北京大学学报(医学版) ›› 2020, Vol. 52 ›› Issue (6): 1135-1139. doi: 10.19723/j.issn.1671-167X.2020.06.025
类风湿关节炎合并色素沉着绒毛结节性滑膜炎1例及文献回顾
- 北京大学人民医院风湿免疫科,北京 100044
Rheumatoid arthritis combined with pigmented villonodular synovitis: A case report and literature review
- Department of Rheumatology and Immunology, Peking University People’s Hospital, Beijing 100044, China
摘要:
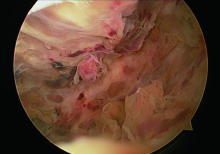
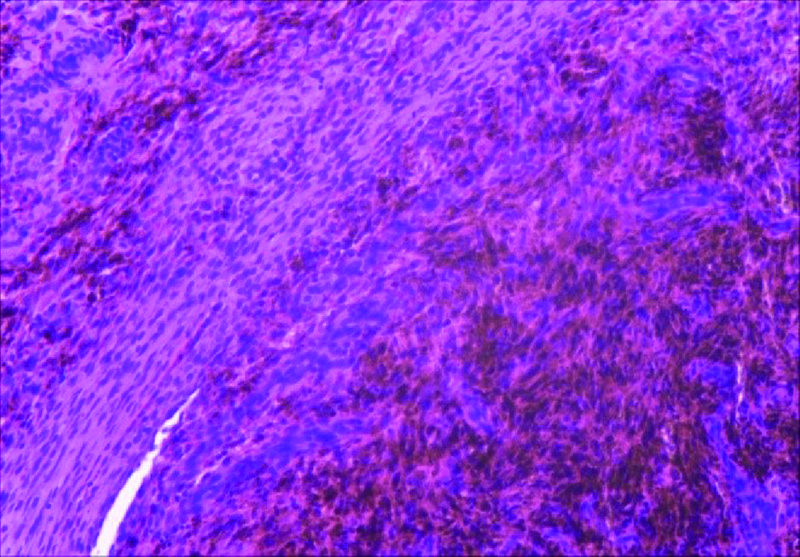
报道北京大学人民医院风湿免疫科诊治的1例类风湿关节炎(rheumatoid arthritis, RA)合并色素沉着绒毛结节性滑膜炎(pigmented villonodular synovitis, PVNS)的临床诊疗过程,并回顾国内外相关文献报道,对该病的诊断、治疗及预后进行综合分析,总结疾病特点,提高对该病的认识,减少漏诊并促进及早诊断。本例患者为45岁女性,RA病史15年,未进行规律治疗,近3个月右膝关节肿痛加重,关节腔穿刺发现大量RA病情难以解释的血性关节液。膝关节磁共振 (magnetic resonance imaging, MRI)提示T1及T2加权像均为低信号的含铁血黄素沉着。患者行膝关节镜检查,镜下表现及组织病理检查符合PVNS的诊断,给予患者切除增生滑膜。术后给予患者积极的功能锻炼及慢作用抗风湿药物规范治疗,随访半年恢复良好,右膝关节未再出现肿胀。RA是以慢性滑膜炎和关节破坏为特征的自身免疫疾病,PVNS是一种以滑膜增殖为特征的侵蚀性关节疾病,二者均为滑膜受累,且临床表现相似,RA合并PVNS的病例罕见,明确诊断具有难度。本研究分别在万方数据知识服务平台和中国知网以“类风湿关节炎”和“色素沉着绒毛结节性滑膜炎”为检索词检索相关文献,未检索到中文文献。在PubMed中以“rheumatoid arthritis”与“pigmented villonodular synovitis”为检索词检索,共检索到2篇英文文献。对于该病,临床医生需充分了解患者的病程发展,通过MRI及组织病理检查做出正确诊断,并进行有针对性地治疗。
中图分类号:
- R593.22
| [1] |
Croia C, Bursi R, Sutera D, et al. One year in review 2019: pathogenesis of rheumatoid arthritis[J]. Clin Exp Rheumatol, 2019,37(3):347-357.
pmid: 31111823 |
| [2] |
Ottaviani S, Ayral X, Dougados M, et al. Pigmented villonodular synovitis: a retrospective single-center study of 122 cases and review of the literature[J]. Semin Arthritis Rheum, 2011,40(6):539-546.
doi: 10.1016/j.semarthrit.2010.07.005 pmid: 20884045 |
| [3] |
Hirose I, Mori Y, Fujimoto A. Case report: rheumatoid arthritis occurring during observation after surgery for localized pigmented villonodular synovitis[J]. Mod Rheumatol, 2003,13(3):281-284.
pmid: 24387219 |
| [4] |
Zhao X, Ji W, Qian X, et al. Pigmented villonodular synovitis developing in a patient with rheumatoid arthritis[J]. J Clin Rheumatol, 2014,20(5):283-286.
doi: 10.1097/RHU.0000000000000119 pmid: 25036563 |
| [5] |
Dougados M. Synovial fluid cell analysis[J]. Baillieres Clin Rheumatol, 1996,10(3):519-534.
pmid: 8876957 |
| [6] | Myers BW, Masi AT. Pigmented villonodular synovitis and tenosynovitis: A clinical epidemiologic study of 166 cases and literature review[J]. Medicine (Baltimore), 1980,59(3):223-238. |
| [7] |
Mastboom M, Verspoor F, Verschoor A, et al. Higher incidence rates than previously known in tenosynovial giant cell tumors[J]. Acta orthopaedica, 2017,88(6):688-694.
doi: 10.1080/17453674.2017.1361126 pmid: 28787222 |
| [8] |
Fiocco U, Sfriso P, Lunardi F, et al. Molecular pathways involved in synovial cell inflammation and tumoral proliferation in diffuse pigmented villonodular synovitis[J]. Autoimmun Rev, 2010,9(11):780-784.
doi: 10.1016/j.autrev.2010.07.001 pmid: 20620241 |
| [9] |
Gouin F, Noailles T. Localized and diffuse forms of tenosynovial giant cell tumor (formerly giant cell tumor of the tendon sheath and pigmented villonodular synovitis)[J]. Orthop Traumatol Surg Res, 2017,103(1S):S91-S97.
doi: 10.1016/j.otsr.2016.11.002 pmid: 28057477 |
| [10] |
Staals E, Ferrari S, Donati D, et al. Diffuse-type tenosynovial giant cell tumour: Current treatment concepts and future perspectives[J]. Eur J Cancer, 2016,63:34-40.
doi: 10.1016/j.ejca.2016.04.022 pmid: 27267143 |
| [11] |
Cupp J, Miller M, Montgomery K, et al. Translocation and expression of CSF1 in pigmented villonodular synovitis, tenosynovial giant cell tumor, rheumatoid arthritis and other reactive synovitides[J]. Am J Surg Pathol, 2007,31(6):970-976.
doi: 10.1097/PAS.0b013e31802b86f8 pmid: 17527089 |
| [12] |
Oliviero F, Galozzi P, Ramonda R, et al. Unusual findings in synovial fluid analysis: A review[J]. Ann Clin Lab Sci, 2017,47(3):253-259.
pmid: 28667024 |
| [13] | 列锐锋. 膝关节色素沉着绒毛结节性滑膜炎MRI表现[J]. 罕少疾病杂志, 2020,27(2):67-69. |
| [14] |
Houdek MT, Scorianz M, Wyles CC, et al. Long-term outcome of knee arthroplasty in the setting of pigmented villonodular synovitis[J]. Knee, 2017,24(4):851-855.
doi: 10.1016/j.knee.2017.04.019 pmid: 28552192 |
| [15] |
Barile A, Sabatini M, Iannessi F, et al. Pigmented villonodular synovitis (PVNS) of the knee joint: magnetic resonance imaging (MRI) using standard and dynamic paramagnetic contrast media. Report of 52 cases surgically and histologically controlled[J]. Radiol Med, 2004,107(4):356-366.
pmid: 15103287 |
| [16] | 巫娟, 徐钢, 傅静. 膝关节色素沉着绒毛结节性滑膜炎的临床病理分析[J]. 四川医学, 2017,38(9):1010-1013. |
| [17] |
Bernthal N, Ishmael C, Burke Z. Management of pigmented villonodular synovitis (PVNS): an orthopedic surgeon’s perspective[J]. Curr Oncol Rep, 2020,22(6):63.
pmid: 32494892 |
| [18] |
Palmerini E, Staals E, Maki R, et al. Tenosynovial giant cell tumour/pigmented villonodular synovitis: outcome of 294 patients before the era of kinase inhibitors[J]. Eur J Cancer, 2015,51(2):210-217.
doi: 10.1016/j.ejca.2014.11.001 pmid: 25465190 |
| [19] |
Tap W, Gelderblom H, Palmerini E, et al. Pexidartinib versus placebo for advanced tenosynovial giant cell tumour (ENLIVEN): a randomised phase 3 trial[J]. Lancet, 2019,394(10197):478-487.
doi: 10.1016/S0140-6736(19)30764-0 pmid: 31229240 |
| [20] |
Monestime S, Lazaridis D. Pexidartinib (TURALIO?): The first FDA-indicated systemic treatment for tenosynovial giant cell tumor[J]. Drugs R D, 2020,20(3):189-195.
doi: 10.1007/s40268-020-00314-3 pmid: 32617868 |
| [21] |
Gelderblom H, Cropet C, Chevreau C, et al. Nilotinib in locally advanced pigmented villonodular synovitis: a multicentre, open-label, single-arm, phase 2 trial[J]. Lancet Oncol, 2018,19(5):639-648.
doi: 10.1016/S1470-2045(18)30143-8 pmid: 29571946 |
| [1] | 刘东武, 陈杰, 高明利, 于静. 类风湿关节炎伴发淋巴结Castleman样病理改变1例[J]. 北京大学学报(医学版), 2024, 56(5): 928-931. |
| [2] | 黄会娜,赵静,赵祥格,白自然,李霞,王冠. 乳酸对类风湿关节炎患者外周血CD4+T细胞亚群的调控作用[J]. 北京大学学报(医学版), 2024, 56(3): 519-525. |
| [3] | 汤晓菲,李永红,丁秋玲,孙卓,张阳,王育梅,田美伊,刘坚. 类风湿关节炎患者下肢深静脉血栓发病率及危险因素[J]. 北京大学学报(医学版), 2024, 56(2): 279-283. |
| [4] | 邹雪,白小娟,张丽卿. 艾拉莫德联合托法替布治疗难治性中重度类风湿关节炎的疗效[J]. 北京大学学报(医学版), 2023, 55(6): 1013-1021. |
| [5] | 吴琦,蔡月明,何娟,黄文蒂,王庆文. 血脂异常与类风湿关节炎肺间质病变的相关性分析[J]. 北京大学学报(医学版), 2023, 55(6): 982-992. |
| [6] | 张警丰,金银姬,魏慧,姚中强,赵金霞. 体重指数与类风湿关节炎临床特征的相关性分析[J]. 北京大学学报(医学版), 2023, 55(6): 993-999. |
| [7] | 金银姬,孙琳,赵金霞,刘湘源. 血清IgA型抗鼠科肉瘤病毒癌基因同源物B1抗体在类风湿关节炎中的意义[J]. 北京大学学报(医学版), 2023, 55(4): 631-635. |
| [8] | 蔡文心,李仕成,刘一鸣,梁如玉,李静,郭建萍,胡凡磊,孙晓麟,李春,刘栩,叶华,邓立宗,李茹,栗占国. 类风湿关节炎临床分层及其特征的横断面研究[J]. 北京大学学报(医学版), 2022, 54(6): 1068-1073. |
| [9] | 程昉,杨邵英,房星星,王璇,赵福涛. CCL28-CCR10通路在类风湿关节炎单核细胞迁移中的作用[J]. 北京大学学报(医学版), 2022, 54(6): 1074-1078. |
| [10] | 刘蕊,赵金霞,闫良. 类风湿关节炎合并下肢静脉血栓患者的临床特点[J]. 北京大学学报(医学版), 2022, 54(6): 1079-1085. |
| [11] | 张警丰,金银姬,魏慧,姚中强,赵金霞. 类风湿关节炎患者生活质量与疾病活动度的横断面研究[J]. 北京大学学报(医学版), 2022, 54(6): 1086-1093. |
| [12] | 高超,陈立红,王莉,姚鸿,黄晓玮,贾语博,刘田. 类风湿关节炎合并纤维肌痛简易分类标准的临床验证[J]. 北京大学学报(医学版), 2022, 54(2): 278-282. |
| [13] | 娄雪,廖莉,李兴珺,王楠,刘爽,崔若玫,徐健. 类风湿关节炎患者外周血TWEAK基因启动子区甲基化状态及其表达[J]. 北京大学学报(医学版), 2021, 53(6): 1020-1025. |
| [14] | 钟华,徐丽玲,白明欣,苏茵. 类风湿关节炎患者趋化因子CXCL9和CXCL10在骨侵蚀中的作用[J]. 北京大学学报(医学版), 2021, 53(6): 1026-1031. |
| [15] | 罗靓,霍文岗,张钦,李春. 类风湿关节炎合并角膜溃疡的临床特点和相关因素分析[J]. 北京大学学报(医学版), 2021, 53(6): 1032-1036. |
|
||