Journal of Peking University (Health Sciences) ›› 2022, Vol. 54 ›› Issue (6): 1086-1093. doi: 10.19723/j.issn.1671-167X.2022.06.005
Previous Articles Next Articles
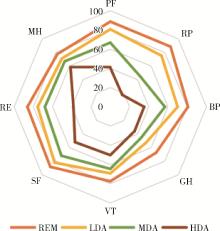
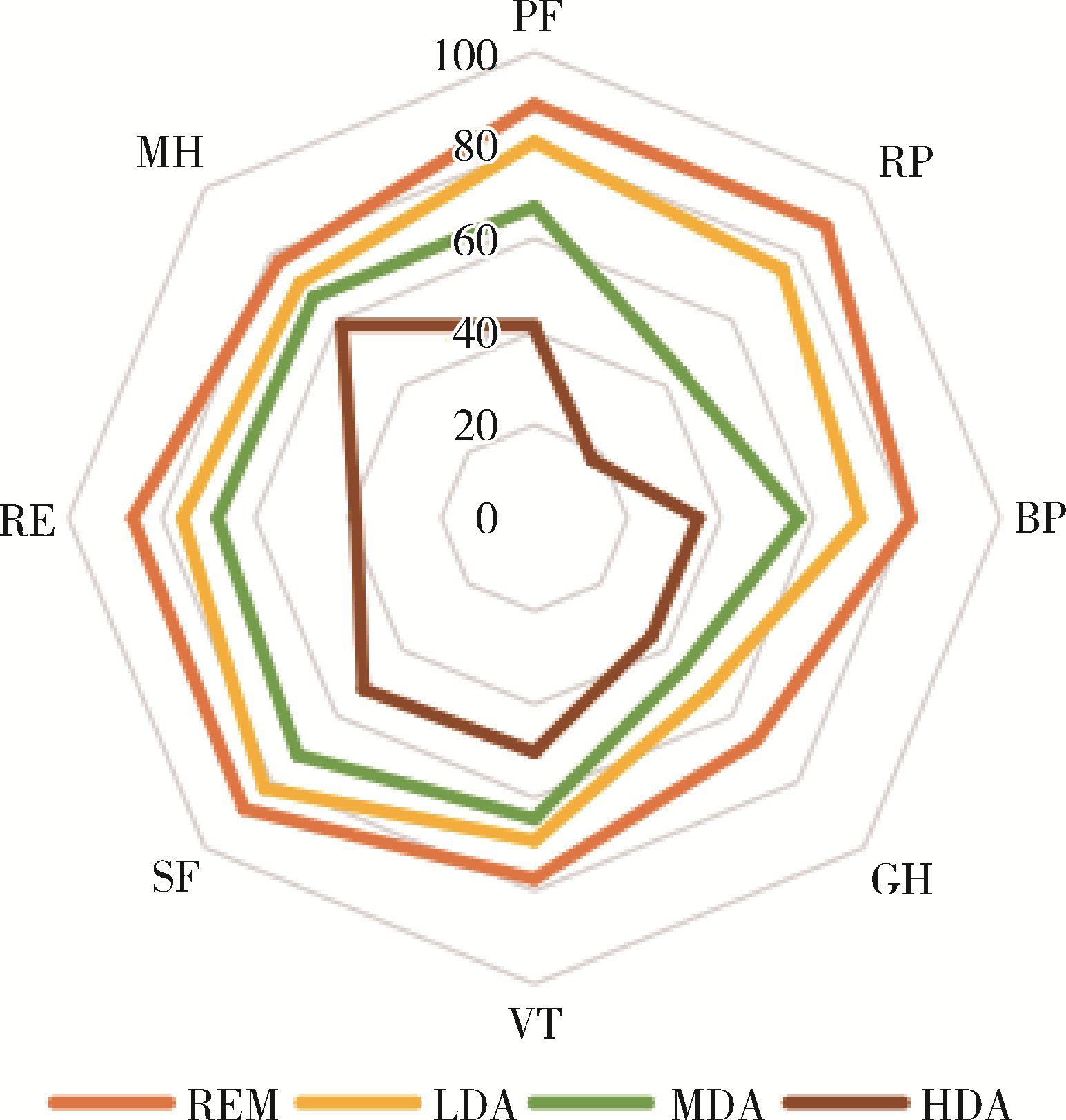
Cross-sectional study on quality of life and disease activity of rheumatoid arthritis patients
Jing-feng ZHANG,Yin-ji JIN,Hui WEI,Zhong-qiang YAO,Jin-xia ZHAO*( )
)
- Department of Rheumatology and Immunology, Peking University Third Hospital, Beijing 100191, China
CLC Number:
- R593.22
| 1 |
Lee DM , Weinblatt ME . Rheumatoid arthritis[J]. Lancet, 2001, 358 (9285): 903- 911.
doi: 10.1016/S0140-6736(01)06075-5 |
| 2 | Lundkvist J , Kastäng F , Kobelt G , et al. The burden of rheumatoid arthritis and access to treatment: Health burden and costs[J]. Eur J Health Econ, 2008, 8 (Suppl 2): S49- S60. |
| 3 |
Li R , Sun J , Ren LM , et al. Epidemiology of eight common rheumatic diseases in China: A large-scale cross-sectional survey in Beijing[J]. Rheumatology (Oxford), 2012, 51 (4): 721- 729.
doi: 10.1093/rheumatology/ker370 |
| 4 | 中华人民共和国国家统计局第二次全国残疾人抽样调查领导小组. 第二次全国残疾人抽样调查主要数据公报[M]. 北京: 中国统计出版社, 2007. |
| 5 | Cunha-Miranda L , Santos H , Ferreira J , et al. Finding rheumatoid arthritis impact on life (FRAIL study): Economic burden[J]. Acta Reumatol Port, 2012, 37 (2): 134- 142. |
| 6 |
de Jong Z , van der Heijde D , McKenna SP , et al. The reliability and construct validity of the RAQoL: A rheumatoid arthritis-specific quality of life instrument[J]. Br J Rheumatol, 1997, 36 (8): 878- 883.
doi: 10.1093/rheumatology/36.8.878 |
| 7 |
Heimans L , Wevers-de Boer KV , Koudijs KK , et al. Health-related quality of life and functional ability in patients with early arthritis during remission steered treatment: Results of the IMPROVED study[J]. Arthritis Res Ther, 2013, 15 (5): R173.
doi: 10.1186/ar4361 |
| 8 |
Marshall S , Haywood K , Fitzpatrick R . Impact of patient-reported outcome measures on routine practice: A structured review[J]. J Eval Clin Pract, 2006, 12 (5): 559- 568.
doi: 10.1111/j.1365-2753.2006.00650.x |
| 9 |
Skevington SM , Day R , Chisholm A , et al. How much do doctors use quality of life information in primary care? Testing the trans-theoretical model of behaviour change[J]. Qual Life Res, 2005, 14 (4): 911- 922.
doi: 10.1007/s11136-004-3710-6 |
| 10 |
Rosa-Goncalves D , Bernardes M , Costa L . Quality of life and functional capacity in patients with rheumatoid arthritis: Cross-sectional study[J]. Reumatol Clin (Engl Ed), 2018, 14 (6): 360- 366.
doi: 10.1016/j.reuma.2017.03.002 |
| 11 |
Gerhold K , Richter A , Schneider M , et al. Health-related quality of life in patients with long-standing rheumatoid arthritis in the era of biologics: Data from the German biologics register RABBIT[J]. Rheumatology, 2015, 54 (10): 1858- 1866.
doi: 10.1093/rheumatology/kev194 |
| 12 |
Zhou YS , Wang XR , An Y , et al. Disability and health-related quality of life in Chinese patients with rheumatoid arthritis: A cross-sectional study[J]. Int J Rheum Dis, 2018, 21 (9): 1709- 1715.
doi: 10.1111/1756-185X.13345 |
| 13 |
Matcham F , Scott IC , Rayner L , et al. The impact of rheumatoid arthritis on quality-of-life assessed using the SF-36: A systematic review and meta-analysis[J]. Semin Arthritis Rheum, 2014, 44 (2): 123- 130.
doi: 10.1016/j.semarthrit.2014.05.001 |
| 14 |
Pencheva DT , Heaney A , McKenna SP , et al. Adaptation and validation of the rheumatoid arthritis quality of life (RAQoL) questionnaire for use in Bulgaria[J]. Rheumatol Int, 2020, 40 (12): 2077- 2083.
doi: 10.1007/s00296-020-04686-2 |
| 15 |
Rupp I , Boshuizen HC , Jacobi CE , et al. Impact of fatigue on health-related quality of life in rheumatoid arthritis[J]. Arthritis Rheum, 2004, 51 (4): 578- 585.
doi: 10.1002/art.20539 |
| 16 |
Bedi GS , Gupta N , Handa R , et al. Quality of life in Indian patients with rheumatoid arthritis[J]. Qual Life Res, 2005, 14 (8): 1953- 1958.
doi: 10.1007/s11136-005-4540-x |
| 17 |
Walker GJ , Littlejohn GO . Measuring quality of life in rheumatic conditions[J]. Clin Rheumatol, 2007, 26 (5): 671- 673.
doi: 10.1007/s10067-006-0450-8 |
| 18 |
Tander B , Cengiz K , Alayli G , et al. A comparative evaluation of health related quality of life and depression in patients with Wbromyalgia syndrome and rheumatoid arthritis[J]. Rheumatol Int, 2008, 28 (9): 859- 865.
doi: 10.1007/s00296-008-0551-6 |
| 19 |
Smolen JS , Aletaha D , Barton A , et al. Rheumatoid arthritis[J]. Nat Rev Dis Primers, 2018, 4, 18001.
doi: 10.1038/nrdp.2018.1 |
| 20 |
Waimann CA , Dal Pra FM , Marengo MF , et al. Quality of life of patients with rheumatoid arthritis in Argentina: Rliability, validity, and sensitivity to change of a Spanish version of the rheumatoid arthritis quality of life questionnaire[J]. Clin Rheumatol, 2012, 31 (7): 1065- 1071.
doi: 10.1007/s10067-012-1976-6 |
| 21 | Chiu YM , Lai MS , Lin HY , et al. Disease activity affects all domains of quality of life in patients with rheumatoid arthritis and is modified by disease duration[J]. Clin Exp Rheumatol, 2014, 32 (6): 898- 903. |
| 22 |
Schmalz G , Noack S , Patschan S , et al. Disease activity, morning stiffness and missing teeth are associated with oral health-related quality of life in individuals with rheumatoid arthritis[J]. Clin Oral Investig, 2020, 24 (10): 3559- 3566.
doi: 10.1007/s00784-020-03226-3 |
| [1] | Dongwu LIU, Jie CHEN, Mingli GAO, Jing YU. Rheumatoid arthritis with Castleman-like histopathology in lymph nodes: A case report [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 928-931. |
| [2] | Huina HUANG,Jing ZHAO,Xiangge ZHAO,Ziran BAI,Xia LI,Guan WANG. Regulatory effect of lactate on peripheral blood CD4+ T cell subsets in patients with rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 519-525. |
| [3] | Xiaofei TANG,Yonghong LI,Qiuling DING,Zhuo SUN,Yang ZHANG,Yumei WANG,Meiyi TIAN,Jian LIU. Incidence and risk factors of deep vein thrombosis in patients with rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 279-283. |
| [4] | Xue ZOU,Xiao-juan BAI,Li-qing ZHANG. Effectiveness of tofacitinib combined with iguratimod in the treatment of difficult-to-treat moderate-to-severe rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1013-1021. |
| [5] | Qi WU,Yue-ming CAI,Juan HE,Wen-di HUANG,Qing-wen WANG. Correlation between dyslipidemia and rheumatoid arthritis associated interstitial lung disease [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 982-992. |
| [6] | Jing-feng ZHANG,Yin-ji JIN,Hui WEI,Zhong-qiang YAO,Jin-xia ZHAO. Correlation analysis between body mass index and clinical characteristics of rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 993-999. |
| [7] | Jin-hui LAI,Qi WANG,Jia-xiang JI,Ming-rui WANG,Xin-wei TANG,Ke-xin XU,Tao XU,Hao HU. Effects of delayed ureteral stents removal during the COVID-19 pandemic on the quality of life and psychological status of postoperative patients with urinary calculi [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 857-864. |
| [8] | Yin-ji JIN,Lin SUN,Jin-xia ZHAO,Xiang-yuan LIU. Significance of IgA isotype of anti-v-raf murine sarcoma viral oncogene homologue B1 antibody in rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 631-635. |
| [9] | Wen-xin CAI,Shi-cheng LI,Yi-ming LIU,Ru-yu LIANG,Jing LI,Jian-ping GUO,Fan-lei HU,Xiao-lin SUN,Chun LI,Xu LIU,Hua YE,Li-zong DENG,Ru LI,Zhan-guo LI. A cross-sectional study on the clinical phenotypes of rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1068-1073. |
| [10] | Fang CHENG,Shao-ying YANG,Xing-xing FANG,Xuan WANG,Fu-tao ZHAO. Role of the CCL28-CCR10 pathway in monocyte migration in rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1074-1078. |
| [11] | Rui LIU,Jin-xia ZHAO,Liang YAN. Clinical characteristics of patients with rheumatoid arthritis complicated with venous thrombosis of lower extremities [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1079-1085. |
| [12] | GAO Chao,CHEN Li-hong,WANG Li,YAO Hong,HUANG Xiao-wei,JIA Yu-bo,LIU Tian. Validation of the Pollard’s classification criteria (2010) for rheumatoid arthritis patients with fibromyalgia [J]. Journal of Peking University (Health Sciences), 2022, 54(2): 278-282. |
| [13] | LOU Xue,LIAO Li,LI Xing-jun,WANG Nan,LIU Shuang,CUI Ruo-mei,XU Jian. Methylation status and expression of TWEAK gene promoter region in peripheral blood of patients with rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2021, 53(6): 1020-1025. |
| [14] | ZHONG Hua,XU Li-ling,BAI Ming-xin,SU Yin. Effect of chemokines CXCL9 and CXCL10 on bone erosion in patients with rheumatoid arthritis [J]. Journal of Peking University (Health Sciences), 2021, 53(6): 1026-1031. |
| [15] | LUO Liang,HUO Wen-gang,ZHANG Qin,LI Chun. Clinical characteristics and risk factors of rheumatoid arthritis with ulcerative keratitis [J]. Journal of Peking University (Health Sciences), 2021, 53(6): 1032-1036. |
|
||