Journal of Peking University (Health Sciences) ›› 2022, Vol. 54 ›› Issue (1): 68-76. doi: 10.19723/j.issn.1671-167X.2022.01.011
Previous Articles Next Articles
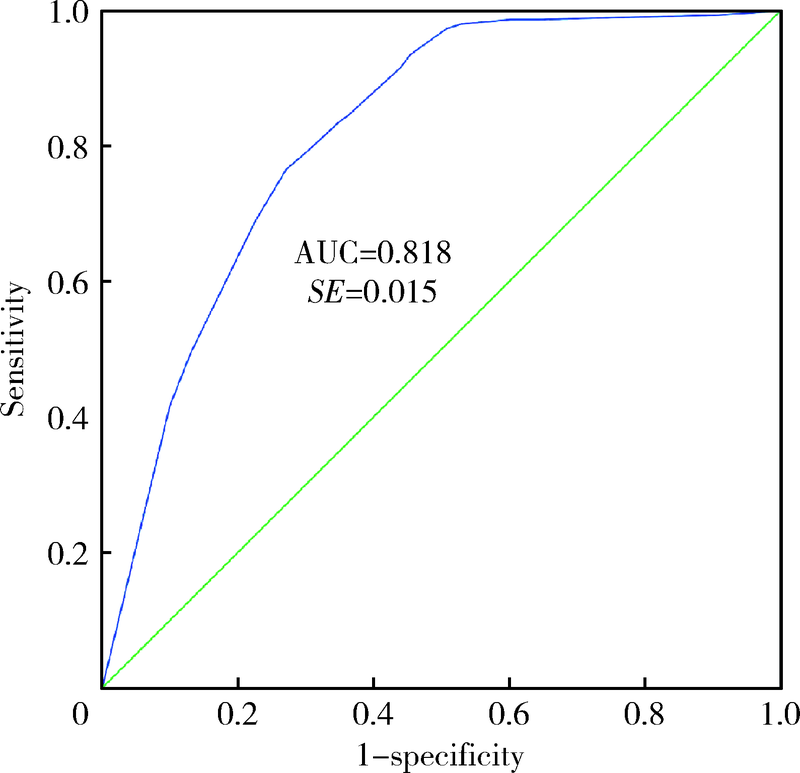
Analysis of etiological characteristics and establishment of prediction model of postoperative infections in patients undergoing oral squamous cell carcinoma surgery with free flap reconstruction
SU Jun-qi1,SONG Yang1,XIE Shang2,△( )
)
- 1. Department of Clinical Laboratory, Peking University School and Hospital of Stomatology, Beijing 100081, China
2. Department of Oral and Maxillofacial Surgery, Peking University School and Hospital of Stomatology & National Center of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology & NHC Research Center of Engineering and Technology for Computerized Dentistry & NMPA Key Laboratory for Dental Materials, Beijing 100081, China
CLC Number:
- R782.3
| [1] |
Panarese I, Aquino G, Ronchi A, et al. Oral and oropharyngeal squamous cell carcinoma: Prognostic and predictive parameters in the etiopathogenetic route[J]. Expert Rev Anticancer ther, 2019, 19(2):105-119.
doi: 10.1080/14737140.2019.1561288 |
| [2] |
Cannon RB, Houlton JJ, Mendez E, et al. Methods to reduce postoperative surgical site infections after head and neck oncology surgery[J]. Lancet Oncol, 2017, 18(7):e405-e413.
doi: 10.1016/S1470-2045(17)30375-3 |
| [3] |
McBain AJ, Sissons C, Ledder RG, et al. Development and cha-racterization of a simple perfused oral microcosm[J]. J Appl Microbiol, 2005, 98(3):624-634.
pmid: 15715865 |
| [4] | Jansisyanont P, Kasemsai W, Bamroong P. Factors related to the treatment outcome of maxillofacial fascia space infection[J]. J Oral Max Surg Med Pathol, 2015, 27(4):458-464. |
| [5] | 张建丽, 刘玉坤, 任起辉, 等. 行口腔颌面外科术患者术后感染病原学特征及相关因素分析[J]. 中华医院感染学杂志, 2018, 28(3):440-443. |
| [6] | 李月莉, 苏翠霞, 高凤蕊, 等. 口腔颌面外科患者气管切开术后肺部感染的病原学分析及干预对策[J]. 中华医院感染学杂志, 2014, 24(5):1239-1241. |
| [7] |
Manchon A, Prados-Frutos JC, Rueda-Rodriguez C, et al. Anti-biotic release from calcium phosphate materials in oral and maxillofacial surgery: Molecular, cellular and pharmaceutical aspects[J]. Curr Pharm Biotechnol, 2017, 18(1):52-63.
doi: 10.2174/1389201018666161114145827 |
| [8] | 刘登峰, 孙仁义, 肖进, 等. 口腔颌面外科患者医院感染病原菌分布及耐药性分析[J]. 中华医院感染学杂志, 2014, 24(23):5928-5930. |
| [9] | 李新芳, 顾华芳, 顾永华, 等. 肠杆菌科细菌耐药性与抗菌药物使用强度的相关性分析[J]. 中华医院感染学杂志, 2016, 26(1):16-18. |
| [10] |
Batard E, Ollivier F, Boutoille D, et al. Relationship between hospital antibiotic use and quinolone resistance in Escherichia coli[J]. Int J Infect Dis, 2013, 17(4):e254-e258.
doi: 10.1016/j.ijid.2012.10.005 |
| [11] | 解泽强, 菅记涌, 孙盼盼, 等. 2010—2015年医院铜绿假单胞菌感染分布及耐药性分析[J]. 中华医院感染学杂志, 2017, 27(3):498-500. |
| [12] | 张艳, 魏华波, 王志强, 等. 医院感染铜绿假单胞菌的分布及耐药性研究[J]. 中华医院感染学杂志, 2014, 24(13):3139-3141. |
| [13] | 侯飞, 王玲, 崔伟锋, 等. 铜绿假单胞菌医院感染的危险因素及耐药性分析[J]. 中华医院感染学杂志, 2013, 23(16):4050-4052. |
| [14] | Zhao Y, Guo L, Li J, et al. Molecular epidemiology, antimicro-bial susceptibility, and pulsed-field gel electrophoresis genotyping of Pseudomonas aeruginosa isolates from mink[J]. Can J Vet Res, 2018, 82(4):256-263. |
| [15] |
Shanthi J, Pazhanimurugan R, Gopikrishnan V, et al. Mechanism of drug resistance, characterization of plasmid-borne determinants and transformation study in P. aeruginosa from burn and ICU units-its susceptibility pattern[J]. Burns, 2013, 39(4):643-649.
doi: 10.1016/j.burns.2012.08.012 pmid: 22980776 |
| [16] | 郑百慧, 龚春梅, 黎敏, 等. 呼吸与危重症医学病房分离的碳青霉烯耐药铜绿假单胞菌的分子流行病学[J]. 中华医院感染学杂志, 2020, 30(17):2610-2614. |
| [17] |
Oliveira MC, Oliveira CR, Gonçalves KV, et al. Enterobacte-riaceae resistant to third generation cephalosporins upon hospital admission: Risk factors and clinical outcomes[J]. Braz J Infect Dis, 2015, 19(3):239-245.
doi: 10.1016/j.bjid.2015.01.006 |
| [18] |
Guo Z, Zhang J, Gong Z, et al. Correlation of factors associated with postoperative infection in patients with malignant oral and maxillofacial tumours: A Logistic regression analysis[J]. Br J Oral Maxillofac Surg, 2019, 57(5):460-465.
doi: S0266-4356(19)30123-8 pmid: 31006505 |
| [19] | Anehosur VS, Karadiguddi P, Joshi VK, et al. Elective tracheostomy in head and neck surgery: Our experience[J]. J Clin Diagn Res, 2017, 11(5): ZC36-ZC39. |
| [20] |
Goetz C, Burian NM, Weitz J, et al. Temporary tracheotomy in microvascular reconstruction in maxillofacial surgery: Benefit or threat?[J]. J Craniomaxillofac Surg, 2019, 47(4):642-646.
doi: 10.1016/j.jcms.2019.01.017 |
| [21] |
Li L, Yuan W, Zhang S, et al. Analysis of risk factors for pneumonia in 482 patients undergoing oral cancer surgery with tracheo-tomy[J]. J Oral Maxillofac Surg, 2016, 74(2):415-419.
doi: 10.1016/j.joms.2015.08.018 |
| [22] |
Xu J, Hu J, Yu P, et al. Perioperative risk factors for postoperative pneumonia after major oral cancer surgery: A retrospective analysis of 331 cases[J]. PLoS One, 2017, 12(11):e0188167.
doi: 10.1371/journal.pone.0188167 |
| [23] |
Algar FJ, Alvarez A, Salvatierra A, et al. Predicting pulmonary complications after pneumonectomy for lung cancer[J]. Eur J Cardiothorac Surg, 2003, 23(2):201-208.
doi: 10.1016/S1010-7940(02)00719-4 |
| [24] |
Maeng SH, Yoo HS, Choi SH, et al. Impact of parainfluenza virus infection in pediatric cancer patients[J]. Pediatr Blood Cancer, 2012, 59(4):708-710.
doi: 10.1002/pbc.23390 pmid: 22095941 |
| [25] |
Liu P, Li X, Luo M, et al. Risk factors for carbapenem-resistant Klebsiella pneumoniae infection: A meta-analysis[J]. Microb Drug Resist, 2018, 24(2):190-198.
doi: 10.1089/mdr.2017.0061 |
| [26] |
Zhu WM, Yuan Z, Zhou HY. Risk factors for carbapenem-resis-tant Klebsiella pneumoniae infection relative to two types of control patients: A systematic review and meta-analysis[J]. Antimicrob Resist Infect Control, 2020, 9(1):23.
doi: 10.1186/s13756-020-0686-0 |
| [1] | Zhicun LI, Tianyu WU, Lei LIANG, Yu FAN, Yisen MENG, Qian ZHANG. Risk factors analysis and nomogram model construction of postoperative pathological upgrade of prostate cancer patients with single core positive biopsy [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 896-901. |
| [2] | Ye YAN,Xiaolong LI,Haizhui XIA,Xuehua ZHU,Yuting ZHANG,Fan ZHANG,Ke LIU,Cheng LIU,Lulin MA. Analysis of risk factors for long-term overactive bladder after radical prostatectomy [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 589-593. |
| [3] | Yan CHEN,Kuangmeng LI,Kai HONG,Shudong ZHANG,Jianxing CHENG,Zhongjie ZHENG,Wenhao TANG,Lianming ZHAO,Haitao ZHANG,Hui JIANG,Haocheng LIN. Retrospective study on the impact of penile corpus cavernosum injection test on penile vascular function [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 680-686. |
| [4] | Bo PANG,Tongjun GUO,Xi CHEN,Huaqi GUO,Jiazhang SHI,Juan CHEN,Xinmei WANG,Yaoyan LI,Anqi SHAN,Hengyi YU,Jing HUANG,Naijun TANG,Yan WANG,Xinbiao GUO,Guoxing LI,Shaowei WU. Personal nitrogen oxides exposure levels and related influencing factors in adults over 35 years old in Tianjin and Shanghai [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 700-707. |
| [5] | Jing HE,Zhongze FANG,Ying YANG,Jing LIU,Wenyao MA,Yong HUO,Wei GAO,Yangfeng WU,Gaoqiang XIE. Relationship between lipid metabolism molecules in plasma and carotid atheroscle-rotic plaques, traditional cardiovascular risk factors, and dietary factors [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 722-728. |
| [6] | Shan CAI,Yihang ZHANG,Ziyue CHEN,Yunfe LIU,Jiajia DANG,Di SHI,Jiaxin LI,Tianyu HUANG,Jun MA,Yi SONG. Status and pathways of factors influencing physical activity time among elementary and junior high school students in Beijing [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 403-410. |
| [7] | Zuhong ZHANG,Tianjiao CHEN,Jun MA. Associations between puberty timing and cardiovascular metabolic risk factors among primary and secondary students [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 418-423. |
| [8] | Yuting LIN,Huali WANG,Yu TIAN,Litong GONG,Chun CHANG. Factors influencing cognitive function among the older adults in Beijing [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 456-461. |
| [9] | Jinrong ZHU,Yana ZHAO,Wei HUANG,Weiwei ZHAO,Yue WANG,Song WANG,Chunyan SU. Clinical characteristics of COVID-19 infection in patients undergoing hemodialysis [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 267-272. |
| [10] | Zhanhong LAI,Jiachen LI,Zelin YUN,Yonggang ZHANG,Hao ZHANG,Xiaoyan XING,Miao SHAO,Yuebo JIN,Naidi WANG,Yimin LI,Yuhui LI,Zhanguo LI. A unicenter real-world study of the correlation factors for complete clinical response in idiopathic inflammatory myopathies [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 284-292. |
| [11] | Xiaoqian SI,Xiujuan ZHAO,Fengxue ZHU,Tianbing WANG. Risk factors for acute respiratory distress syndrome in patients with traumatic hemorrhagic shock [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 307-312. |
| [12] | Junqi SU,Xiaoying WANG,Zhiqiang SUN. Establishment and verification of a prognostic nomogram for survival of tongue squamous cell carcinoma patients who underwent cervical dissection [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 120-130. |
| [13] | Yangyang LI,Lin HOU,Zijun MA,Shanyamei HUANG,Jie LIU,Chaomei ZENG,Jiong QIN. Association of pregnancy factors with cow's milk protein allergy in infants [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 144-149. |
| [14] | Xiaoqiang LIU,Yin ZHOU. Risk factors of perioperative hypertension in dental implant surgeries with bone augmentation [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 93-98. |
| [15] | Liang LUO,Yun LI,Hong-yan WANG,Xiao-hong XIANG,Jing ZHAO,Feng SUN,Xiao-ying ZHANG,Ru-lin JIA,Chun LI. Anti-endothelial cell antibodies in predicting early miscarriage [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1039-1044. |
|
||