Journal of Peking University (Health Sciences) ›› 2025, Vol. 57 ›› Issue (5): 836-840. doi: 10.19723/j.issn.1671-167X.2025.05.004
Previous Articles Next Articles
Current situation and exploration of clinical transformation of plasmatrix in oral implantology
Yulan WANG, Hao ZENG, Yufeng ZHANG*( )
)
- Department of Implantology, School and Hospital of Stomatology, Wuhan University, Wuhan 430079, China
CLC Number:
- R783.6
| 1 |
|
| 2 |
doi: 10.1002/JPER.22-0196 |
| 3 |
|
| 4 |
|
| 5 |
doi: 10.1111/cid.12343 |
| 6 |
|
| 7 |
Farshidfar N, Apaza Alccayhuaman KA, Estrin NE, et al. Advantages of horizontal centrifugation of platelet-rich fibrin in regenerative medicine and dentistry[J/OL]. Periodontol 2000, 2025. [2025-03-25]. http://doi.org/10.1111/prd.12625.
|
| 8 |
张玉峰. 血浆基质制品的前世今生[J]. 中华口腔医学杂志, 2021, 56 (8): 740- 746.
|
| 9 |
doi: 10.1089/ten.teb.2016.0233 |
| 10 |
Farshidfar N, Amiri MA, Estrin NE, et al. Platelet-rich plasma (PRP) versus injectable platelet-rich fibrin (i-PRF): A syste-matic review across all fields of medicine[J/OL]. Periodontol 2000, 2025. [2025-03-24]. http://doi.org/10.1111/prd.12626.
|
| 11 |
doi: 10.1016/j.biopha.2023.115795 |
| 12 |
doi: 10.1002/jper.11364.Onlineaheadofprint |
| 13 |
doi: 10.1016/j.acthis.2023.152059 |
| 14 |
doi: 10.1002/jbm.a.36792 |
| 15 |
doi: 10.1111/prd.12538 |
| 16 |
doi: 10.1007/s00784-023-05108-w |
| 17 |
|
| 18 |
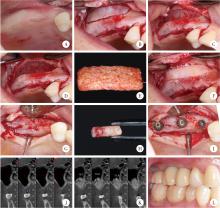
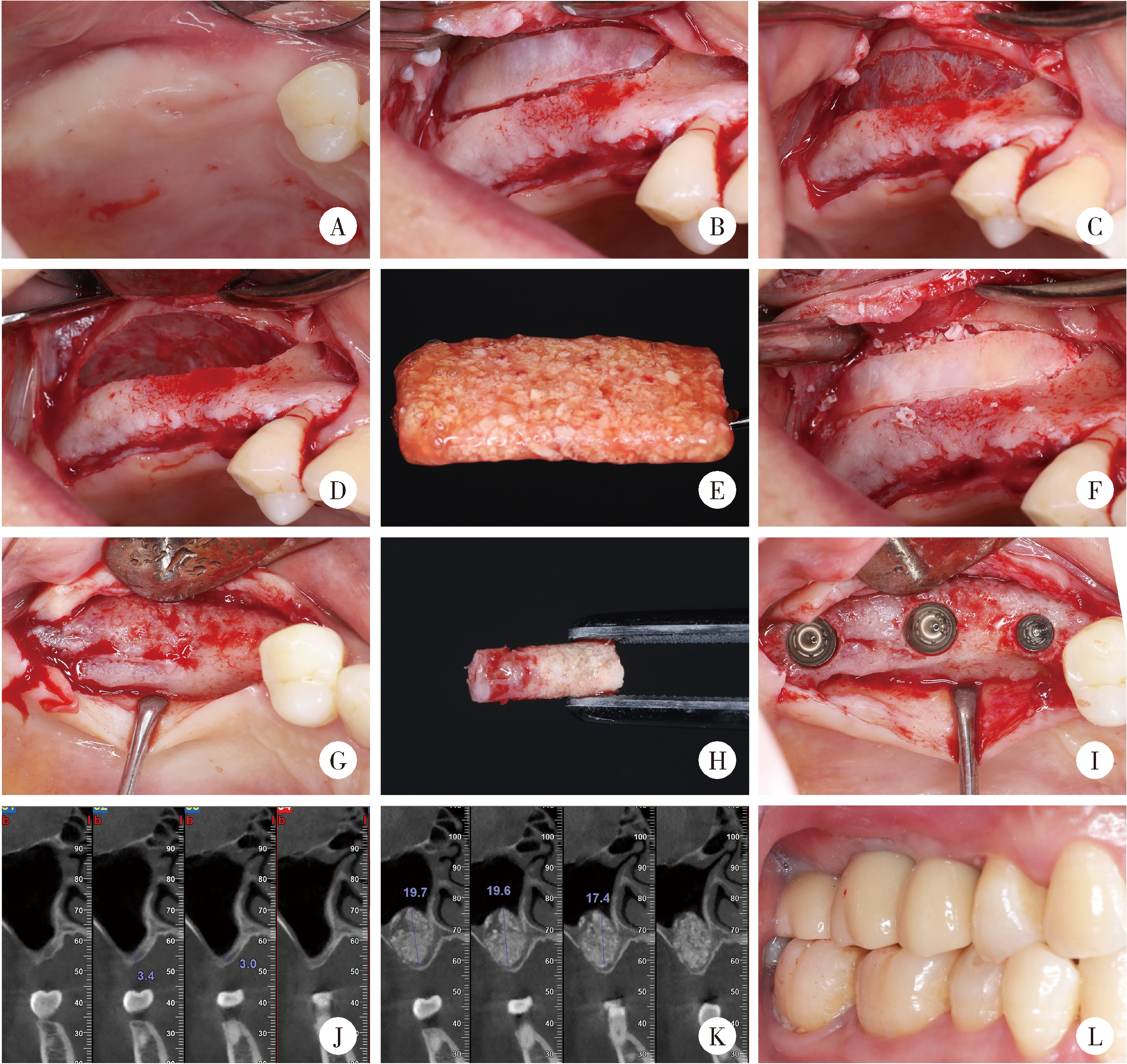
张玉峰, 王宇蓝. 血浆基质在口腔种植垂直骨增量中的应用[J]. 口腔疾病防治, 2022, 30 (12): 837- 843.
|
| 19 |
张玉峰, 王宇蓝. 血浆基质在口腔种植水平骨增量中的应用[J]. 口腔疾病防治, 2022, 30 (3): 153- 159.
|
| 20 |
doi: 10.12998/wjcc.v11.i11.2396 |
| 21 |
doi: 10.1186/s12903-020-1023-y |
| 22 |
张玉峰, 张晓欣. 血浆基质在牙槽嵴保存术中的应用[J]. 口腔疾病防治, 2024, 32 (3): 161- 168.
|
| 23 |
|
| 24 |
doi: 10.1111/prd.12609 |
| 25 |
王宇蓝, 曾浩, 夏婷, 等. 骨致密化技术联合血浆基质在穿牙槽嵴上颌窦底提升中的应用[J]. 中国口腔种植学杂志, 2025, 30 (2): 106- 110.
|
| 26 |
张晓欣, 张玉峰. 上颌窦底骨量不足新分类及血浆基质治疗策略[J]. 口腔生物医学, 2021, 12 (4): 215- 218.
|
| 27 |
doi: 10.1007/s00784-025-06198-4 |
| 28 |
doi: 10.1111/clr.14053 |
| 29 |
doi: 10.1186/s12903-023-03228-z |
| 30 |
doi: 10.1002/cap.10202 |
| 31 |
doi: 10.12998/wjcc.v9.i4.960 |
| 32 |
doi: 10.11607/prd.2505 |
| 33 |
doi: 10.1111/jre.12568 |
| 34 |
doi: 10.1016/j.joms.2020.02.019 |
| 35 |
doi: 10.1111/cid.12661 |
| 36 |
|
| 37 |
doi: 10.1590/1678-7757-2023-0294 |
| 38 |
doi: 10.1088/1748-605X/acbad5 |
| 39 |
doi: 10.1007/s00784-022-04510-0 |
| 40 |
|
| 41 |
张玉峰. 数字化骨块在骨增量中的应用[J]. 中华口腔医学杂志, 2023, 58 (4): 312- 317.
|
| [1] | Ziyang YU, Houzuo GUO, Xi JIANG, Weihua HAN, Ye LIN. Imaging study of osteogenesis in maxillary sinus segment of zygomatic implants [J]. Journal of Peking University (Health Sciences), 2025, 57(5): 967-974. |
| [2] | Fangru LIN, Zhihui TANG. Correlation analysis of peri-implant health after single-tooth dental implant [J]. Journal of Peking University (Health Sciences), 2025, 57(2): 347-353. |
| [3] | Juan WANG, Lixin QIU, Huajie YU. Influence of emergence profile designs on the peri-implant tissue in the mandibular molar: A randomized controlled trial [J]. Journal of Peking University (Health Sciences), 2025, 57(1): 65-72. |
| [4] | Congwei WANG,Min GAO,Yao YU,Wenbo ZHANG,Xin PENG. Clinical analysis of denture rehabilitation after mandibular fibula free-flap reconstruction [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 66-73. |
| [5] | Qian DING,Wen-jin LI,Feng-bo SUN,Jing-hua GU,Yuan-hua LIN,Lei ZHANG. Effects of surface treatment on the phase and fracture strength of yttria- and magnesia-stabilized zirconia implants [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 721-728. |
| [6] | Fei SUN,Jian LIU,Si-qi LI,Yi-ping WEI,Wen-jie HU,Cui WANG. Profiles and differences of submucosal microbial in peri-implantitis and health implants: A cross-sectional study [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 30-37. |
| [7] | LI Yi,YU Hua-jie,QIU Li-xin. Clinical classification and treatment decision of implant fracture [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 126-133. |
| [8] | LI Peng,PIAO Mu-zi,HU Hong-cheng,WANG Yong,ZHAO Yi-jiao,SHEN Xiao-jing. Radiography study on osteotome sinus floor elevation with placed implant simultaneously with no graft augmentation [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 95-101. |
| [9] | Zhong ZHANG,Huan-xin MENG,Jie HAN,Li ZHANG,Dong SHI. Effect of vertical soft tissue thickness on clinical manifestation of peri-implant tissue in patients with periodontitis [J]. Journal of Peking University (Health Sciences), 2020, 52(2): 332-338. |
| [10] | Chun-ping LIN,Song-he LU,Jun-xin ZHU,Hong-cheng HU,Zhao-guo YUE,Zhi-hui TANG. Influence of thread shapes of custom-made root-analogue implants on stress distribution of peri-implant bone: A three-dimensional finite element analysis [J]. Journal of Peking University(Health Sciences), 2019, 51(6): 1130-1137. |
| [11] | Qian WANG,Dan LI,Zhi-hui TANG. Sinus floor elevation and simultaneous dental implantation: A long term retrospective study of sinus bone gain [J]. Journal of Peking University(Health Sciences), 2019, 51(5): 925-930. |
| [12] | Xiao-qian LIU,Qiu-wen CHEN,Hai-lan FENG,Bing WANG,Jian QU,Zhen SUN,Mo-di HENG,Shao-xia PAN. Oral hygiene maintenance of locator attachments implant overdentures in edentulous population: A longitudinal study [J]. Journal of Peking University(Health Sciences), 2019, 51(1): 136-144. |
| [13] | Zhi-yong△ ZHANG,Tian MENG,Quan CHEN,Wen-shu LIU,Yu-huan CHEN. Retrospective analysis of early dental implant failure [J]. Journal of Peking University(Health Sciences), 2018, 50(6): 1088-1091. |
| [14] | LIU Jing-yin, CHEN Fei, GE Yan-jun, WEI Ling, PAN Shao-xia, FENG Hai-lan. Influence of implants prepared by selective laser melting on early bone healing [J]. Journal of Peking University(Health Sciences), 2018, 50(1): 117-122. |
| [15] | LIANG Nai-wen, SHI Lei,HUANG Ying,DENG Xu-liang. Role of different scale structures of titanium implant in the biological behaviors of human umbilical vein endothelial cells [J]. Journal of Peking University(Health Sciences), 2017, 49(1): 43-048. |
|
||