北京大学学报(医学版) ›› 2019, Vol. 51 ›› Issue (4): 737-741. doi: 10.19723/j.issn.1671-167X.2019.04.025
合并急性肾损伤的感染性心内膜炎的临床特点和预后分析
- 北京大学第一医院心脏外科, 北京 100034
Clinical features and prognosis of infective endocarditis patients with acute kidney injury
Si-yu ZHANG( ),Xi-hui LI,Feng XIAO
),Xi-hui LI,Feng XIAO
- Department of Cardiac Surgery, Peking University First Hospital, Beijing 100034, China
摘要:
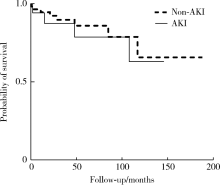
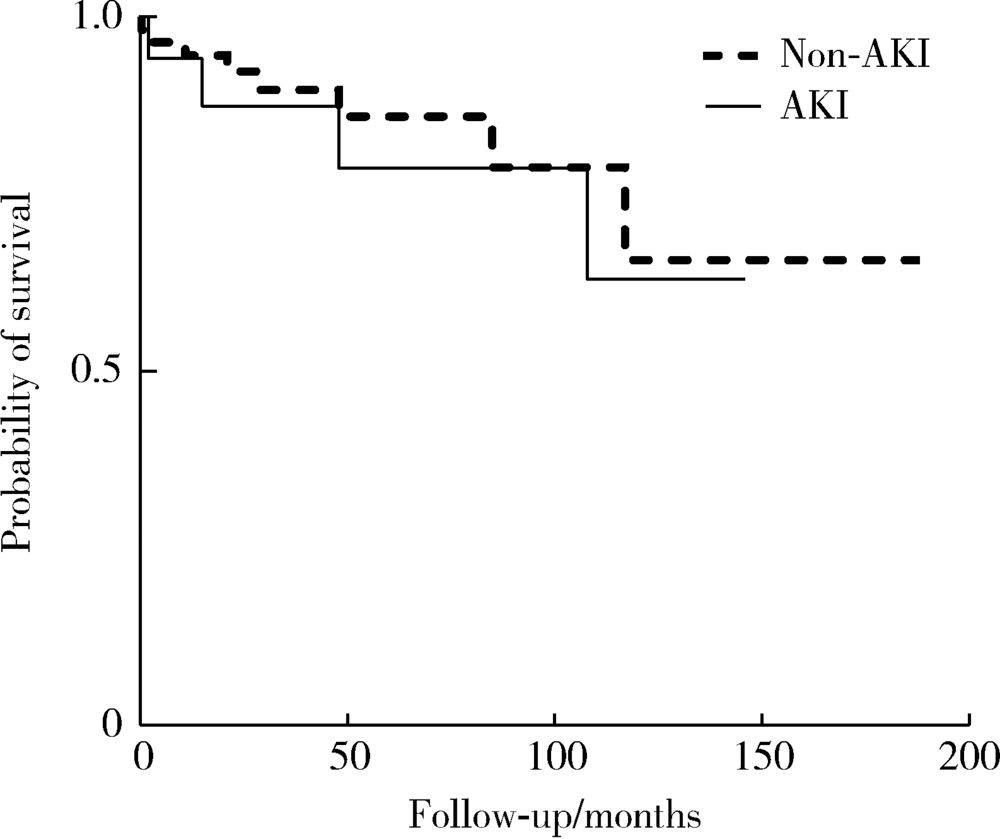
目的:探讨合并急性肾损伤(acute kidney injury,AKI)的感染性心内膜炎(infective endocarditis,IE)患者的临床特点,分析此类患者的围术期及预后情况。方法:回顾性分析2002年1月至2018年6月在北京大学第一医院心脏外科就诊的IE患者100例。根据患者术前情况及AKIN标准,分为AKI组和非AKI组,比较两组临床资料和术后并发症的差异,随访对比两组预后情况。结果:AKI组21例和非AKI组79例,总体平均年龄(43.7±15.7)岁,男女比例3 :1,IE患者中AKI的发生率为21%。两组间年龄、性别构成差异无统计学意义。与非AKI组相比,AKI组患者皮疹及下肢水肿的比例更高(P=0.017和P=0.001),尿潜血及尿蛋白阳性率更高(P<0.001),血红蛋白及血清白蛋白水平更低(P<0.001),临床心功能更差(P=0.033)。两组病原菌检出率及病原菌种类差异无统计学意义。除9例患者拒绝手术外,其余91例患者均接受了体外循环下心内直视手术,包括AKI组19例和非AKI组72例。AKI组患者围术期红细胞用量更多(P=0.010),术后呼吸机使用时间及监护室停留时间更长(P=0.028和P=0.003)。以两组患者术前末次肌酐为基准,AKI组新发术后肾功能不全比例更高(P=0.004)。两组患者院内死亡率差异无统计学意义(P=0.463),随访期间两组生存率差异未见统计学意义(P=0.581)。结论:与非AKI组相比,合并AKI的IE患者围术期并发症发生率更高,但两组患者院内死亡率及预后无明显差异。
中图分类号:
- R542.42
| [1] | Habib G, Lancellotti P, Antunes MJ , et al. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM)[J]. Eur Heart J, 2015,36(44):3075-3128. |
| [2] | Thakar CV, Worley S , Arrigain, S, et al. Influence of renal dysfunction on mortality after cardiac surgery: Modifying effect of preoperative renal function[J]. Kidney Int, 2005,67(3):1112-1119. |
| [3] | Shanmugam B, Khalif A, Pati P , et al. Trends in acute kidney injury in patients diagnosed with infective endocarditis: Data from the national inpatient sample from 1999-2014[J]. Chest, 2017,152(4):A69. |
| [4] | Legrand M, Pirracchio R, Rosa A , et al. Incidence, risk factors and prediction of post-operative acute kidney injury following cardiac surgery for active infective endocarditis: An observational study[J]. Crit Care, 2013,17(5):R220. |
| [5] | Mylonakis E, Calderwood SB . Infective endocarditis in adults. N Engl J Med, 2001,345(18):1318-1330. |
| [6] | Cruz DN, Bagshaw SM, Ronco C , et al. Acute kidney injury: classification and staging[J]. Contrib Nephrol, 2010,164:24-32. |
| [7] | Slipczuk L, Codolosa JN, Davila CD , et al. Infective endocarditis epidemiology over five decades: a systematic review[J]. PLoS One, 2013,8(12):e82665. |
| [8] | Olmos C, Vilacosta I, Fernández-Pérez C , et al. The evolving nature of infective endocarditis in Spain: A population-based study (2003 to 2014)[J]. J Am Coll Cardiol, 2017,70(22):2795-2804. |
| [9] | Shih CJ, Chu H, Chao PW , et al. Long-term clinical outcome of major adverse cardiac events in survivors of infective endocarditis a nationwide population-based study[J]. Circulation, 2014,130(19):1684-1691. |
| [10] | Boils CL, Nasr SH, Walker PD , et al. Update on endocarditis-associated glomerulonephritis[J]. Kidney Int, 2015,87(6):1241-1249. |
| [11] | 张苑, 任鹏涛, 杨婧 , 等. 感染性心内膜炎患者临床特征与预后影响因素分析[J]. 中华医院感染学杂志, 2016,26(7):1531-1532. |
| [12] | Ambrosioni J, Hernandez-Meneses M, Téllez A , et al. Hospital clinic infective endocarditis investigators. The changing epide-miology of infective endocarditis in the Twenty-First Century[J]. Curr Infect Dis Rep, 2017,19(5):21. |
| [13] | Fowler VG Jr, Miro JM, Hoen B , et al. Staphylococcus aureus endocarditis: a consequence of medical progress[J]. JAMA, 2005,293(24):3012-3021. |
| [14] | Salgado-Pabón W, Breshears L, Spaulding AR , et al. Superantigens are critical for Staphylococcus aureus infective endocarditis, sepsis, and acute kidney injury [J/OL]. MBio, 2013,4(4), doi: 10.1128/mBio.00494-13. |
| [15] | Wallace SM, Walton BI, Kharbanda RK , et al. Mortality from infective endocarditis: clinical predictors of outcome[J]. Heart, 2002,88(1):53-60. |
| [16] | Kang DH, Kim YJ, Kim SH , et al. Early surgery versus conventional treatment for infective endocarditis[J]. N Engl J Med, 2012,366(26):2466-2473. |
| [17] | Chu VH, Park LP, Athan E , et al. Association between surgical indications, operative risk, and clinical outcome in infective endocarditis: a prospective study from the international collaboration on endocarditis[J]. Circulation, 2015,131(2):131-140. |
| [18] | Mariscalco G, Lorusso R, Dominici C , et al. Acute kidney injury: a relevant complication after cardiac surgery[J]. Ann Thorac Surg, 2011,92(4):1539-1547. |
| [19] | Pang PY, Sin YK, Lim CH , et al. Surgical management of infective endocarditis: An analysis of early and late outcomes[J]. Eur J Cardiothorac Surg, 2015,47(5):826-832. |
| [20] | Buchholtz K, Larsen CT, Hassager C , et al. In infectious endocarditis patients mortality is highly related to kidney function at time of diagnosis: A prospective observational cohort study of 231 cases[J]. Eur J Intern Med, 2009,20(4):407-410. |
| [1] | 于博,赵扬玉,张喆,王永清. 妊娠合并感染性心内膜炎1例[J]. 北京大学学报(医学版), 2022, 54(3): 578-580. |
| [2] | 杨阳,肖锋,王进,宋波,李西慧,张师杰,何志嵩,张寰,尹玲. 同期手术治疗心脏病和非心脏疾病[J]. 北京大学学报(医学版), 2021, 53(2): 327-331. |
| [3] | 孟昭婷,穆东亮. 肺叶切除术中少尿与术后急性肾损伤的关系[J]. 北京大学学报(医学版), 2021, 53(1): 188-194. |
| [4] | 蔺轲,谢俊卿,胡永华,孔桂兰. 支持向量机在ICU急性肾损伤患者住院死亡风险预测中的应用[J]. 北京大学学报(医学版), 2018, 50(2): 239-244. |
| [5] | 袁远,沈明,高旭光. 以蛛网膜下腔出血为首发而血培养阴性的感染性心内膜炎1例报道并文献回顾[J]. 北京大学学报(医学版), 2017, 49(6): 1081-1086. |
| [6] | 肖冰冰, 张岱, 陈锐, 史惠蓉, 辛晓燕,王惠兰,庞义存,朱赛楠,姚晨, 廖秦平 . 蔗糖凝胶治疗细菌性阴道病的多中心、随机、双盲、平行对照Ⅲ期临床试验[J]. 北京大学学报(医学版), 2015, 47(6): 925-932. |
| [7] | 于婕,万峰,解基严,吴松,崔仲奇,徐敏,张喆,高炜. EuroSCORE与SinoSCORE对冠状动脉旁路移植术后患者早期生命质量的预测价值[J]. 北京大学学报(医学版), 2015, 47(5): 769-773. |
| [8] | 李西慧,李岩,肖锋,李一帆,王进,宋波,杨阳,董士勇. 终末期肾病透析依赖患者行心脏手术的围手术期管理和随访结果[J]. 北京大学学报(医学版), 2013, 45(4): 634-. |
| [9] | 肖冰冰, 吴成, 林怀宪, 张岱, 耿力, 王惠兰, 于风华, 朱赛楠, 姚晨, 廖秦平 . 蔗糖凝胶治疗细菌性阴道病Ⅱ期临床试验研究[J]. 北京大学学报(医学版), 2010, 42(6): 746-751. |
| [10] | 毛斌, 陈英, 颜晓蕾, 张健群. 多器官衰竭评分系统及其修正法在心脏手术后的使用价值[J]. 北京大学学报(医学版), 2010, 42(2): 151-154. |
|
||