北京大学学报(医学版) ›› 2019, Vol. 51 ›› Issue (5): 875-880. doi: 10.19723/j.issn.1671-167X.2019.05.014
股骨近端病理性骨折患者围手术期的临床特征分析
- 北京大学第一医院骨科, 北京 100034
Perioperative clinical characteristics of patients with pathological fracture of proximal femur
Yun-peng CUI,Chuan MI,Bing WANG,Yuan-xing PAN,Yun-fei LIN,Xue-dong SHI( )
)
- Department of Orthopaedics, Peking University First Hospital, Beijing 100034, China
摘要:
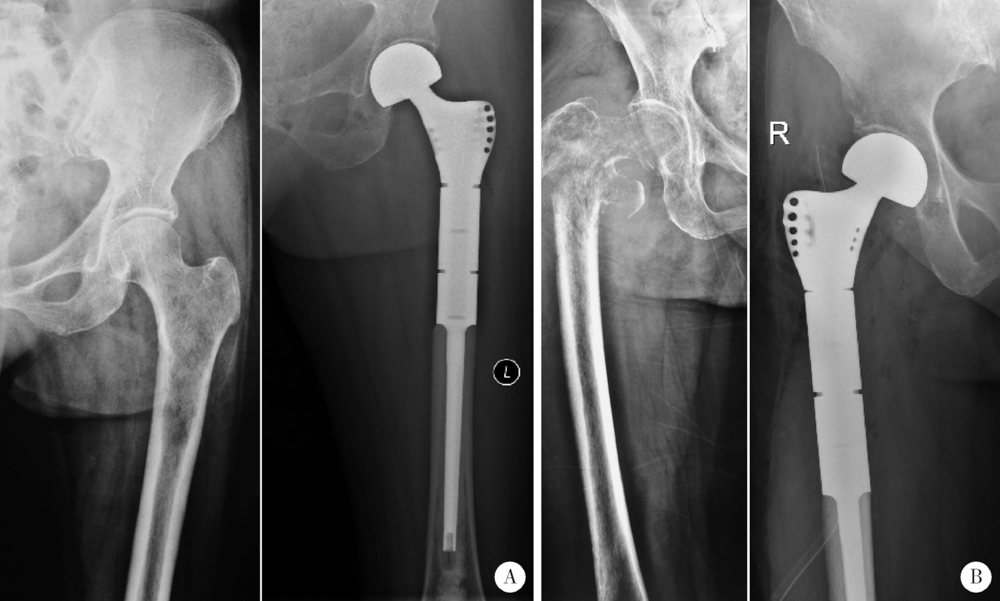
目的:分析股骨近端恶性肿瘤导致病理性骨折患者的围手术期临床特征,探讨病理性骨折对患者股骨近端假体置换围手术期治疗的影响。方法:回顾性分析北京大学第一医院骨科2011年1月至2017年2月期间收治的因股骨近端恶性肿瘤行股骨近端扩大切除、肿瘤半髋关节置换手术的患者共28例。根据骨折情况将患者分为骨折组和非骨折组,对比两组患者围手术期临床特征。结果:骨折患者占50.0%,两组间不同年龄、性别、受累肢体以及肿瘤病理类型间的差异无统计学意义。术前两组患者血红蛋白浓度、红细胞压积、下肢血栓间的差异无统计学意义(P>0.05),骨折组患者白蛋白低于非骨折组,差异有统计学意义(P=0.031)。两组患者术中出血、手术时间的差异无统计学意义(P>0.05)。两组患者术后第1天患者血红蛋白浓度、红细胞压积、白蛋白下降程度,以及术后引流管留置时间、术后引流总量、术后下地时间、术后住院日的差异无统计学意义(P>0.05)。术后第7天,骨折组患者血红蛋白浓度(P=0.025)、红细胞压积(P=0.039)低于非骨折组,差异有统计学意义。术中、术后7天内骨折组患者需输血的人数均多于非骨折组患者(术中:7/14 vs. 1/14,P=0.033;术后7天内:8/14 vs. 1/14,P=0.013)。以Gross公式计算围手术期总失血量(术后7天内),骨折组患者高于非骨折组患者[(2 066.3±419.8) mL vs. (786.0±152.6) mL, P=0.039]。骨折组患者术前Barthel日常生活能力评分低于非骨折组(P=0.009),视觉模拟评分(visual analogue scale,VAS)高于非骨折组(P<0.001),出院前两组患者上述评分间差异无统计学意义(P>0.05)。结论:股骨近端病理性骨折的患者围手术期白蛋白低,病理性骨折不增加患者手术时间、术中出血量以及围手术期功能恢复情况,但是骨折组患者围手术期的总失血量多于非骨折组患者,术后血红蛋白浓度、红细胞压积低于非骨折组,骨折组患者术中、术后需输血治疗的人数多于非骨折组。
中图分类号:
- R683.42
| [1] | Sumathi VP, Jeys L, Legdeur N . Metastatic tumours of bone[J]. Surgery (Oxford), 2012,30(2):80-85. |
| [2] | Costa L, Badia X, Chow E , et al. Impact of skeletal complications on patients’ quality of life, mobility, and functional independence[J]. Support Care Cancer, 2008,16(10):879-889. |
| [3] | Harvey N, Ahlmann ER, Allison DC , et al. Endoprostheses last longer than intramedullary devices in proximal femur metastases[J]. Clin Orthop Relat Res, 2012,470(3):684-691. |
| [4] | 杨毅, 郭卫, 尉然 . 两种方式重建股骨近端转移癌患者的围手术期安全性比较[J]. 中国骨与关节外科, 2013,6(3):214-218. |
| [5] | Steensma M, Boland PJ, Morris CD , et al. Endoprosthetic treatment is more durable for pathologic proximal femur fractures[J]. Clin Orthop Relat Res, 2012,470(3):920-926. |
| [6] | Wedin R, Bauer HC . Surgical treatment of skeletal metastatic lesions of the proximal femur: endoprosjournal or reconstruction nail?[J]. J Bone Joint Surg, 2005,87(12):1653-1657. |
| [7] | Ratasvuori M, Wedin R, Hansen BH , et al. Prognostic role of en-bloc resection and late onset of bone metastasis in patients with bone-seeking carcinomas of the kidney, breast, lung, and prostate: SSG study on 672 operated skeletal metastases[J]. J Surg Oncol, 2014,110(4):360-365. |
| [8] | Hobusch GM, Bollmann J, Puchner SE , et al. What sport activity levels are achieved in patients after resection and endoprosthetic reconstruction for a proximal femur bone sarcoma?[J]. Clin Orthop Relat Res, 2016,475(3):1-10. |
| [9] | Guzik G . Treatment outcomes and quality of life after the implantation of modular prostheses of the proximal femur in patients with cancer metastases[J]. Ortop Traumatol Rehabil, 2016,18(3):231-238. |
| [10] | Peterson JR, O’Connor IT, Topfer J, et al. Functional results and complications with long stem hemiarthroplasty in patients with metastases to the proximal femur[J]. J Am Coll Surgeons, 2016,223(4):e150. |
| [11] | Calabró T, Rooyen RV, Piraino I , et al. Reconstruction of the proximal femur with a modular resection prosjournal[J]. Eur J Orthop Surg Traumatol, 2016,26(4):415-421. |
| [12] | Peterson JR, Decilveo AP, O’Connor IT, et al. What are the functional results and complications with long stem hemiarthroplasty in patients with metastases to the proximal femur?[J]. Clin Ortho Relat Res, 2017,475(3):745-756. |
| [13] | Houdek MT, Watts CD, Wyles CC , et al. Functional and oncologic outcome of cemented endoprosjournal for malignant proximal femoral tumors[J]. J Surg Oncol, 2016,114(4):501-506. |
| [14] | Thambapillary S, Dimitriou R, Makridis KG , et al. Implant longevity, complications and functional outcome following proximal femoral arthroplasty for musculoskeletal tumors: a systematic review[J]. J Arthroplasty, 2013,28(8):1381-1385. |
| [15] | Janssen SJ, Teunis T, Hornicek FJ , et al. Outcome after fixation of metastatic proximal femoral fractures: A systematic review of 40 studies[J]. J Surg Oncol, 2016,114(4):507-519. |
| [16] | Houdek MT, Wyles CC, Labott JR , et al. Durability of hemiarthroplasty for pathologic proximal femur fractures[J]. J Arthroplasty, 2017,32(12):3607-3610. |
| [17] | Zoccali C, Attala D, Uccio ASD , et al. The dual mobility cup in muscular skeletal oncology: rationale and indications[J]. Int Orthop, 2017,41(3):447-453. |
| [18] | Gross JB . Estimating allowable blood loss: corrected for dilution[J]. Anesthesiology, 1983,58(3):277-280. |
| [19] | Liu X, Zhang X, Chen Y , et al. Hidden blood loss after total hip arthroplasty[J]. J Arthroplasty, 2011,26(7):1100-1105. |
| [20] | Kumar A, Torres ML, Cliby WA , et al. Inflammatory and nutritional serum markers as predictors of peri-operative morbidity and survival in ovarian cancer[J]. Anticancer Res, 2017,37(7):3673-3677. |
| [21] | Goh SL, De Silva RP, Dhital K , et al. Is low serum albumin associated with postoperative complications in patients undergoing oesophagectomy for oesophageal malignancies?[J]. Interact Cardiovasc Thorac Surg, 2015,20(1):107-113. |
| [22] | Musallam KM, Tamim HM, Richards T , et al. Preoperative anaemia and postoperative outcomes in non-cardiac surgery: a retrospective cohort study[J]. Lancet, 2011,378(9800):1396-1407. |
| [23] | Fowler AJ, Ahmad T, Phull MK , et al. Meta-analysis of the association between preoperative anaemia and mortality after surgery[J]. Br J Surg, 2015,102(11):1314-1324. |
| [24] | Rasouli MR, Restrepo C, Maltenfort MG , et al. Risk factors for surgical site infection following total joint arthroplasty[J]. J Bone Joint Surg Am, 2014,96(18):e158. |
| [25] | 周宗科, 翁习生, 向兵 , 等. 中国髋、膝关节置换术加速康复——围术期贫血诊治专家共识[J]. 中华骨与关节外科杂志, 2016,9(1):10-15. |
| [26] | Mirels H . Metastatic disease in long bones. A proposed scoring system for diagnosing impending pathologic fractures[J]. Clin Orthop Relat Res, 1989,249:256-264. |
| [27] | Damron TA, Morgan H, Prakash D , et al. Critical evaluation of Mirels’ rating system for impending pathologic fractures[J]. Clin Orthop Relat Res, 2003(415 Suppl):S201-S207. |
| [28] | Damron TA, Nazarian A, Entezari V , et al. CT-based structural rigidity analysis is more accurate than Mirels scoring for fracture prediction in metastatic femoral lesions[J]. Clin Orthop Relat Res, 2016,474(3):643-651. |
| [29] | Ulaner GA, Zindman AM, Zheng J , et al. FDG PET/CT assesses the risk of femoral pathological fractures in patients with metastatic breast cancer[J]. Clin Nucl Med, 2017,42(4):264-270. |
| [1] | 刘园梅, 傅义程, 郝靖欣, 张福春, 刘慧琳. 老年髋部骨折患者住院期间发生术后心力衰竭的列线图预测模型的构建及验证[J]. 北京大学学报(医学版), 2024, 56(5): 874-883. |
| [2] | 乔佳佳,田聪,黄晓波,刘军. 肾结石合并系统性红斑狼疮行经皮肾镜碎石取石术的安全性和有效性评估[J]. 北京大学学报(医学版), 2024, 56(4): 745-749. |
| [3] | 白心竹,何金徽,陆松松,李春,王依林,熊建. 椎体骨折合并活化部分凝血活酶时间延长1例[J]. 北京大学学报(医学版), 2024, 56(2): 371-374. |
| [4] | 刘想,谢辉辉,许玉峰,张晓东,陶晓峰,柳林,王霄英. 人工智能对提高放射科住院医生诊断胸部肋骨骨折一致性的价值[J]. 北京大学学报(医学版), 2023, 55(4): 670-675. |
| [5] | 熊士凯,史尉利,王安鸿,谢兴,郭秦炜. 腓骨远端撕脱骨折的影像学诊断:踝关节X线与CT三维重建的比较[J]. 北京大学学报(医学版), 2023, 55(1): 156-159. |
| [6] | 侯国进,周方,田耘,姬洪全,张志山,郭琰,吕扬,杨钟玮. 外侧锁定接骨板治疗股骨远端骨折术后翻修的相关影响因素[J]. 北京大学学报(医学版), 2022, 54(6): 1172-1177. |
| [7] | 姜保国,张培训. 老年髋部骨折的围手术期风险评估[J]. 北京大学学报(医学版), 2022, 54(5): 803-809. |
| [8] | 周伟,安金刚,荣起国,张益. 下颌骨颏部骨折联合双侧髁突囊内骨折致伤机制的三维有限元分析[J]. 北京大学学报(医学版), 2021, 53(5): 983-989. |
| [9] | 王建伟,徐啸,鲍正清,刘振华,何峰,黄广林,满立波. 耻骨下缘部分切除辅助后尿道吻合术在男性骨盆骨折后尿道离断修复中的应用[J]. 北京大学学报(医学版), 2021, 53(4): 798-802. |
| [10] | 侯国进,周方,田耘,姬洪全,张志山,郭琰,吕扬,杨钟玮,张雅文. 后路短节段跨伤椎椎弓根螺钉固定治疗胸腰段爆裂骨折术后再发后凸的危险因素[J]. 北京大学学报(医学版), 2021, 53(1): 167-174. |
| [11] | 刘中砥,许庭珉,党育,张殿英,付中国. 有限切开复位髓内外联合固定技术治疗股骨转子下骨折的临床随访[J]. 北京大学学报(医学版), 2020, 52(6): 1102-1106. |
| [12] | 王建伟,满立波,徐啸,刘振华,何峰,黄广林,翟建坡,周宁,李玮. 耻骨会阴联合切口后尿道吻合术治疗复杂男性骨盆骨折后尿道离断[J]. 北京大学学报(医学版), 2020, 52(4): 646-650. |
| [13] | 郭辅政,朱凤雪,邓玖旭,杜哲,赵秀娟. 严重多发伤患者机械通气的危险因素分析[J]. 北京大学学报(医学版), 2020, 52(4): 738-742. |
| [14] | 张鹏,贾波,陈逍堃,王宇,黄伟,赖人杰,王志伟,熊建,王天兵. 尺骨茎突与乙状切迹骨折对桡骨远端骨折患者术后腕关节功能的影响[J]. 北京大学学报(医学版), 2020, 52(3): 578-581. |
| [15] | 刘冰川,孙川,邢永,周方,田耘,姬洪全,张志山,郭琰,吕扬,杨钟玮,侯国进,高山. 中青年股骨颈骨折内固定术后发生缺血性股骨头坏死的相关因素[J]. 北京大学学报(医学版), 2020, 52(2): 290-297. |
|
||