北京大学学报(医学版) ›› 2025, Vol. 57 ›› Issue (3): 592-598. doi: 10.19723/j.issn.1671-167X.2025.03.025
单绒毛膜双羊膜囊双胎妊娠双胎之一胎死宫内对妊娠结局的影响
卞雯*, 周文君*, 吴天晨, 朱培静, 陈一诺, 原鹏波, 王学举, 王颖, 魏瑗*( ), 赵扬玉*(
), 赵扬玉*( )
)
- 北京大学第三医院妇产科,北京 100191
Perinatal outcomes of single intrauterine fetal demise in monochorionic diamniotic twins
Wen BIAN, Wenjun ZHOU, Tianchen WU, Peijing ZHU, Yinuo CHEN, Pengbo YUAN, Xueju WANG, Ying WANG, Yuan WEI*( ), Yangyu ZHAO*(
), Yangyu ZHAO*( )
)
- Department of Obstetrics and Gynecology, Peking University Third Hospital, Beijing 100191, China
摘要:
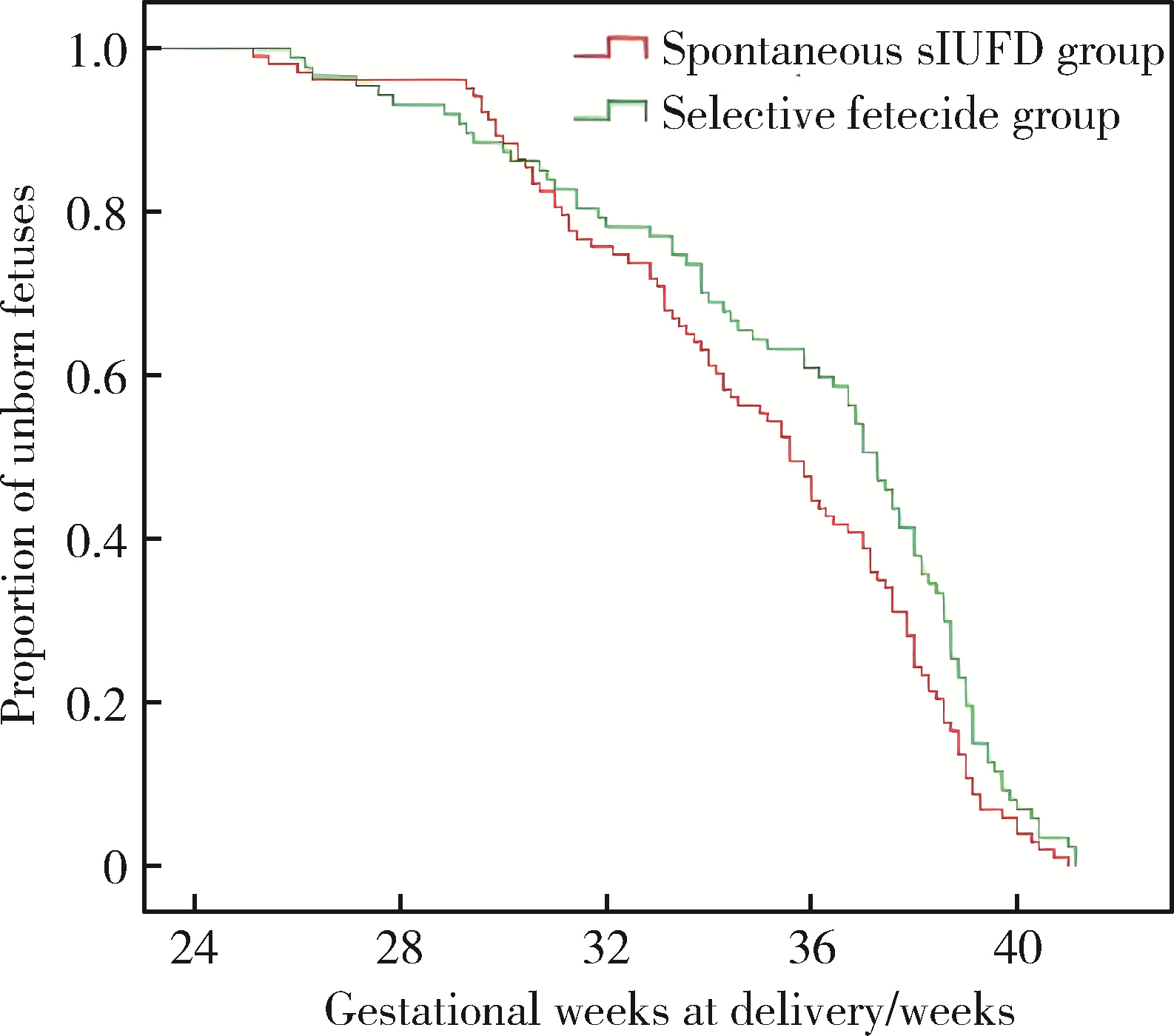
目的: 比较单绒毛膜双羊膜囊(monochorionic diamniotic,MCDA)双胎妊娠选择性减胎和自发双胎之一胎死宫内(single intrauterine fetal demise,sIUFD)后的存活儿妊娠结局,并探索预后的影响因素。方法: 收集2010年9月至2021年8月北京大学第三医院收治的219例MCDA双胎妊娠中一胎宫内死亡病例,根据胎死方式分为自发sIUFD组(120例)和选择性减胎组(99例),采集孕期母体情况、宫内死亡胎儿情况和妊娠结局资料进行回顾性病例分析。结果: 自发sIUFD组和选择性减胎组的存活儿活产率分别为85.0%及81.8%,存活儿总围生期存活率则分别为73.3%及81.8%,差异均无统计学意义。与自发sIUFD组相比,选择性减胎组的分娩孕周更大, < 37周早产率、新生儿窒息率和早期新生儿死亡率更低。以分娩孕周为结局变量,采用Cox回归分析发现,胎死方式并非影响存活儿分娩孕周的风险因素,而妊娠期高血压和胎死孕周为影响存活儿分娩孕周的独立风险因素;分别以是否出现 < 37周早产、存活儿宫内死亡和新生儿颅脑B超异常为结局变量,采用非条件Logistics回归分析发现,胎死方式、胎死孕周、死胎位置和胎儿并发症等为影响上述存活儿结局的独立风险因素;根据单因素分析结果,将上述风险因素纳入多因素回归分析,结果与单因素分析相同。结论: 对于存在严重双胎并发症的MCDA双胎妊娠患者,进行选择性减胎术后的存活儿预后更好,积极的宫内干预治疗对于改善存活儿预后具有重要的意义。
中图分类号:
- R714.2
| 1 |
doi: 10.1159/000342751 |
| 2 |
doi: 10.1097/AOG.0b013e31822f129d |
| 3 |
doi: 10.1186/s12884-021-03656-1 |
| 4 |
doi: 10.1159/000445291 |
| 5 |
doi: 10.1016/j.ajog.2008.08.039 |
| 6 |
中华医学会围产医学分会胎儿医学学组, 中华医学会妇产科学分会产科学组. 双胎妊娠临床处理指南(2020年更新)[J]. 中国产前诊断杂志(电子版), 2021, 13 (1): 51- 63.
|
| 7 |
doi: 10.1017/thg.2016.26 |
| 8 |
谢家磊, 吴天晨, 王晓莉, 等. 微波消融和射频消融减胎术治疗复杂性单绒毛膜妊娠的比较[J]. 中国生育健康杂志, 2022, 33 (1): 14- 17.
|
| 9 |
doi: 10.1002/pd.5423 |
| 10 |
doi: 10.1002/ijgo.13785 |
| 11 |
doi: 10.1016/j.ajog.2013.12.009 |
| 12 |
doi: 10.1016/j.ajog.2015.04.035 |
| 13 |
王颖, 魏瑗, 原鹏波, 等. 单绒毛膜双胎之一胎死宫内的共存儿预后分析[J]. 中华医学杂志, 2016, 96 (37): 3003- 3007.
|
| 14 |
doi: 10.1002/uog.22160 |
| 15 |
doi: 10.1002/pd.5830 |
| 16 |
doi: 10.1111/j.1471-0528.2006.01027.x |
| 17 |
doi: 10.1111/1471-0528.15530 |
| 18 |
doi: 10.1111/j.1471-0528.2009.02128.x |
| 19 |
doi: 10.1002/uog.14722 |
| 20 |
doi: 10.1002/uog.12408 |
| 21 |
doi: 10.1111/1471-0528.13490 |
| 22 |
|
| 23 |
doi: 10.1136/fn.88.4.F269 |
| 24 |
中国妇幼保健协会双胎妊娠专业委员会. 双胎输血综合征诊治及保健指南(2020)[J]. 中国实用妇科与产科杂志, 2020, 36 (8): 714- 721.
|
| 25 |
中国妇幼保健协会双胎妊娠专业委员会. 选择性胎儿宫内生长受限诊治及保健指南(2020)[J]. 中国实用妇科与产科杂志, 2020, 36 (7): 618- 625.
|
| 26 |
中国妇幼保健协会双胎妊娠专业委员会. 双胎反向动脉灌注序列征诊治及保健指南(2020)[J]. 中国实用妇科与产科杂志, 2020, 36 (6): 524- 530.
|
| 27 |
中华医学会围产医学分会胎儿医学学组, 中华医学会妇产科学分会产科学组. 双胎妊娠临床处理指南(第二部分): 双胎妊娠并发症的诊治[J]. 中国产前诊断杂志(电子版), 2015, 7 (4): 57- 64.
|
| 28 |
doi: 10.1002/uog.14879 |
| 29 |
doi: 10.1002/pd.5269 |
| 30 |
doi: 10.1017/thg.2018.57 |
| [1] | 王文琼, 侯玉珂, 李春, 张学武. 系统性红斑狼疮患者不良妊娠结局的预测因素[J]. 北京大学学报(医学版), 2025, 57(3): 599-603. |
| [2] | 杨树涵, 李奕昕, 崔浩亮, 王佑新, 吴玉莹, 王明月, 杨依凡, 恩卡尔·努尔, 杨磊, 王辉. 代谢相关脂肪性肝病及其心脏代谢风险指标异常与不良妊娠结局的相关性[J]. 北京大学学报(医学版), 2025, 57(3): 487-495. |
| [3] | 马会超,李军,王永清. 妊娠合并炎症性肠病的临床特点[J]. 北京大学学报(医学版), 2024, 56(2): 260-266. |
| [4] | 游芳凝,罗靓,刘香君,张学武,李春. 未分化结缔组织病患者的妊娠结局、疾病演变及其影响因素[J]. 北京大学学报(医学版), 2023, 55(6): 1045-1052. |
| [5] | 孙希雅,陈艺璐,曾琳,闫丽盈,乔杰,李蓉,智旭. 不孕女性维生素D水平与抗苗勒氏管激素的相关性及对妊娠结局的预测[J]. 北京大学学报(医学版), 2023, 55(1): 167-173. |
| [6] | 郑晓娟, 邓晓莉, 刘湘源. 54例抗磷脂综合征患者的妊娠结局[J]. 北京大学学报(医学版), 2014, 46(2): 323-328. |
| [7] | 任昀,杨硕,杨蕊,李蓉,陈新娜,王海燕,马彩虹,刘平,乔杰. 促性腺激素释放激素激动剂长方案与拮抗剂方案对体外受精治疗妊娠结局的影响[J]. 北京大学学报(医学版), 2013, 45(6): 877-881. |
| [8] | 陈倩, 郭燕燕. 妊娠合并慢性肾炎19例临床分析及随访[J]. 北京大学学报(医学版), 2002, 34(1): 93-94. |
|
||