Journal of Peking University(Health Sciences) ›› 2020, Vol. 52 ›› Issue (1): 18-23. doi: 10.19723/j.issn.1671-167X.2020.01.003
Previous Articles Next Articles
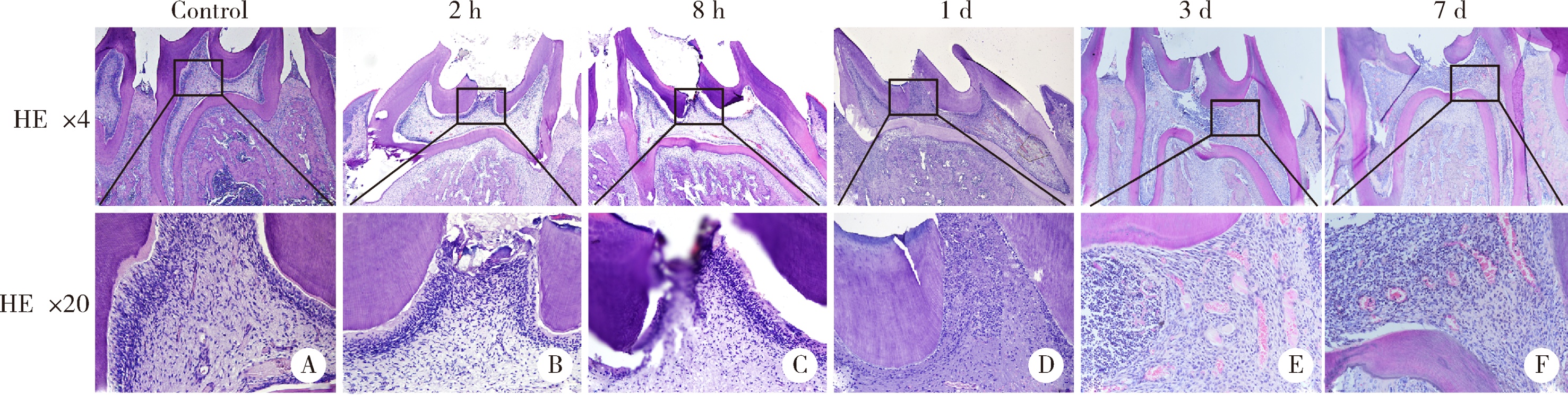
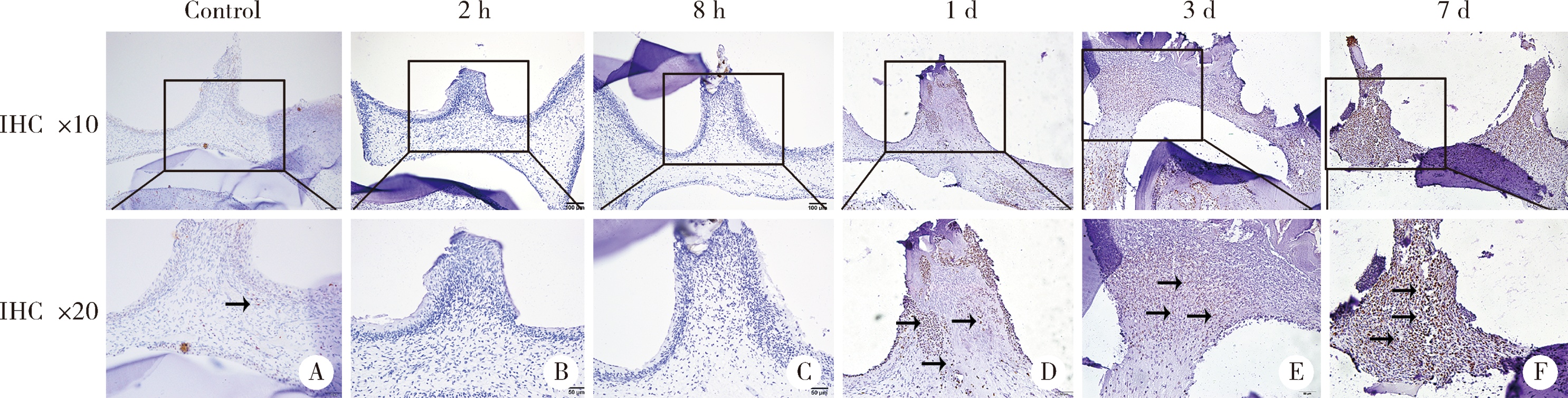
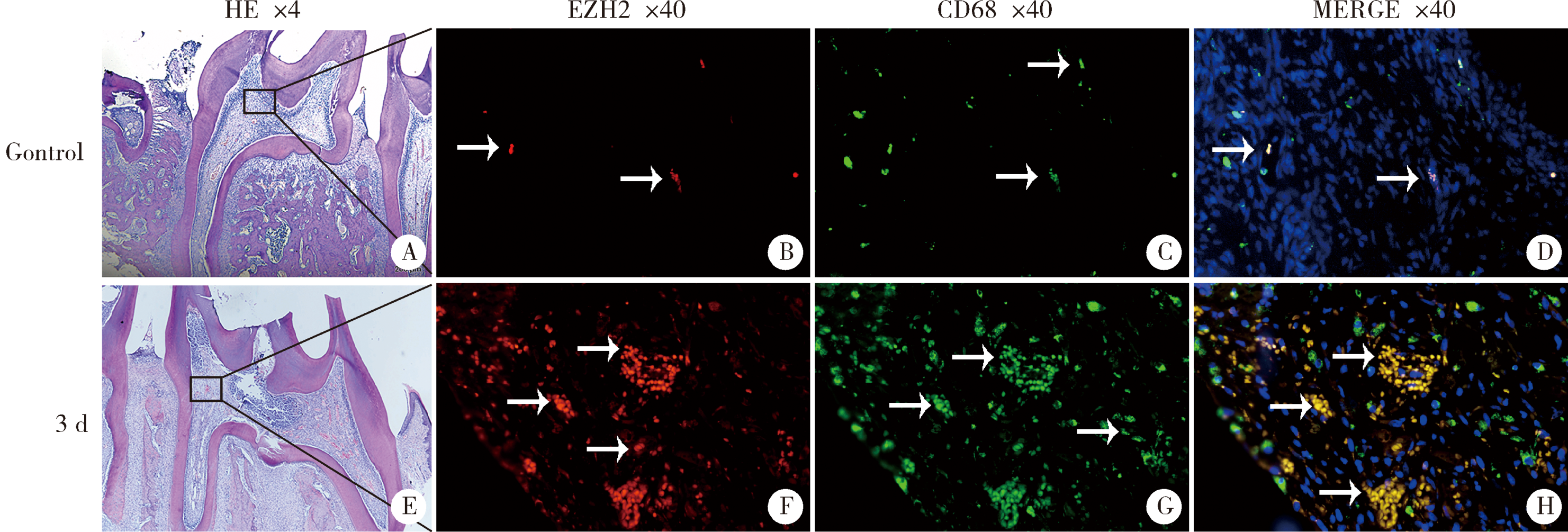
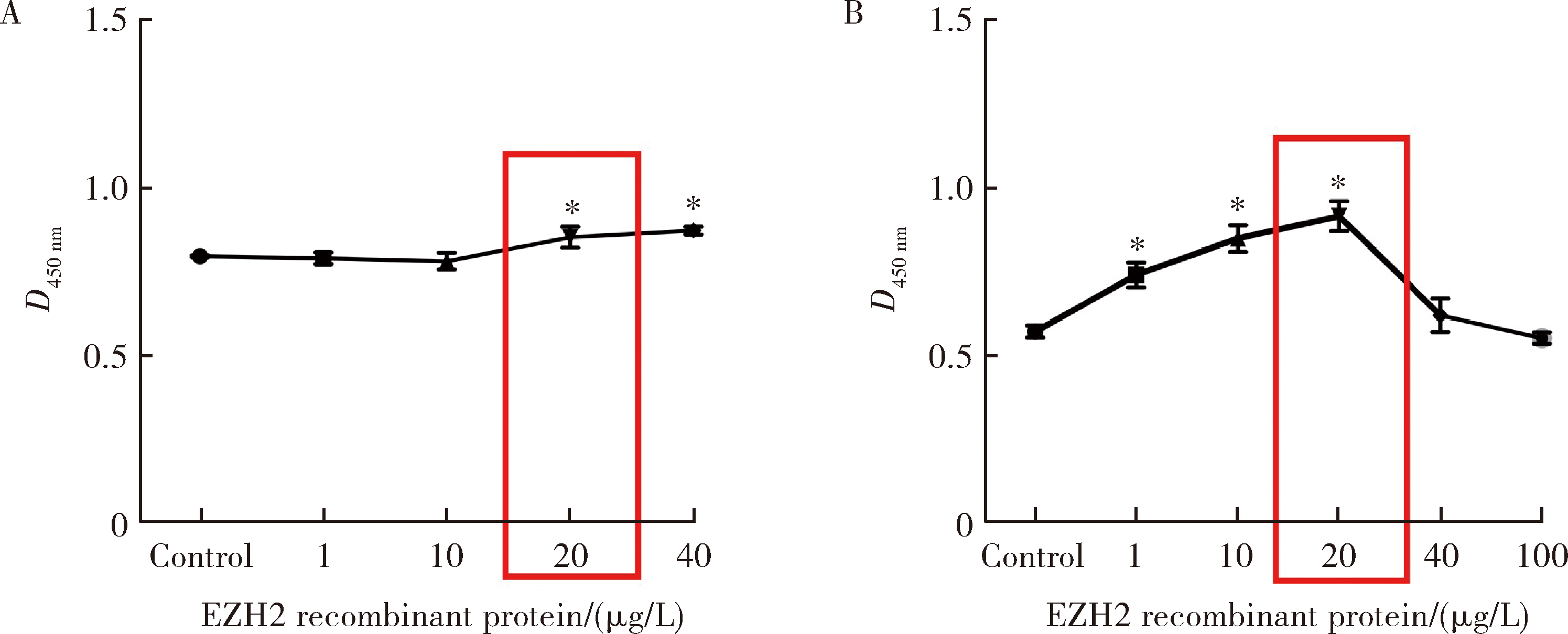
Enhancer of zeste homolog 2 affects dental pulp inflammation by regulating macrophage chemotaxis
Ying-yi CHEN,Zi-qi HU,Tian-qian HUI( ),He LIU(
),He LIU( )
)
- Department of Pediatric Dentistry, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
CLC Number:
- R781.31
| [1] | Aas JA, Griffen AL, Dardis SR , et al. Bacteria of dental caries in primary and permanent teeth in children and young adults[J]. J Clin Microbiol, 2008,46(4):1407-1417. |
| [2] | Tokuda M, Sakuta T, Fushuku A , et al. Regulation of interleukin-6 expression in human dental pulp cell cultures stimulated with Prevotella intermedia lipopolysaccharide[J]. J Endod, 2001,27(4):273-277. |
| [3] | Goldberg M, Farges JC, Lacerda-Pinheiro S , et al. Inflammatory and immunological aspects of dental pulp repair[J]. Pharmacol Res, 2008,58(2):137-147. |
| [4] | Zhao Y, Wang CL, Li RM , et al. Wnt5a promotes inflammatory responses via nuclear factor kappaB (NF-kappaB) and mitogen-activated protein kinase (MAPK) pathways in human dental pulp cells[J]. J Biol Chem, 2014,289(30):21028-21039. |
| [5] | Hui T, A P, Zhao Y , et al. EZH2 regulates dental pulp inflammation by direct effect on inflammatory factors[J]. Arch Oral Biol, 2018,85(1):16-22. |
| [6] | Li B, Yu F, Wu F , et al. EZH2 Impairs human dental pulp cell mineralization via the Wnt/β-catenin pathway[J]. J Dent Res, 2018,97(5):571-579. |
| [7] | Feinberg AP . Phenotypic plasticity and the epigenetics of human disease[J]. Nature, 2007,447(7143):433-440. |
| [8] | Calvanese V, Lara E, Kahn A , et al. The role of epigenetics in aging and age-related diseases[J]. Ageing Res Rev, 2009,8(4):268-276. |
| [9] | Bayarsaihan D . Epigenetic mechanisms in inflammation[J]. J Dent Res, 2011,90(1):9-17. |
| [10] | Deng P, Chen QM, Hong C , et al. Histone methyltransferases and demethylases: regulators in balancing osteogenic and adipogenic differentiation of mesenchymal stem cells[J]. Int J Oral Sci, 2015,7(4):197-204. |
| [11] | Hui T, A P, Zhao Y , et al. EZH2, a potential regulator of dental pulp inflammation and regeneration[J]. J Endod, 2014,40(8):1132-1138. |
| [12] | Hoang M, Kim JJ, Kim Y , et al. Alcohol-induced suppression of KDM6B dysregulates the mineralization potential in dental pulp stem cells[J]. Stem Cell Res, 2016,17(1):111-121. |
| [13] | Yadav R, Weng HR . EZH2 regulates spinal neuroinflammation in rats with neuropathic pain[J]. Neuroscience, 2017,349(5):106-117. |
| [14] | Arifuzzaman S, Das A, Kim SH , et al. Selective inhibition of EZH2 by a small molecule inhibitor regulates microglial gene expression essential for inflammation[J]. Biochem Pharmacol, 2017,137(8):61-80. |
| [15] | Liu Y, Peng J, Sun T , et al. Epithelial EZH2 serves as an epigenetic determinant in experimental colitis by inhibiting TNFα-mediated inflammation and apoptosis[J]. Proc Natl Acad Sci USA, 2017,114(19):E3796-E3805. |
| [16] | Wu H, He M, Yang R , et al. Astrocyte elevated gene-1 participates in the production of pro-inflammatory cytokines in dental pulp cells via NF-kappaB signalling pathway[J]. Int Endod J, 2018,51(10):1130-1138. |
| [17] | Renard E, Gaudin A, Bienvenu G , et al. Immune cells and molecular networks in experimentally induced pulpitis[J]. J Dent Res, 2016,95(2):196-205. |
| [18] | 吴晓恋, 张盛丹, 魏亚娟 , 等. 热休克蛋白27及热休克因子1在牙髓炎中的表达研究[J]. 牙体牙髓牙周病学杂志, 2017,27(1):7-11. |
| [19] | Adrian JC, Bernier JL, Sprague WG . Laser and the dental pulp[J]. J Am Dent Assoc, 1971,83(1):113-117. |
| [20] | 王勤, 张成飞, 林琼光 , 等. 脉冲Nd:YAG激光照射牙本质对牙髓的影响[J]. 现代口腔医学杂志, 1996,10(1):20-22. |
| [21] | Cleaton-Jones P, Duggal M, Parak R , et al. Pulpitis induction in baboon primary teeth using carious dentine or Streptococcus mutans[J]. SADJ, 2004,59(3):119-122. |
| [22] | Gunawan M, Venkatesan N, Loh JT , et al. The methyltransferase Ezh2 controls cell adhesion and migration through direct methylation of the extranuclear regulatory protein talin[J]. Nat Immunol, 2015,16(5):505-516. |
| [1] | Shuang WANG,Chu-fang PENG,He LIU. Pulpotomy of human primary molars with novel bioceramic material [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1196-1201. |
| [2] | Yan-rui ZHAO,Yang LIU,Dong WANG,Wen-rui LV,Jun-lin ZHOU. Effects of sulfur dioxide on alveolar macrophage apoptosis in acute lung injury induced by limb ischemia/reperfusion in rats [J]. Journal of Peking University(Health Sciences), 2019, 51(2): 239-244. |
| [3] | BAI Ning,YANG Ling-fei,AN Li-hua,WANG wen,LI Yun-qian,SHENG Hui,WANG Tong,LI Hua-kan,YUAN Lan. Dynamic visual analysis of neutrophils chemotaxis in peritoneal cavity of schizophrenic model in mice [J]. Journal of Peking University(Health Sciences), 2018, 50(2): 226-230. |
| [4] | LING Long, ZHAO Yu-ming, GE Li-hong. Impact of different degree pulpitis on cell proliferation and osteoblastic differentiation of dental pulp stem cell in Beagle immature premolars [J]. Journal of Peking University(Health Sciences), 2016, 48(5): 878-883. |
| [5] | CHEN Hong-tao, WANG Wen-ying, WANG Jin, LIANG Ya-ping, WANG Xiao-ting, HOU Guang-min, JI Ai-ping. Risk assessment of different grades of hypertension during the treatment of patients with acute pulpitis [J]. Journal of Peking University(Health Sciences), 2016, 48(1): 89-93. |
| [6] | YU Tao, JIANG Ting, WEI Qing-mei, LI Yi-fen, David L. Kaplan. Wound healing effects of silk fibroin-bone morphogenetic protein-2 scaffolds on inflammatory pulp in rats [J]. Journal of Peking University(Health Sciences), 2015, 47(5): 814-819. |
|
||