Journal of Peking University (Health Sciences) ›› 2020, Vol. 52 ›› Issue (3): 514-520. doi: 10.19723/j.issn.1671-167X.2020.03.018
Previous Articles Next Articles
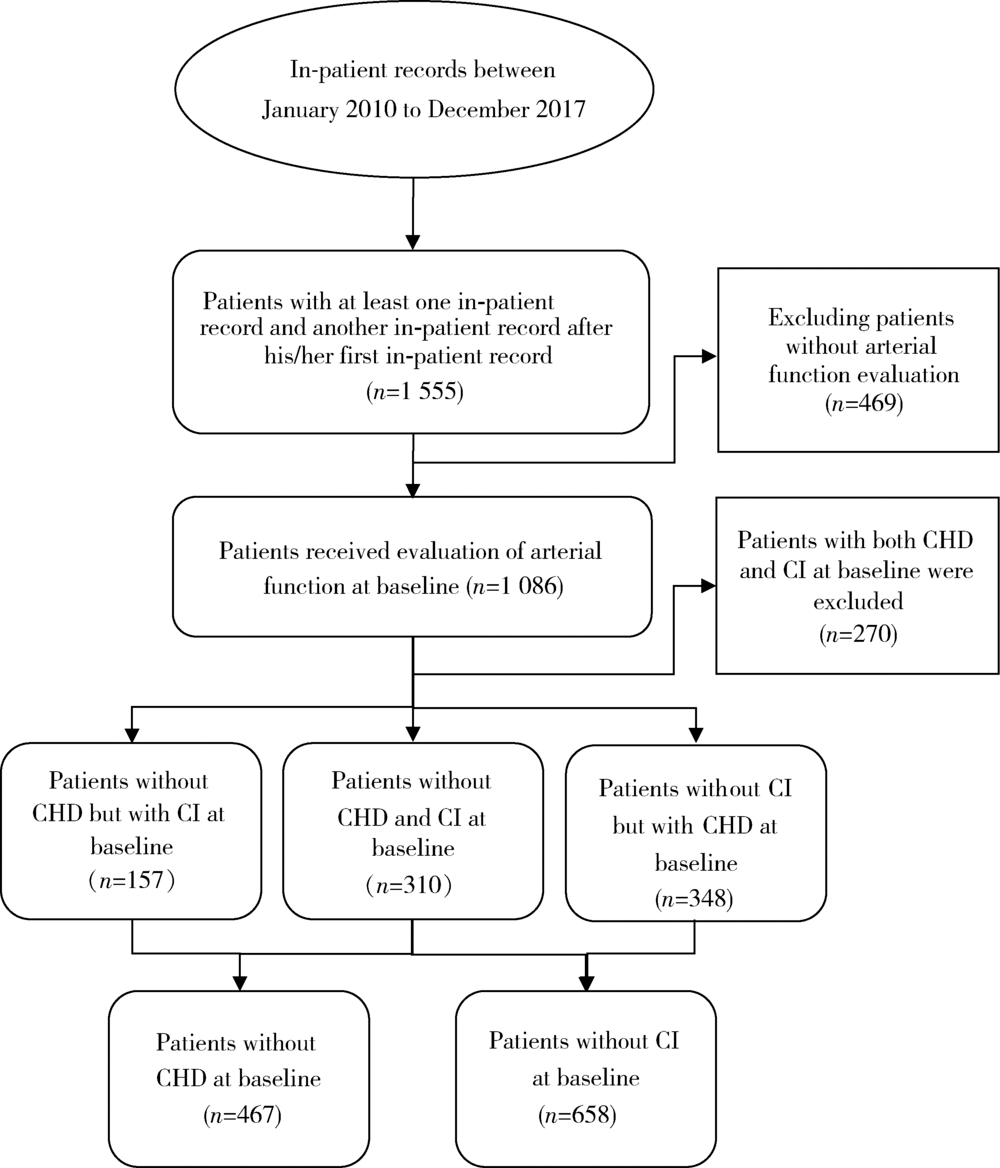
Predictive value of vascular health indicators on newly cardiovascular events: Preliminary validation of Beijing vascular health stratification system
Huan LIU1,2,Ying-dong HE3,Jin-bo LIU1,2,Wei HUANG1,Na ZHAO1,Hong-wei ZHAO1,Xiao-hua ZHOU2,3,△( ),Hong-yu WANG1,2,△(
),Hong-yu WANG1,2,△( )
)
- 1. Vascular Medicine Center, Peking University Shougang Hospital, Beijing 100144, China
2. Vascular Health Research Center of Peking University Health Science Center, Beijing 100191, China
3. Department of Biostatistics, Peking University, Beijing International Center for Mathematical Research, Beijing 100871, China
CLC Number:
- R541.4
| [1] | Winsor T. Influence of arterial disease on the systolic blood pressure gradients of the extremity[J]. Am J Med Sci, 1950,220(2):117-126. |
| [2] |
Ohkuma T, Ninomiya T, Tomiyama H, et al. Ankle-brachial index measured by oscillometry is predictive for cardiovascular disease and premature death in the Japanese population: An individual participant data meta-analysis[J]. Atherosclerosis, 2018,275:141-148.
pmid: 29902702 |
| [3] | Heald CL, Fowkes FG, Murray GD, et al. Risk of mortality and cardiovascular disease associated with the ankle-brachial index: Systematic review[J]. Atherosclerosis, 2006,189(1):61-69. |
| [4] | Zhong Q, Hu MJ, Cui YJ, et al. Carotid-femoral pulse wave velocity in the prediction of cardiovascular events and mortality: an updated systematic review and meta-analysis[J]. Angiology, 2018,69(7):617-629. |
| [5] | Willum-Hansen T, Staessen JA, Torp-Pedersen C, et al. Prognostic value of aortic pulse wave velocity as index of arterial stiffness in the general population[J]. Circulation, 2006,113(5):664-670. |
| [6] |
Niiranen TJ, Kalesan B, Larson MG, et al. Aortic-brachial arte-rial stiffness gradient and cardiovascular risk in the community: the Framingham Heart Study[J]. Hypertension, 2017,69(6):1022-1028.
pmid: 28396534 |
| [7] | Mitchell GF, Hwang SJ, Vasan RS, et al. Arterial stiffness and cardiovascular events: the Framingham Heart Study[J]. Circulation, 2010,121(4):505-511. |
| [8] |
Tillin T, Chambers J, Malik I, et al. Measurement of pulse wave velocity: site matters[J]. J Hypertens, 2007,25(2):383-389.
pmid: 17211245 |
| [9] | Shirai K, Utino J, Otsuka K, et al. A novel blood pressure-independent arterial wall stiffness parameter; cardio-ankle vascular index (CAVI)[J]. J Atheroscler Thromb, 2006,13(2):101-107. |
| [10] | Laucevišius A, Ryliškytè L, Balsytè J, et al. Association of cardio-ankle vascular index with cardiovascular risk factors and cardiovascular events in metabolic syndrome patients[J]. Medicina (Kaunas), 2015,51(3):152-158. |
| [11] | Matsushita K, Ding N, Kim ED, et al. Cardio-ankle vascular index and cardiovascular disease: Systematic review and meta-analysis of prospective and cross-sectional studies[J]. J Clin Hypertens (Greenwich), 2019,21(1):16-24. |
| [12] | Sato Y, Nagayama D, Saiki A, et al. Cardio-ankle vascular index is independently associated with future cardiovascular events in outpatients with metabolic disorders[J]. J Atheroscler Thromb, 2016,23(5):596-605. |
| [13] | Satoh-Asahara N, Kotani K, Yamakage H, et al. Cardio-ankle vascular index predicts for the incidence of cardiovascular events in obese patients: a multicenter prospective cohort study (Japan Obesity and Metabolic Syndrome Study: JOMS)[J]. Atherosclerosis, 2015,242(2):461-468. |
| [14] |
Vallée A, Petruescu L, Kretz S, et al. Added value of aortic pulse wave velocity index in a predictive diagnosis decision tree of coronary heart disease[J]. Am J Hypertens, 2019,32(4):375-383.
pmid: 30624553 |
| [15] |
Velescu A, Clara A, Peñafiel J, et al. Adding low ankle brachial index to classical risk factors improves the prediction of major cardiovascular events. The REGICOR study[J]. Atherosclerosis, 2015,241(2):357-363.
pmid: 26071658 |
| [16] |
Gronewold J, Hermann DM, Lehmann N, et al. Ankle-brachial index predicts stroke in the general population in addition to classical risk factors[J]. Atherosclerosis, 2014,233(2):545-550.
pmid: 24530962 |
| [17] | 中国医药教育协会血管医学专业委员会, 中华医学会北京心血管病学分会血管专业学组, 北京大学医学部血管疾病社区防治中心. 中国血管健康评估系统应用指南[J]. 中华医学杂志, 2018,98(37):2955-2967. |
| [18] | 王宏宇, 刘欢. 新的血管健康分级标准与血管医学[J]. 心血管病学进展, 2015,36(4):365-368. |
| [19] | Liu H, Liu J, Zhao H, et al. The design and rationale of the Beijing Vascular Disease Patients Evaluation Study (BEST study)[J]. Contemp Clin Trials Commun, 2017,7:18-22. |
| [20] |
Hong JB, Leonards CO, Endres M, et al. Ankle-brachial index and recurrent stroke risk: meta-analysis[J]. Stroke, 2016,47(2):317-322.
doi: 10.1161/STROKEAHA.115.011321 pmid: 26658450 |
| [1] | Zhicun LI, Tianyu WU, Lei LIANG, Yu FAN, Yisen MENG, Qian ZHANG. Risk factors analysis and nomogram model construction of postoperative pathological upgrade of prostate cancer patients with single core positive biopsy [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 896-901. |
| [2] | Ye YAN,Xiaolong LI,Haizhui XIA,Xuehua ZHU,Yuting ZHANG,Fan ZHANG,Ke LIU,Cheng LIU,Lulin MA. Analysis of risk factors for long-term overactive bladder after radical prostatectomy [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 589-593. |
| [3] | Yan CHEN,Kuangmeng LI,Kai HONG,Shudong ZHANG,Jianxing CHENG,Zhongjie ZHENG,Wenhao TANG,Lianming ZHAO,Haitao ZHANG,Hui JIANG,Haocheng LIN. Retrospective study on the impact of penile corpus cavernosum injection test on penile vascular function [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 680-686. |
| [4] | Bo PANG,Tongjun GUO,Xi CHEN,Huaqi GUO,Jiazhang SHI,Juan CHEN,Xinmei WANG,Yaoyan LI,Anqi SHAN,Hengyi YU,Jing HUANG,Naijun TANG,Yan WANG,Xinbiao GUO,Guoxing LI,Shaowei WU. Personal nitrogen oxides exposure levels and related influencing factors in adults over 35 years old in Tianjin and Shanghai [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 700-707. |
| [5] | Jing HE,Zhongze FANG,Ying YANG,Jing LIU,Wenyao MA,Yong HUO,Wei GAO,Yangfeng WU,Gaoqiang XIE. Relationship between lipid metabolism molecules in plasma and carotid atheroscle-rotic plaques, traditional cardiovascular risk factors, and dietary factors [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 722-728. |
| [6] | Shan CAI,Yihang ZHANG,Ziyue CHEN,Yunfe LIU,Jiajia DANG,Di SHI,Jiaxin LI,Tianyu HUANG,Jun MA,Yi SONG. Status and pathways of factors influencing physical activity time among elementary and junior high school students in Beijing [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 403-410. |
| [7] | Zuhong ZHANG,Tianjiao CHEN,Jun MA. Associations between puberty timing and cardiovascular metabolic risk factors among primary and secondary students [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 418-423. |
| [8] | Tianjing ZHOU,Qiuping LIU,Minglu ZHANG,Xiaofei LIU,Jiali KANG,Peng SHEN,Hongbo LIN,Xun TANG,Pei GAO. Comparison of initiation of antihypertensive therapy strategies for primary prevention of cardiovascular diseases in Chinese population: A decision-analytic Markov modelling study [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 441-447. |
| [9] | Yuting LIN,Huali WANG,Yu TIAN,Litong GONG,Chun CHANG. Factors influencing cognitive function among the older adults in Beijing [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 456-461. |
| [10] | Jinrong ZHU,Yana ZHAO,Wei HUANG,Weiwei ZHAO,Yue WANG,Song WANG,Chunyan SU. Clinical characteristics of COVID-19 infection in patients undergoing hemodialysis [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 267-272. |
| [11] | Zhanhong LAI,Jiachen LI,Zelin YUN,Yonggang ZHANG,Hao ZHANG,Xiaoyan XING,Miao SHAO,Yuebo JIN,Naidi WANG,Yimin LI,Yuhui LI,Zhanguo LI. A unicenter real-world study of the correlation factors for complete clinical response in idiopathic inflammatory myopathies [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 284-292. |
| [12] | Xiaoqian SI,Xiujuan ZHAO,Fengxue ZHU,Tianbing WANG. Risk factors for acute respiratory distress syndrome in patients with traumatic hemorrhagic shock [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 307-312. |
| [13] | Yangyang LI,Lin HOU,Zijun MA,Shanyamei HUANG,Jie LIU,Chaomei ZENG,Jiong QIN. Association of pregnancy factors with cow's milk protein allergy in infants [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 144-149. |
| [14] | Xiaoqiang LIU,Yin ZHOU. Risk factors of perioperative hypertension in dental implant surgeries with bone augmentation [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 93-98. |
| [15] | Liang LUO,Yun LI,Hong-yan WANG,Xiao-hong XIANG,Jing ZHAO,Feng SUN,Xiao-ying ZHANG,Ru-lin JIA,Chun LI. Anti-endothelial cell antibodies in predicting early miscarriage [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1039-1044. |
|
||