Journal of Peking University (Health Sciences) ›› 2023, Vol. 55 ›› Issue (1): 133-138. doi: 10.19723/j.issn.1671-167X.2023.01.020
Previous Articles Next Articles
Reinforced radiculoplasty for the treatment of symptomatic sacral Tarlov cysts: A clinical analysis of 71 cases
Chao WU1,Bin LIU1,*( ),Jing-cheng XIE1,Zhen-yu WANG1,Chang-cheng MA1,Jun YANG1,Jian-jun SUN1,Xiao-dong CHEN1,Tao YU1,Guo-zhong LIN1,Yu SI1,Yun-feng HAN1,Su-hua CHEN1,Xiao-liang YIN1,Qian-quan MA1,Mu-tian ZHENG1,Lin ZENG2
),Jing-cheng XIE1,Zhen-yu WANG1,Chang-cheng MA1,Jun YANG1,Jian-jun SUN1,Xiao-dong CHEN1,Tao YU1,Guo-zhong LIN1,Yu SI1,Yun-feng HAN1,Su-hua CHEN1,Xiao-liang YIN1,Qian-quan MA1,Mu-tian ZHENG1,Lin ZENG2
- 1. Department of Neurosurgery, Peking University Third Hospital, Beijing 100191, China
2. Clinical Epidemiology Research Center, Peking University Third Hospital, Beijing 100191, China
CLC Number:
- R651.2
| 1 | Kozowski P , Kalinowski P , Jankiewicz M , et al. Perineural cysts[J]. Pol Merkur Lekarski, 2018, 45 (269): 201- 204. |
| 2 |
Nabors MW , Pait TG , Byrd EB , et al. Updated assessment and current classification of spinal meningeal cysts[J]. J Neurosurg, 1988, 68 (3): 366- 377.
doi: 10.3171/jns.1988.68.3.0366 |
| 3 |
Sharma M , SirDeshpande P , Ugiliweneza B , et al. A systematic comparative outcome analysis of surgical versus percutaneous techniques in the management of symptomatic sacral perineural (Tarlov) cysts: A meta-analysis[J]. J Neurosurg Spine, 2019, 30 (5): 623- 634.
doi: 10.3171/2018.10.SPINE18952 |
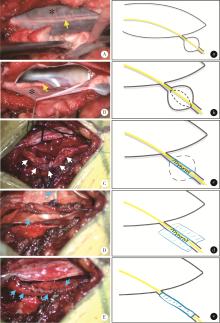
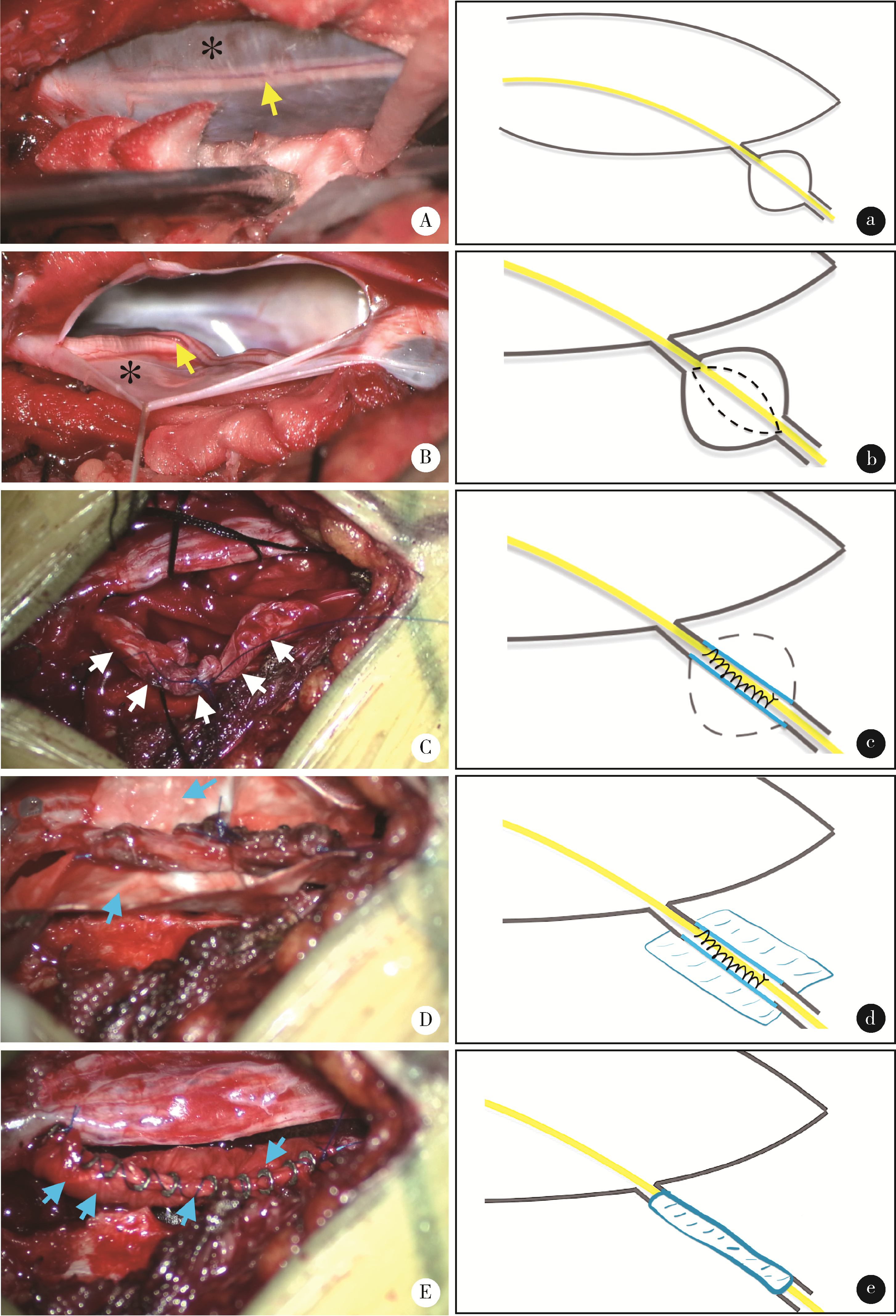
| 4 | Sugawara T , Higashiyama N , Tamura S , et al. Novel wrapping surgery for symptomatic sacral perineural cysts[J]. J Neurosurg Spine, 2021, 36 (2): 185- 192. |
| 5 |
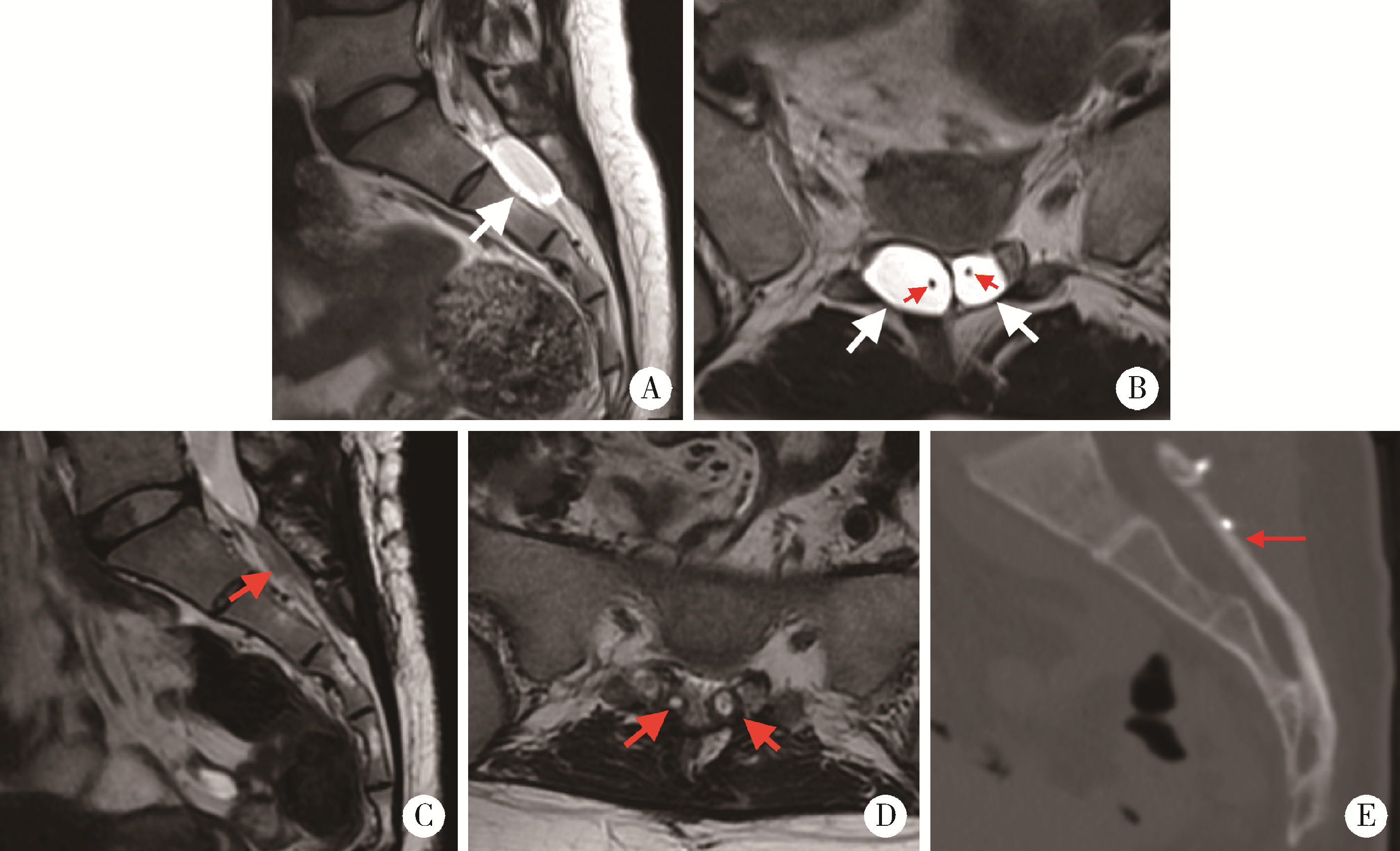
Liu B , Wang Z , Lin G , et al. Radiculoplasty with reconstruction using 3D-printed artificial dura mater for the treatment of sympto-matic sacral canal cysts: Two case reports[J]. Medicine (Baltimore), 2018, 97 (49): e13289.
doi: 10.1097/MD.0000000000013289 |
| 6 |
刘彬, 王振宇, 谢京城, 等. 显微手术治疗骶管囊肿43例临床分析[J]. 中国微创外科杂志, 2017, 17 (12): 1104- 1108.
doi: 10.3969/j.issn.1009-6604.2017.12.015 |
| 7 |
Paterakis K , Brotis A , Bakopoulou M , et al. A giant Tarlov cyst presenting with hydronephrosis in a patient with Marfan syndrome: A case report and review of the literature[J]. World Neurosurg, 2019, 126, 581- 587.
doi: 10.1016/j.wneu.2019.02.222 |
| 8 |
Henderson FC Sr , Austin C , Benzel E , et al. Neurological and spinal manifestations of the Ehlers-Danlos syndromes[J]. Am J Med Genet C Semin Med Genet, 2017, 175 (1): 195- 211.
doi: 10.1002/ajmg.c.31549 |
| 9 |
Tarlov IM . Cysts of the sacral nerve roots: Clinical significance and pathogenesis[J]. AMA Arch Neurol Psychiatry, 1952, 68 (1): 94- 108.
doi: 10.1001/archneurpsyc.1952.02320190100010 |
| 10 |
Marino D , Carluccio MA , Di Donato I , et al. Tarlov cysts: Clinical evaluation of an Italian cohort of patients[J]. Neurol Sci, 2013, 34 (9): 1679- 1682.
doi: 10.1007/s10072-013-1321-0 |
| 11 |
Hulens M , Rasschaert R , Bruyninckx F , et al. Symptomatic Tarlov cysts are often overlooked: Ten reasons why. A narrative review[J]. Eur Spine J, 2019, 28 (10): 2237- 2248.
doi: 10.1007/s00586-019-05996-1 |
| 12 |
Yang AI , Rinehart CD , McShane BJ , et al. Growth of lumbosacral perineural (Tarlov) cysts: A natural history analysis[J]. Neurosurgery, 2020, 86 (1): 88- 92.
doi: 10.1093/neuros/nyy586 |
| 13 |
Galarza M , Chaban G , Gazzeri R , et al. Functional recovery following resection of large Tarlov cyst malformation: A multicentre longitudinal cohort study[J]. Acta Neurochir (Wien), 2021, 163 (10): 2769- 2776.
doi: 10.1007/s00701-021-04817-z |
| 14 |
Lim VM , Khanna R , Kalinkin O , et al. Evaluating the discordant relationship between Tarlov cysts and symptoms of pudendal neuralgia[J]. Am J Obstet Gynecol, 2020, 222 (1): 70.e1- 70.e6.
doi: 10.1016/j.ajog.2019.07.021 |
| 15 | Yucesoy K, Yilmaz M, Kaptan H, et al. A novel surgical technique for treatment of symptomatic Tarlov cysts[J/OL]. Br J Neurosurg, (2021-12-21)[2022-01-16]. https://doi.org/10.1080/02688697.2021.2016623. |
| 16 |
中华医学会神经外科学分会. 骶管囊肿诊治专家共识[J]. 中华神经外科杂志, 2019, 35 (4): 325- 329.
doi: 10.3760/cma.j.issn.1001-2346.2019.04.001 |
| 17 |
Cheng SJ , Hakkinen I , Zhang P , et al. Paradoxical headache in a case of chronic spontaneous intracranial hypotension and multiple perineural cysts[J]. Headache, 2021, 61 (8): 1291- 1294.
doi: 10.1111/head.14188 |
| 18 |
Sharma M , SirDeshpande P , Ugiliweneza B , et al. A systematic comparative outcome analysis of surgical versus percutaneous techniques in the management of symptomatic sacral perineural (Tarlov) cysts: A meta-analysis[J]. J Neurosurg Spine, 2019, 30 (5): 623- 634.
doi: 10.3171/2018.10.SPINE18952 |
| 19 |
Murphy K , Oaklander AL , Elias G , et al. Treatment of 213 patients with symptomatic Tarlov cysts by CT-guided percutaneous injection of fibrin sealant[J]. AJNR Am J Neuroradiol, 2016, 37 (2): 373- 379.
doi: 10.3174/ajnr.A4517 |
| 20 | Soon WC , Sun R , Czyz M . Haemorrhagic Tarlov cyst: A rare complication of anticoagulation therapy[J]. Oxf Med Case Reports, 2021, (8): omab063. |
| 21 | 文泽贤, 储卫华, 叶信珍, 等. 显微填塞治疗症状性骶管囊肿的长期疗效[J]. 中国微侵袭神经外科杂志, 2017, 22 (4): 172- 175. |
| 22 |
Potts MB , McGrath MH , Chin CT , et al. Microsurgical fenestration and paraspinal muscle pedicle flaps fort the treatment of symptomatic sacral Tarlov cysts[J]. World Neurosurg, 2016, 86, 233- 242.
doi: 10.1016/j.wneu.2015.09.055 |
| 23 |
Burke JF , Thawani JP , Berger I , et al. Microsurgical treatment of sacral perineural (Tarlov) cysts: Case series and review of the literature[J]. J Neurosurg Spine, 2016, 24 (5): 700- 707.
doi: 10.3171/2015.9.SPINE153 |
| 24 |
Medani K , Lawandy S , Schrot R , et al. Surgical management of symptomatic Tarlov cysts: Cyst fenestration and nerve root imbrication. A single institutional experience[J]. J Spine Surg, 2019, 5 (4): 496- 503.
doi: 10.21037/jss.2019.11.11 |
| 25 |
Tsitsopoulos PP , Marklund N , Salci K , et al. Management of symptomatic sacral perineural cysts with microsurgery and a vascularized fasciocutaneous flap[J]. J Spine Surg, 2018, 4 (3): 602- 609.
doi: 10.21037/jss.2018.07.02 |
| 26 | 程诚, 尚爱加, 唐红, 等. 显微切除并脂肪填塞治疗骶管囊肿的临床应用[J]. 中国临床神经外科杂志, 2018, 23 (5): 350- 351. |
| 27 |
修波, 李萃萃, 林和璞, 等. 脂肪块封堵囊颈术治疗骶管Tarlov囊肿[J]. 中华神经外科杂志, 2018, 34 (11): 1119- 1122.
doi: 10.3760/cma.j.issn.1001-2346.2018.11.010 |
| 28 | 朱含硕, 沈霖, 陈正, 等. 漏口内口封堵并带蒂肌瓣填塞治疗症状性骶管囊肿的疗效分析[J]. 中国临床神经外科杂志, 2020, 25 (5): 274- 276. |
| 29 |
林国中, 王振宇, 刘斌. 神经电生理监测技术在椎管内病变术中的应用[J]. 北京大学学报(医学版), 2012, 44 (5): 776- 779.
doi: 10.3969/j.issn.1671-167X.2012.05.021 |
| 30 | 林国中, 王振宇, 谢京城, 等. 内含终丝的骶管囊肿21例临床研究[J]. 北京大学学报(医学版), 2020, 52 (3): 583- 585. |
| [1] | Guo-zhong LIN,Jing-cheng XIE,Xiao-dong CHEN,Jun YANG. Classification and microsurgical treatment of primary tethered cord syndrome in adults [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 641-645. |
| [2] | Bin CHEN,Chao WU,Bin LIU,Tao YU,Zhen-yu WANG. Prognosis of patients with spinal intramedullary cavernous hemangioma by different treatments [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 652-657. |
| [3] | Jing-cheng XIE,Xiao-dong CHEN,Jun YANG. Diagnosis and surgical treatment of tethered cord syndrome accompanied by congenital dermal sinus tract in adults [J]. Journal of Peking University (Health Sciences), 2022, 54(6): 1163-1166. |
| [4] | Guo-zhong LIN,Zhen-yu WANG,Jing-cheng XIE,Bin LIU,Chang-cheng MA,Xiao-dong CHEN. Clinical study of 21 cases of sacral cysts containing fila terminale [J]. Journal of Peking University (Health Sciences), 2020, 52(3): 582-585. |
| [5] | . [J]. Journal of Peking University(Health Sciences), 2016, 48(2): 191-193. |
|
||