北京大学学报(医学版) ›› 2019, Vol. 51 ›› Issue (3): 493-500. doi: 10.19723/j.issn.1671-167X.2019.03.017
股骨近端防旋髓内钉与动力髋螺钉治疗不稳定型粗隆间骨折的meta分析
- 北京大学人民医院创伤骨科, 北京 100044
Proximal femoral nails antirotation and dynamic hip screws for fixation of unstable intertrochanteric fractures of femur: A meta-analysis
Yi-ran ZHANG,Feng RAO,Wei PI,Pei-xun ZHANG△( ),Bao-guo JIANG△(
),Bao-guo JIANG△( )
)
- Department of Trauma and Orthopedics, Peking University People’s Hospital, Beijing 100044, China
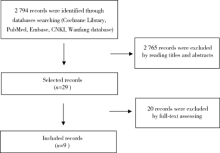
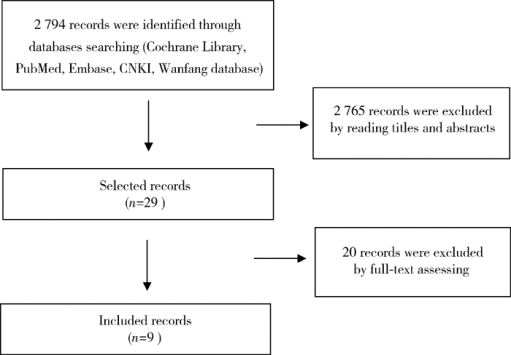
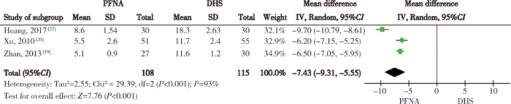
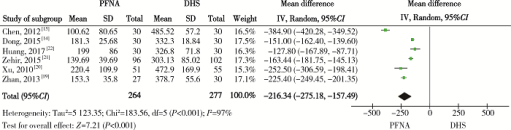
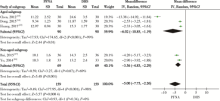
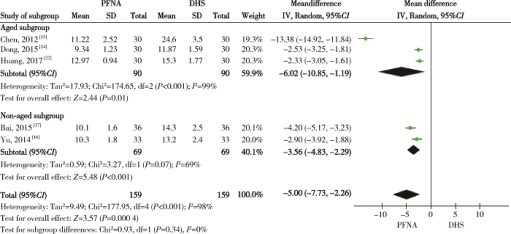
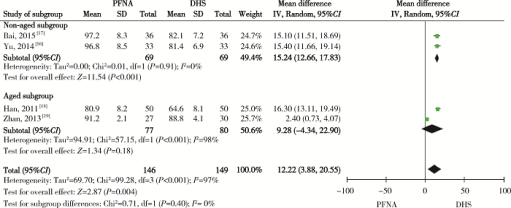
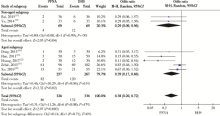
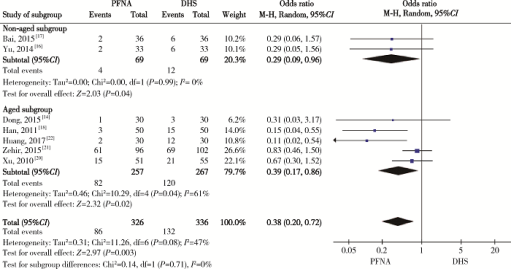
摘要: 目的 不稳定型粗隆间骨折手术治疗采用髓内固定还是髓外固定仍存在争议,本研究运用meta分析方法评价股骨近端防旋髓内钉(proximal femoral nail antirotation,PFNA)和动力髋螺钉(dynamic hip screw,DHS)用于不稳定型粗隆间骨折的疗效及安全性。方法 计算机检索PubMed、Embase、The Cochrane Central Register of Controlled Trials(CENTRAL)、Google Scholar、中国科技论文与引文数据库(CSTPCD)、中国期刊全文数据库(CNKI)等数据库,截止日期为2019年1月1日,由2位研究者独立按照纳入与排除标准筛选PFNA与DHS治疗不稳定型粗隆间骨折的随机对照研究,进行质量评价,以切口长度、手术时间、术中出血量、开始负重时间、骨折愈合时间、Harris功能评分等临床疗效指标和并发症等安全性指标为观察指标,提取相关数据,应用RevMan 5.3统计软件进行数据分析。结果 纳入随机对照试验9篇,共779例患者,其中PFNA固定383例、DHS固定396例。分析结果提示,与DHS固定相比,PFNA固定的手术切口长度小[均数差(mean difference,MD)=-7.43, 95%CI(-9.31,5.55),P<0.05]、手术时间短[MD=-20.76, 95%CI(-29.57,-11.95),P<0.05]、术中出血量少[MD=-216.34, 95%CI(-275.18,-157.49),P<0.05]、术后可更早开始负重[MD=-12.34, 95%CI (-17.71,-6.97),P<0.05]、骨折愈合时间短[MD=-5.00, 95%CI(-7.73,-2.26),P<0.05]、术后Harris功能评分高[MD=12.22, 95%CI(3.88,20.55),P<0.05]、Harris评分优良率高[OR=3.56, 95%CI(1.44,8.81),P<0.05]、并发症发生率低[OR=0.48, 95%CI(0.33,0.70),P<0.05]。按年龄亚组分析,组间差异均无统计学意义。二者在住院时间及发生内固定松动、术中和术后股骨干骨折以及内固定断裂、切出、移位、退钉等固定失效并发症方面的差异均无统计学意义(P>0.05)。结论 现有证据表明针对不稳定型粗隆间骨折,PFNA内固定临床疗效优于DHS内固定,但二者的安全性分析仍需更多高质量随机对照研究提供更可靠的证据。
中图分类号:
- R683.3
| [1] |
Gullberg B, Johnell O, Kanis JA . World-wide projections for hip fracture[J]. Osteoporos Int, 1997,7(5):407-413.
doi: 10.1007/PL00004148 |
| [2] |
Kanis JA, Johnell O, De Laet C , et al. International variations in hip fracture probabilities: implications for risk assessment[J]. J Bone Miner Res, 2002,17(7):1237-1244.
doi: 10.1359/jbmr.2002.17.7.1237 |
| [3] |
Mattisson L, Bojan A, Enocson A . Epidemiology, treatment and mortality of trochanteric and subtrochanteric hip fractures: data from the Swedish fracture register[J]. BMC Musculoskelet Disord, 2018,19(1):369.
doi: 10.1186/s12891-018-2276-3 |
| [4] |
Lizaur-Utrilla A, Gonzalez-Navarro B, Vizcaya-Moreno MF , et al. Reasons for delaying surgery following hip fractures and its impact on one year mortality[J]. Int Orthop, 2019,43(2):441-448.
doi: 10.1007/s00264-018-3936-5 |
| [5] | Brunner LC, Eshilian-Oates L, Kuo TY . Hip fractures in adults[J]. Am Fam Physician, 2003,67(3):537-542. |
| [6] |
Hagino H, Endo N, Harada A , et al. Survey of hip fractures in Japan: recent trends in prevalence and treatment[J]. J Orthop Sci, 2017,22(5):909-914.
doi: 10.1016/j.jos.2017.06.003 |
| [7] |
Saudan M, Lübbeke A, Sadowski C , et al. Pertrochanteric fractures: is there an advantage to an intramedullary nail? A rando-mized, prospective study of 206 patients comparing the dynamic hip screw and proximal femoral nail[J]. J Orthop Trauma, 2002,16(6):386-393.
doi: 10.1097/00005131-200207000-00004 |
| [8] |
Knobe M, Gradl G, Ladenburger A , et al. Unstable intertrochanteric femur fractures: Is there a consensus on definition and treatment in Germany?[J]. Clin Orthop Relar Res, 2013,471(9):2831-2840.
doi: 10.1007/s11999-013-2834-9 |
| [9] |
Lenich A, Vester H, Nerlich M , et al. Clinical comparison of the second and third generation of intramedullary devices for trochanteric fractures of the hip: Blade vs. screw[J]. Injury, 2010,41(12):1292-1296.
doi: 10.1016/j.injury.2010.07.499 |
| [10] |
Giraud B, Dehoux E, Jovenin N , et al. Pertrochanteric fractures: a randomized prospective study comparing dynamic screw plate and intramedullary fixation[J]. Rev Chir Orthop Reparatrice Appar Mot, 2005,91(8):732-736.
doi: 10.1016/S0035-1040(05)84484-8 |
| [11] |
Yamauchi K, Fushimi K, Shirai G , et al. Comparison of func-tional recovery in the very early period after surgery between plate and nail fixation for correction of stable femoral intertrochanteric fractures: a controlled clinical trial of 18 patients[J]. Geriatr Orthop Surg Rehabil, 2014,5(2):63-68.
doi: 10.1177/2151458514527607 |
| [12] |
Guerra MT, Pasqualin S, Souza MP , et al. Functional recovery of elderly patients with surgically-treated intertrochanteric fractures: preliminary results of a randomised trial comparing the dynamic hip screw and proximal femoral nail techniques[J]. Injury, 2014,45(Suppl. 5):S26-S31.
doi: 10.1016/S0020-1383(14)70017-8 |
| [13] |
Liberati A, Altman DG, Tetzlaff J , et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration[J]. J Clin Epidemiol, 2009,62(10):e1-e34.
doi: 10.1016/j.jclinepi.2009.06.006 |
| [14] | 董宝铁, 高伟, 周振东 . 动力髋螺钉与防旋型股骨近端髓内钉治疗高龄不稳定型股骨粗隆间骨折比较[J]. 现代仪器与医疗, 2015,21(2):86-87, 92. |
| [15] | 陈振宇, 黄福才, 钟巍巍 . PFNA治疗高龄股骨粗隆间不稳定型骨折应用研究[J]. 中国社区医师(医学专业), 2012,14(21):198-199. |
| [16] | 于长明 . 股骨粗隆间不稳定骨折应用PFNA和DHS内固定的比较[J]. 中国实用医药, 2014,9(22):61-62. |
| [17] | 白愉乐 . PFNA和DHS内固定治疗股骨粗隆间不稳定骨折的比较研究[J]. 中国现代药物应用, 2015,9(20):63-64. |
| [18] | 韩成龙 . 老年股骨粗隆间不稳定骨折不同内固定方法的疗效比较[J]. 河北医药, 2011,33(22):3390-3392. |
| [19] | 展振江, 李明, 张元凯 , 等. PFNA与DHS治疗老年股骨粗隆间不稳定性骨折疗效对比[J]. 山东大学学报(医学版), 2013,51(12):92-94, 99. |
| [20] |
Xu YZ, Geng DC, Mao HQ , et al. A comparison of the proximal femoral nail antirotation device and dynamic hip screw in the treatment of unstable pertrochanteric fracture[J]. J Int Med Res, 2010,38(4):1266-1275.
doi: 10.1177/147323001003800408 |
| [21] |
Zehir S, Zehir R, Zehir S , et al. Proximal femoral nail antirotation against dynamic hip screw for unstable trochanteric fractures; a prospective randomized comparison[J]. Eur J Trauma Emerg Surg, 2015,41(4):393-400.
doi: 10.1007/s00068-014-0463-y |
| [22] |
Huang SG, Chen B, Zhang Y , et al. Comparison of the clinical effectiveness of PFNA, PFLCP, and DHS in treatment of unstable intertrochanteric femoral fracture[J]. Am J Ther, 2017,24(6):e659-e666.
doi: 10.1097/MJT.0000000000000346 |
| [23] | Yin S, Dai X, Zhang DF , et al. Is proximal femoral nail antirotation superior to gamma nail and dynamic hip screw in treatment of intertrochanteric fractures? A pairwise and network meta-analysis[J]. Int J Clin Exp Med, 2016,9(12):22993-23007. |
| [24] |
Ma KL, Wang X, Luan FJ , et al. Proximal femoral nails antirotation, Gamma nails, and dynamic hip screws for fixation of intertrochanteric fractures of femur: A meta-analysis[J]. Orthop Traumatol Surg Res, 2014,100(8):859-866.
doi: 10.1016/j.otsr.2014.07.023 |
| [25] |
Swart E, Makhni EC, Macaulay W , et al. Cost-effectiveness ana-lysis of fixation options for intertrochanteric hip fractures[J]. J Bone Joint Surg Am, 2014,96(19):1612-1620.
doi: 10.2106/JBJS.M.00603 |
| [26] | 程建, 雷会宁, 冯仕明 , 等. PFNA与DHS治疗不稳定型股骨粗隆间骨折的Meta分析[J]. 重庆医学, 2016,45(21):2956-2961. |
| [27] |
Audigé L, Hanson B, Swiontkowski MF . Implant-related complications in the treatment of unstable intertrochanteric fractures: meta-analysis of dynamic screw-plate versus dynamic screw-intramedullary nail devices[J]. Int Orthop, 2003,27(4):197-203.
doi: 10.1007/s00264-003-0457-6 |
| [28] | Parker MJ, Handoll HH. Gamma and other cephalocondylic intra-medullary nails versus extramedullary implants for extracapsular hip fractures in adults [J]. Cochrane Database Syst Rev, 2010( 9): CD000093. |
| [29] |
Weiser L, Ruppel AA, Nüchtern JV , et al. Extra- vs. intra-medullary treatment of pertrochanteric fractures: a biomechanical in vitro study comparing dynamic hip screw and intramedullary nail[J]. Arch Orthop Trauma Surg, 2015,135(8):1101-1106.
doi: 10.1007/s00402-015-2252-4 |
| [1] | 陈斌,吴超,刘彬,于涛,王振宇. 脊髓髓内海绵状血管瘤患者不同治疗方式的预后[J]. 北京大学学报(医学版), 2023, 55(4): 652-657. |
| [2] | 袁昌巍,王盈进,张书杰,沈胜利,段鸿洲. 显微外科手术与血管内栓塞治疗硬脊膜动静脉瘘临床疗效比较的meta分析[J]. 北京大学学报(医学版), 2022, 54(2): 304-314. |
| [3] | 冯菁楠,高乐,孙一鑫,杨继春,邓思危,孙凤,詹思延. Xpert®MTB/RIF对我国人群活动性肺结核和利福平耐药肺结核诊断准确性的meta分析[J]. 北京大学学报(医学版), 2021, 53(2): 320-326. |
| [4] | 侯国进,周方,田耘,姬洪全,张志山,郭琰,吕扬,杨钟玮,张雅文. 后路短节段跨伤椎椎弓根螺钉固定治疗胸腰段爆裂骨折术后再发后凸的危险因素[J]. 北京大学学报(医学版), 2021, 53(1): 167-174. |
| [5] | 刘中砥,许庭珉,党育,张殿英,付中国. 有限切开复位髓内外联合固定技术治疗股骨转子下骨折的临床随访[J]. 北京大学学报(医学版), 2020, 52(6): 1102-1106. |
| [6] | 曾保起,于树青,陈瑶,翟伟,刘斌,詹思延,孙凤. 主动脉瓣生物瓣膜安全性的系统评价与meta分析[J]. 北京大学学报(医学版), 2020, 52(3): 547-556. |
| [7] | 孙建军,杨军,谢京城,常青,马长城,郑梅,LIAO Hung-I,王涛,陈晓东,韩芸峰,林国中,于涛,张嘉,司雨. 少节段和多节段髓内肿瘤的临床对照[J]. 北京大学学报(医学版), 2019, 51(5): 840-850. |
| [8] | 张玮,张培训. 老年髋部骨折患者围手术期血栓预防时限分析[J]. 北京大学学报(医学版), 2019, 51(3): 501-504. |
| [9] | 陈健,左才红,张财义,杨明,张培训. 解剖型髓内钉和股骨近端防旋髓内钉治疗老年股骨转子间骨折的疗效比较[J]. 北京大学学报(医学版), 2019, 51(2): 283-287. |
| [10] | 刘爽,郭雨龙,杨静逸,王维,徐健. 间充质干细胞治疗系统性红斑狼疮有效性的meta分析[J]. 北京大学学报(医学版), 2018, 50(6): 1014-1021. |
| [11] | 魏滨,张华,徐懋,李民,王军,张利萍,郭向阳,赵一鸣,周方. 不同麻醉方法对髋部骨折老年患者术后转归的影响[J]. 北京大学学报(医学版), 2017, 49(6): 1008-1013. |
| [12] | 石慧峰, 张敬旭, 张嵘, 王晓莉. 中国0~6岁儿童孤独症谱系障碍患病率的meta分析[J]. 北京大学学报(医学版), 2017, 49(5): 798-806. |
| [13] | 张伯松, 李文毅, 刘兴华, 危杰, 贺良, 王满宜. 肱骨干骨折手术与非手术治疗的比较[J]. 北京大学学报(医学版), 2017, 49(5): 851-854. |
| [14] | 马燕燕,章晶晶,高雪梅. 不同下颌前伸度口腔矫治器治疗阻塞性睡眠呼吸暂停低通气综合征的系统评价[J]. 北京大学学报(医学版), 2017, 49(4): 691-699. |
| [15] | 张树,张继源,杨杜明,杨明,张培训. 矢状位不稳定转子间骨折的形态特征和复位技术[J]. 北京大学学报(医学版), 2017, 49(2): 236-241. |
|
||