Journal of Peking University (Health Sciences) ›› 2020, Vol. 52 ›› Issue (3): 444-450. doi: 10.19723/j.issn.1671-167X.2020.03.008
Previous Articles Next Articles
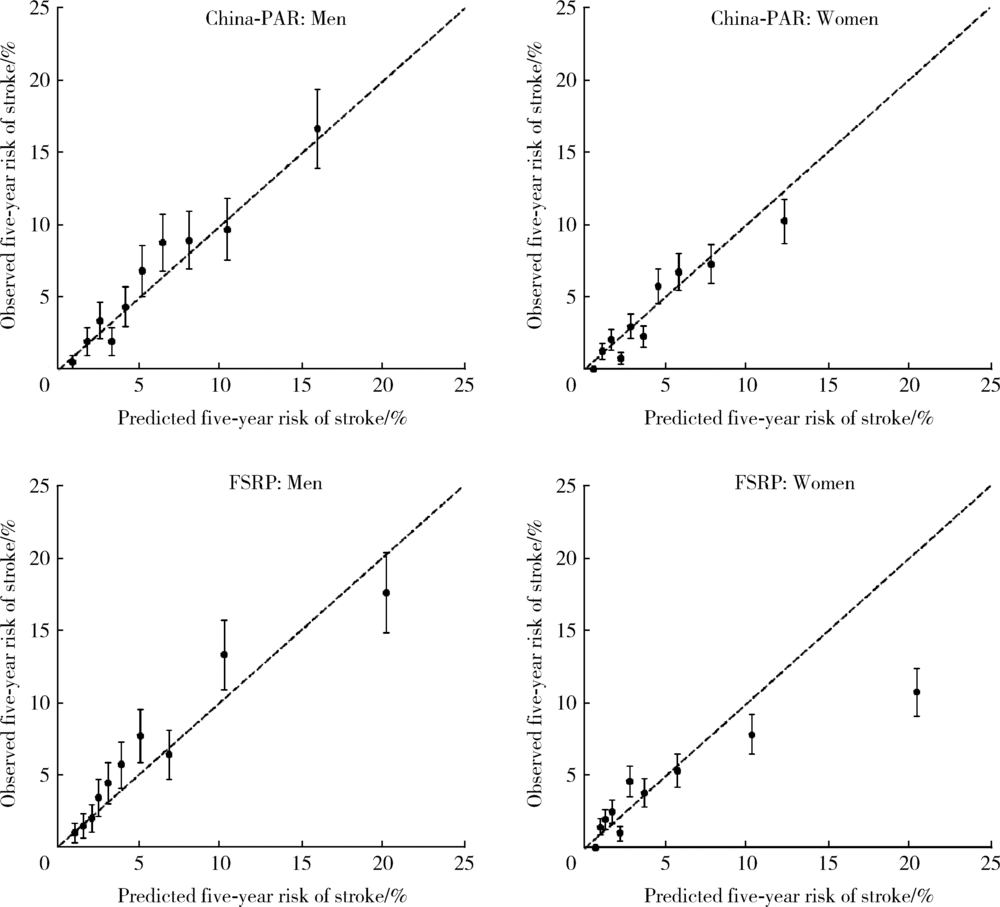
Application of the China-PAR stroke risk equations in a rural northern Chinese population
Xun TANG1,Du-dan ZHANG2,Xiao-fei LIU1,Qiu-ping LIU1,Yang CAO1,Na LI3,Shao-ping HUANG3,Hui-dong DOU4,Pei GAO1,△( ),Yong-hua HU1,△(
),Yong-hua HU1,△( )
)
- 1. Department of Epidemiology and Biostatistics, Peking University School of Public Health, Beijing 100191, China
2. Cardiovascular Epidemiology Unit, Department of Public Health and Primary Care, University of Cambridge, Cambridge CB1 8RN, United Kingdom
3. Fangshan District Center for Disease Control and Prevention, Beijing 102446, China
4. The First Hospital of Fangshan District, Beijing 102400, China
CLC Number:
- R181.2
| [1] | GBD 2016 lifetime risk of stroke collaborators. Global, regional, and country-specific lifetime risks of stroke, 1990 and 2016BD 2016 lifetime risk of stroke collaborators. Global, regional, and country-specific lifetime risks of stroke, 1990 and 2016[J]. N Engl J Med, 2018,379(25):2429-2437. |
| [2] | Zhou M, Wang H, Zeng X, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990—2017: a systematic analysis for the global burden of disease study 2017[J]. Lancet, 2019,394(10204):1145-1158. |
| [3] |
Lloyd-Jones DM, Braun LT, Ndumele CE, et al. Use of risk assessment tools to guide decision-making in the primary prevention of atherosclerotic cardiovascular disease: a special report from the American Heart Association and American College of Cardiology[J]. Circulation, 2019,139(25):e1162-e1177.
pmid: 30586766 |
| [4] | Dufouil C, Beiser A, McLure LA, et al. Revised Framingham stroke risk profile to reflect temporal trends[J]. Circulation, 2017,135(12):1145-1159. |
| [5] |
Xing X, Yang X, Liu F, et al. Predicting 10-year and lifetime stroke risk in Chinese population[J]. Stroke, 2019,50(9):2371-2378.
pmid: 31390964 |
| [6] | 唐迅, 何柳, 曹洋, 等. 基于农村社区人群的心血管危险因素相对效应和性别差异的分层研究[J]. 北京大学学报(医学版), 2011,43(3):379-385. |
| [7] | 唐迅, 张杜丹, 何柳, 等. China-PAR模型在北方农村人群中预测动脉粥样硬化性心血管疾病发病风险的应用[J]. 北京大学学报(医学版), 2017,49(3):439-445. |
| [8] |
Alba AC, Agoritsas T, Walsh M, et al. Discrimination and calibration of clinical prediction models: users’ guides to the medical literature[J]. JAMA, 2017,318(14):1377-1384.
pmid: 29049590 |
| [9] |
Cook NR, Ridker PM. Calibration of the pooled cohort equations for atherosclerotic cardiovascular disease: an update[J]. Ann Intern Med, 2016,165(11):786-794.
pmid: 27723890 |
| [10] | 中国心血管病风险评估和管理指南编写联合委员会. 中国心血管病风险评估和管理指南[J]. 中华预防医学杂志, 2019,53(1):13-35. |
| [11] |
Flueckiger P, Longstreth W, Herrington D, et al. Revised Framingham stroke risk score, nontraditional risk markers, and incident stroke in a multiethnic cohort[J]. Stroke, 2018,49(2):363-369.
doi: 10.1161/STROKEAHA.117.018928 pmid: 29311270 |
| [12] |
Bos D, Ikram MA, Leening MJG, et al. The revised Framingham stroke risk profile in a primary prevention population: the Rotterdam study[J]. Circulation, 2017,135(22):2207-2209.
pmid: 28559499 |
| [1] | Huan YU,Ruo-tong YANG,Si-yue WANG,Jun-hui WU,Meng-ying WANG,Xue-ying QIN,Tao WU,Da-fang CHEN,Yi-qun WU,Yong-hua HU. Metformin use and risk of ischemic stroke in patients with type 2 diabetes: A cohort study [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 456-464. |
| [2] | Yun-jing ZHANG,Li-ying QIAO,Meng QI,Ying YAN,Wei-wei KANG,Guo-zhen LIU,Ming-yuan WANG,Yun-feng XI,Sheng-feng WANG. Development and validation of risk prediction model for new-onset cardiovascular diseases among breast cancer patients: Based on regional medical data of Inner Mongolia [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 471-479. |
| [3] | Ruo-tong YANG,Meng-ying WANG,Chun-nan LI,Huan YU,Xiao-wen WANG,Jun-hui WU,Si-yue WANG,Jia-ting WANG,Da-fang CHEN,Tao WU,Yong-hua HU. Interaction between ischemic stroke risk loci identified by genome-wide association studies and sleep habits [J]. Journal of Peking University (Health Sciences), 2022, 54(3): 412-420. |
| [4] | Yu-han DENG,Yong JIANG,Zi-yao WANG,Shuang LIU,Yu-xin WANG,Bao-hua LIU. Long short-term memory and Logistic regression for mortality risk prediction of intensive care unit patients with stroke [J]. Journal of Peking University (Health Sciences), 2022, 54(3): 458-467. |
| [5] | LIU Jie,GUO Chao. A prospective cohort study of the influence of positive/negative effectivity on the mortality risk of the Chinese elderly [J]. Journal of Peking University (Health Sciences), 2022, 54(2): 255-260. |
| [6] | WU Jun-hui,WU Yi-qun,WU Yao,WANG Zi-jing,WU Tao,QIN Xue-ying,WANG Meng-ying,WANG Xiao-wen,WANG Jia-ting,HU Yong-hua. Incidence and risk factors of ischemic stroke in patients with type 2 diabetes among urban workers in Beijing, China [J]. Journal of Peking University (Health Sciences), 2022, 54(2): 249-254. |
| [7] | REN Guo-yong,WU Xue-mei, ,LI Jie-yu,SUN Wei-ping,HUANG Yi-ning. Susceptibility vessel sign in subacute stroke patients with large vessel occlusion [J]. Journal of Peking University (Health Sciences), 2021, 53(6): 1133-1138. |
| [8] | Ya-fei LIU,Lin-lin SONG,Mao-wei XING,Li-xin CAI,Dong-xin WANG. Comparison of pulse pressure variation, stroke volume variation, and plethysmographic variability index in pediatric patients undergoing craniotomy [J]. Journal of Peking University (Health Sciences), 2021, 53(5): 946-951. |
| [9] | Yue HOU,Xu-tong ZHAO,Zhi-ying XIE,Yun YUAN,Zhao-xia WANG. Mitochondrial encephalopathy, lactic acidosis and stroke-like episodes / myoclonus epilepsy with ragged-red fibers /Leigh overlap syndrome caused by mitochondrial DNA 8344A>G mutation [J]. Journal of Peking University (Health Sciences), 2020, 52(5): 851-855. |
| [10] | Wen-ying MENG,Wan-tong HUANG,Jie ZHANG,Ming-yuan JIAO,Lei JIN,Lei JIN. Relationship between serum vitamin E concentration in first trimester and the risk of developing hypertension disorders complicating pregnancy [J]. Journal of Peking University (Health Sciences), 2020, 52(3): 470-478. |
| [11] | Zi-chang JIA,Huan-ju BIAN,Xuan LI,Jing-yuan LUAN,Chang-ming WANG,Qi-jia LIU,Jin-tao HAN. Application of Neuroform EZ stent in the treatment of severe intracranial arterial stenosis with complex symptomatic [J]. Journal of Peking University(Health Sciences), 2019, 51(5): 835-839. |
| [12] | Wen TANG,Jun-yi GAO,Xin-yu MA,Chao-he ZHANG,Lian-tao MA,Ya-sha WANG. Application of recurrent neural network in prognosis of peritoneal dialysis [J]. Journal of Peking University(Health Sciences), 2019, 51(3): 602-608. |
| [13] | Zi-chang JIA,Xuan LI,Xiao-gang LI,Xiang-zhu ZENG,Jing-yuan LUAN,Chang-ming WANG,Jin-tao HAN. Mechanical thrombectomy treatment in patients with acute ischemic stroke: a single center study [J]. Journal of Peking University(Health Sciences), 2019, 51(2): 256-259. |
| [14] | LIN Hong-bo, CHEN Yi, SHEN Peng, LI Xiao-yong,SI Ya-qin, ZHANG Du-dan, TANG Xun, GAO Pei. Incidence and risk factors of chronic kidney disease in community-based patients with diabetes [J]. Journal of Peking University(Health Sciences), 2018, 50(3): 416-421. |
| [15] | SUN Zhuo-nan, MENG Xiu-li, WANG Jun, GUO Xiang-yang, HAN Jin-tao, QI Qiang. Perioperative stroke effectively treated by an acute stroke team including anesthesia department: a case report [J]. Journal of Peking University(Health Sciences), 2017, 49(6): 1090-1094. |
|
||