s12891-015-0454-0 |
| [21] |
Hou G, Zhou F, Tian Y , et al. Predicting the need for blood transfusions in elderly patients with pertrochanteric femoral fractures[J]. Injury, 2014,45(12):1932-1937.
doi: 10.1016/j.injury.2014.08.033 |
| [22] | 张培训, 薛峰, 安帅 , 等. 股骨近端防旋髓内钉和动力髋螺钉治疗股骨转子间骨折的显性和隐性失血量分析[J]. 北京大学学报(医学版), 2012,44(6):891-894. |
| [1] | HOU Guo-jin,ZHOU Fang,TIAN Yun,JI Hong-quan,ZHANG Zhi-shan,GUO Yan,LV Yang,YANG Zhong-wei,ZHANG Ya-wen. Risk factors of recurrent kyphosis in thoracolumbar burst fracture patients treated by short segmental pedicle screw fixation [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 167-174. |
| [2] | Yi-ran ZHANG,Feng RAO,Wei PI,Pei-xun ZHANG,Bao-guo JIANG. Proximal femoral nails antirotation and dynamic hip screws for fixation of unstable intertrochanteric fractures of femur: A meta-analysis [J]. Journal of Peking University(Health Sciences), 2019, 51(3): 493-500. |
| [3] | LIU Zhong-di, MA Ming-tai, CHEN Jian-hai, FU Zhong-guo, JIANG Bao-guo. “Time-angle measurement” reduction evaluation technique and clinical evaluation of proximal humerus fracture [J]. Journal of Peking University(Health Sciences), 2017, 49(6): 1003-1007. |
| [4] | ZHANG Bo-song, LI Wen-yi, LIU Xing-hua, WEI Jie, HE Liang, WANG Man-yi. Comparative results of non-operative and operative treatment of humeral shaft fractures [J]. Journal of Peking University(Health Sciences), 2017, 49(5): 851-854. |
| [5] | GAO Zhi-qiang, AN Gui-sheng, LI Shao-liang. Treatment of complicated intra-articular distal radius fractures with extended flexor carpi radialis approach [J]. Journal of Peking University(Health Sciences), 2017, 49(2): 349-353. |
| [6] | ZHAO Chun-peng, WANG Jun-qiang, SU Yong-gang, HAN Wei, ZHOU Li, WANG Man-yi. Clinical research on robot-assisted percutaneous pelvic and acetabular screws surgery [J]. Journal of Peking University(Health Sciences), 2017, 49(2): 274-280. |
| [7] | ZHANG Quan, SUN Ning, HUANG Qiang, ZHU Shi-wen. Minimally invasive plate osteosynthesis for treatment of proximal humeral fractures through anterolateral acromial approach [J]. Journal of Peking University(Health Sciences), 2017, 49(2): 242-245. |
| [8] | ZHANG Shu, ZHANG Ji-yuan, YANG Du-ming, YANG Ming, ZHANG Pei-xun. Morphology character and reduction methods of sagittally unstable intertrochanteric fractures [J]. Journal of Peking University(Health Sciences), 2017, 49(2): 236-241. |
| [9] | LI Ying, CHA Ye-jun, LI Ting, GONG Mao-qi, JIANG Xie-yuan. Analysis of anterolateral approach and lateral approach for the treatment of coronal shear fracture of the distal humeral [J]. Journal of Peking University(Health Sciences), 2016, 48(6): 1026-1031. |
| [10] | WU Jing-wei, SHEN Hui-liang, LIU Li-min, GAO Zhi-hua. Analysis of early failure of the PHILOS in proximal humerus fractures [J]. Journal of Peking University(Health Sciences), 2016, 48(4): 683-685. |
| [11] | ZHANG Jian, JIANG Xie-yuan, HUANG Xiao-wen. Separate vertical wiring combined with tension band and Kirschner-wire plus cerclage wire in the treatment of displaced inferior pole fractures of the patella [J]. Journal of Peking University(Health Sciences), 2016, 48(3): 534-538. |
| [12] | SUN Bin, ZHANG Zhi-Shan, ZHOU Fang, TIAN Yun, JI Hong-Quan, GUO Yan, 吕Yang , YANG Zhong-Wei. Surgical treatment of inferior pole comminuted fractures of patella with new type tension band [J]. Journal of Peking University(Health Sciences), 2015, 47(2): 272-275. |
| [13] | ZHAO Jing-Xin, SU Xiu-Yun, ZHAO Zhe, ZHANG Li-Cheng, ZHANG Li-Hai, TANG Pei-Fu. Radiographic analysis of treatment of inter-trochanteric fractures using proximal femoral nails [J]. Journal of Peking University(Health Sciences), 2015, 47(2): 263-268. |
| [14] | YANG Ming, ZHANG Xiao-Meng, ZHANG Pei-Xun, WANG Tian-Bing, FU Zhong-Guo, ZHANG Dian-Ying, JIANG Bao-Guo. Applying percutaneous placement of guide wire combined with true lateral view fluoroscopy proximal femoral nail anti-rotation fixation [J]. Journal of Peking University(Health Sciences), 2015, 47(2): 258-262. |
| [15] | LU Hao, JIANG Bao-Guo, FU Zhong-Guo, ZHANG Dian-Ying, WANG Tian-Bing, XU Hai-Lin, ZHANG Pei-Xun. Surgical treatment of internal fixation failure after clavicular fracture operation [J]. Journal of Peking University(Health Sciences), 2014, 46(5): 766-770. |
|
||