Journal of Peking University (Health Sciences) ›› 2021, Vol. 53 ›› Issue (4): 744-749. doi: 10.19723/j.issn.1671-167X.2021.04.021
Previous Articles Next Articles
Expression and distribution of calprotectin in healthy and inflamed periodontal tissues
GAO Hong-yu1,2,MENG Huan-xin1,Δ( ),HOU Jian-xia1,HUANG Bao-xin1,LI Wei1
),HOU Jian-xia1,HUANG Bao-xin1,LI Wei1
- 1. Department of Periodontology, Peking University School and Hospital of Stomatology & National Center of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology, Beijing 100081, China
2. Department of Periodontology, Stomatological Hospital of Tianjin Medical University, Tianjin 300070, China
CLC Number:
- R781.4
| [1] |
Hajishengallis G. Periodontitis: from microbial immune subversion to systemic inflammation [J]. Nat Rev Immunol, 2015, 15(1):30-44.
doi: 10.1038/nri3785 pmid: 25534621 |
| [2] |
Page RC, Kornman KS. The pathogenesis of human periodontitis: an introduction [J]. Periodontol 2000, 1997, 14(1):9-11.
doi: 10.1111/prd.1997.14.issue-1 |
| [3] | Di Benedetto A, Gigante I, Colucci S, et al. Periodontal disease: linking the primary inflammation to bone loss [J/OL]. Clin Dev Immunol, 2013, 2013: 503754(2013-05-23)[2019-12-01]. https//www.hindawi.com/journals/ . |
| [4] |
Kolaczkowska E, Kubes P. Neutrophil recruitment and function in health and inflammation [J]. Nat Rev Immunol, 2013, 13(3):159-175.
doi: 10.1038/nri3399 pmid: 23435331 |
| [5] |
Jin L. An update on innate defense molecules of human gingiva [J]. Periodontol 2000, 2011, 56(1):125-142.
doi: 10.1111/prd.2011.56.issue-1 |
| [6] |
Goyette J, Geczy CL. Inflammation-associated S100 proteins: new mechanisms that regulate function [J]. Amino Acids, 2011, 41(4):821-842.
doi: 10.1007/s00726-010-0528-0 |
| [7] |
Lundy FT, Chalk R, Lamey PJ, et al. Identification of MRP-8 (calgranulin A) as a major responsive protein in chronic periodontitis [J]. J Pathol, 2000, 192(4):540-544.
pmid: 11113873 |
| [8] |
Lundy FT, Chalk R, Lamey PJ, et al. Quantitative analysis of MRP-8 in gingival crevicular fluid in periodontal health and disease using microbore HPLC [J]. J Clin Periodontol, 2001, 28(12):1172-1177.
pmid: 11737516 |
| [9] |
Kido J, Nakamura T, Kido R, et al. Calprotectin in gingival crevicular fluid correlates with clinical and biochemical markers of periodontal disease [J]. J Clin Periodontol, 1999, 26(10):653-657.
pmid: 10522776 |
| [10] |
Andersen E, Dessaix IM, Perneger T, et al. Myeloid-related protein (MRP8/14) expression in gingival crevice fluid in periodontal health and disease and after treatment [J]. J Periodontal Res, 2010, 45(4):458-463.
doi: 10.1111/j.1600-0765.2009.01257.x pmid: 20337885 |
| [11] |
Ren XY, Xu L, Meng HX, et al. Family-based association analysis of S100A8 genetic polymorphisms with aggressive periodontitis [J]. J Periodontal Res, 2009, 44(2):184-192.
doi: 10.1111/j.1600-0765.2008.01103.x pmid: 19210342 |
| [12] |
Li QY, Meng HX, Zhang L, et al. Correlation between single nucleotide polymorphisms in a calprotectin subunit gene and risk of periodontitis in a Chinese population [J]. Ann Hum Genet, 2007, 71(Pt 3):312-324.
doi: 10.1111/ahg.2007.71.issue-3 |
| [13] |
Sun XJ, Meng HX, Shi D, et al. Analysis of plasma calprotectin and polymorphisms of S100A8 in patients with aggressive periodontitis [J]. J Periodontal Res, 2011, 46(3):354-360.
doi: 10.1111/j.1600-0765.2011.01350.x pmid: 21463326 |
| [14] | 孙晓军, 孟焕新, 释栋, 等. 侵袭性牙周炎患者血浆钙结合蛋白与血液中性粒细胞数相关性的研究 [J]. 中华口腔医学杂志, 2014, 49(11):649-651. |
| [15] |
Suryono, Kido J, Hayashi N, et al. Effect of porphyromonas gingivalis lipopolysaccharide, tumor necrosis factor-alpha, and interleukin-1beta on calprotectin release in human monocytes [J]. J Periodontol, 2003, 74(12):1719-1724.
doi: 10.1902/jop.2003.74.12.1719 pmid: 29539076 |
| [16] |
Schlegel Gomez R, Langer P, Pelka M, et al. Variational expression of functionally different macrophage markers (27E10, 25F9, RM3/1) in normal gingiva and inflammatory periodontal disease [J]. J Clin Periodontol, 1995, 22(5):341-346.
pmid: 7541406 |
| [17] |
Li W, Huang B, Liu K, et al. Up-regulated leptin in periodontitis promotes inflammatory cytokine expression in periodontal ligament cells [J]. J Periodontol, 2015, 86(7):917-926.
doi: 10.1902/jop.2015.150030 |
| [18] |
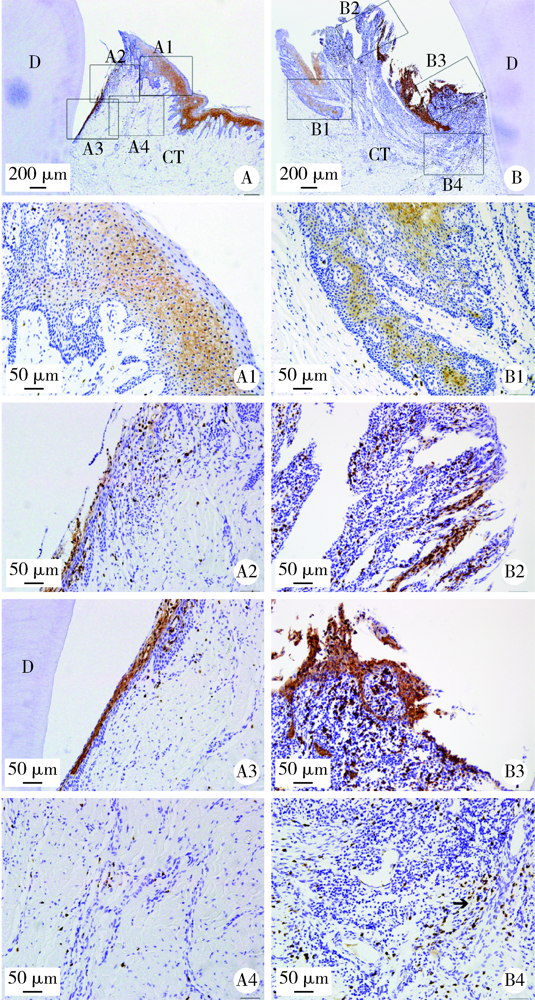
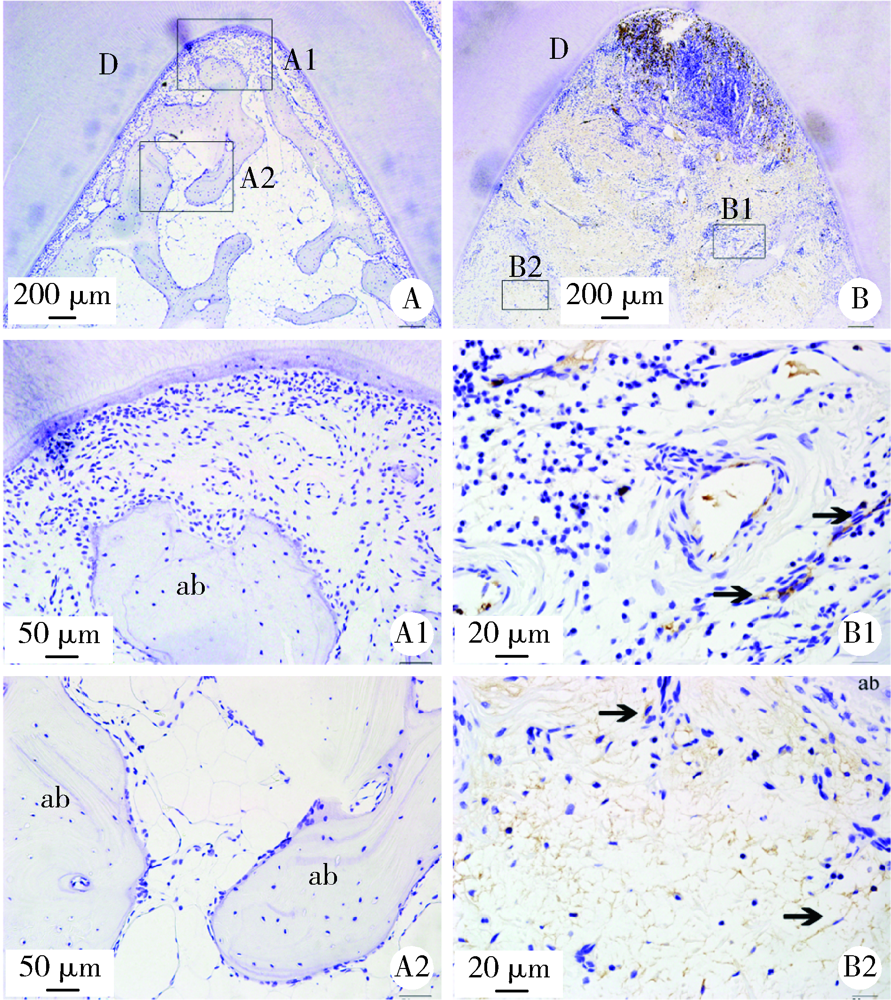
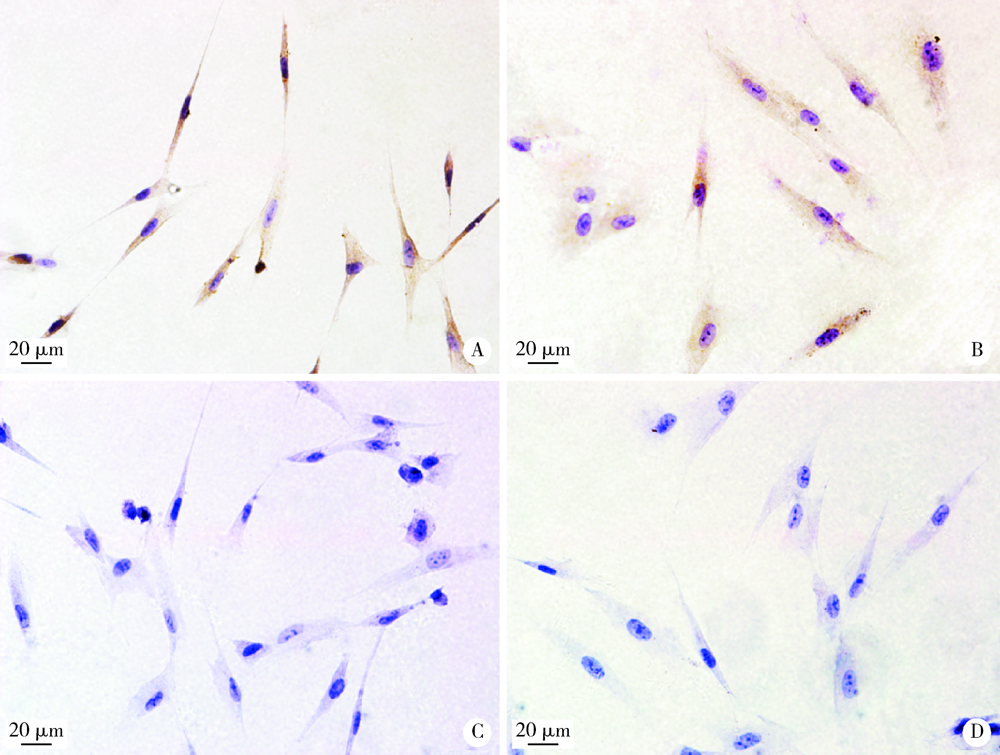
Gao H, Hou J, Meng H, et al. Proinflammatory effects and mechanisms of calprotectin on human gingival fibroblasts [J]. J Periodontal Res, 2017, 52(6):975-983.
doi: 10.1111/jre.12465 pmid: 28643937 |
| [19] |
Gao H, Zhang X, Zheng Y, et al. S100A9-induced release of interleukin (IL)-6 and IL-8 through toll-like receptor 4 (TLR4) in human periodontal ligament cells [J]. Mol Immunol, 2015, 67(2 Pt B):223-232.
doi: 10.1016/j.molimm.2015.05.014 |
| [20] |
Hiroshima Y, Bando M, Kataoka M, et al. Regulation of antimicrobial peptide expression in human gingival keratinocytes by interleukin-1alpha [J]. Arch Oral Biol, 2011, 56(8):761-767.
doi: 10.1016/j.archoralbio.2011.01.004 pmid: 21316034 |
| [21] |
Hsu K, Champaiboon C, Guenther BD, et al. Anti-infective protective properties of S100 calgranulins [J]. Antiinflamm Antiallergy Agents Med Chem, 2009, 8(4):290-305.
doi: 10.2174/187152309789838975 |
| [22] |
Jonsson D, Nebel D, Bratthall G, et al. The human periodontal ligament cell: a fibroblast-like cell acting as an immune cell [J]. J Periodontal Res, 2011, 46(2):153-157.
doi: 10.1111/jre.2011.46.issue-2 |
| [23] |
Ara T, Kurata K, Hirai K, et al. Human gingival fibroblasts are critical in sustaining inflammation in periodontal disease [J]. J Periodontal Res, 2009, 44(1):21-27.
doi: 10.1111/jre.2009.44.issue-1 |
| [24] |
Nisapakultorn K, Ross KF, Herzberg MC. Calprotectin expression in vitro by oral epithelial cells confers resistance to infection by porphyromonas gingivalis [J]. Infect Immun, 2001, 69(7):4242-4247.
pmid: 11401960 |
| [25] |
Yen T, Harrison CA, Devery JM, et al. Induction of the S100 chemotactic protein, CP-10, in murine microvascular endothelial cells by proinflammatory stimuli [J]. Blood, 1997, 90(12):4812-4821.
pmid: 9389698 |
| [1] | Yuru HU,Juan LIU,Wenjing LI,Yibing ZHAO,Qiqiang LI,Ruifang LU,Huanxin MENG. Relationship between short-chain fatty acids in the gingival crevicular fluid and periodontitis of stage Ⅲ or Ⅳ [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 332-337. |
| [2] | Han ZHANG,Yixuan QIN,Diyuan WEI,Jie HAN. A preliminary study on compliance of supportive treatment of patients with periodontitis after implant restoration therapy [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 39-44. |
| [3] | Chang SHU,Ye HAN,Yuzhe SUN,Zaimu YANG,Jianxia HOU. Changes of parameters associated with anemia of inflammation in patients with stage Ⅲ periodontitis before and after periodontal initial therapy [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 45-50. |
| [4] | Xi-yan PEI,Wen YANG,Xiang-ying OUYANG,Feng SUN. Comparison of clinical effects between periodontal endoscopy aiding subgingival debridement and flap surgery [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 716-720. |
| [5] | Jing WEN,Xiang-ying OUYANG,Xi-yan PEI,Shan-yong QIU,Jian-ru LIU,Wen-yi LIU,Cai-fang CAO. Multivariable analysis of tooth loss in subjects with severe periodontitis over 4-year natural progression [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 70-77. |
| [6] | ZHU Xiao-ling,LI Wen-jing,WANG Xian-e,SONG Wen-li,XU Li,ZHANG Li,FENG Xiang-hui,LU Rui-fang,SHI Dong,MENG Huan-xin. Gene polymorphisms of cytochrome B-245 alpha chain (CYBA) and cholesteryl ester transfer protein (CETP) and susceptibility to generalized aggressive periodontitis [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 18-22. |
| [7] | XU Xin-ran,HUO Peng-cheng,HE Lu,MENG Huan-xin,ZHU Yun-xuan,JIN Dong-si-qi. Comparison of initial periodontal therapy and its correlation with white blood cell level in periodontitis patients with or without diabetes mellitus [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 48-53. |
| [8] | LIU Jian,WANG Xian-e,LV Da,QIAO Min,ZHANG Li,MENG Huan-xin,XU Li,MAO Ming-xin. Association between root abnormalities and related pathogenic genes in patients with generalized aggressive periodontitis [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 16-23. |
| [9] | Hong-yu GAO,Jing-ling XU,Huan-xin MENG,Lu HE,Jian-xia HOU. Effect of initial periodontal therapy on blood parameters related to erythrocyte and platelet in patients with type 2 diabetes mellitus and chronic periodontitis [J]. Journal of Peking University (Health Sciences), 2020, 52(4): 750-754. |
| [10] | Yue YAN,Xian-e WANG,Ya-lin ZHAN,Li-li MIAO,Ye HAN,Chu-ren ZHANG,Zhao-guo YUE,Wen-jie HU,Jian-xia HOU. Clinical outcomes of ultrasonic subgingival debridement combined with manual root planing in severe periodontitis [J]. Journal of Peking University(Health Sciences), 2020, 52(1): 64-70. |
| [11] | Yong ZHANG,Chang LIU,Bin CHEN,Fan CHEN,Jin-yu DUAN,Meng-jun ZHANG,Jian JIAO. Associations of impaired glucose metabolism with chronic peridontitis in pre-diabetes patients [J]. Journal of Peking University(Health Sciences), 2020, 52(1): 71-76. |
| [12] | Jie ZHU,Jian-hong LI,Ting-ting YUAN,Lu He,Yu-hong LIANG. Relationship between periodontitis and osteoporosis in postmenopausal women [J]. Journal of Peking University(Health Sciences), 2019, 51(6): 1115-1118. |
| [13] | Shu-wen SHI,Yang MENG,Jian JIAO,Wen-jing LI,Huan-xin MENG,Qing-xian LUAN,Wan-chun WANG. Tooth loss and multivariable analysis after 5-year non-surgical periodontal treatment on molars with furcation involvement [J]. Journal of Peking University(Health Sciences), 2019, 51(5): 913-918. |
| [14] | Ren-jie DU,Jian JIAO,Yan-heng ZHOU,Jie SHI. Occlusal changes before and after orthodontic treatment in patients with aggressive periodontitis [J]. Journal of Peking University(Health Sciences), 2019, 51(5): 919-924. |
| [15] | LIU Yuan, LUAN Qing-xian. Association between chronic periodontitis and carotid intima-media thickness of middle-aged and older adults in Shijingshan community of Beijing [J]. Journal of Peking University(Health Sciences), 2018, 50(2): 264-270. |
|
||