北京大学学报(医学版) ›› 2020, Vol. 52 ›› Issue (1): 158-162. doi: 10.19723/j.issn.1671-167X.2020.01.025
恶性孤立性肺结节患者预后因素分析
- 北京大学第一医院老年内科,北京 100034
Prognosis factors analysis of patients with malignant solitary pulmonary nodules
Yu-qing OUYANG,Lian-fang NI,Xin-min LIU( )
)
- Department of Geriatrics, Peking University First Hospital, Beijing 100034, China
摘要:
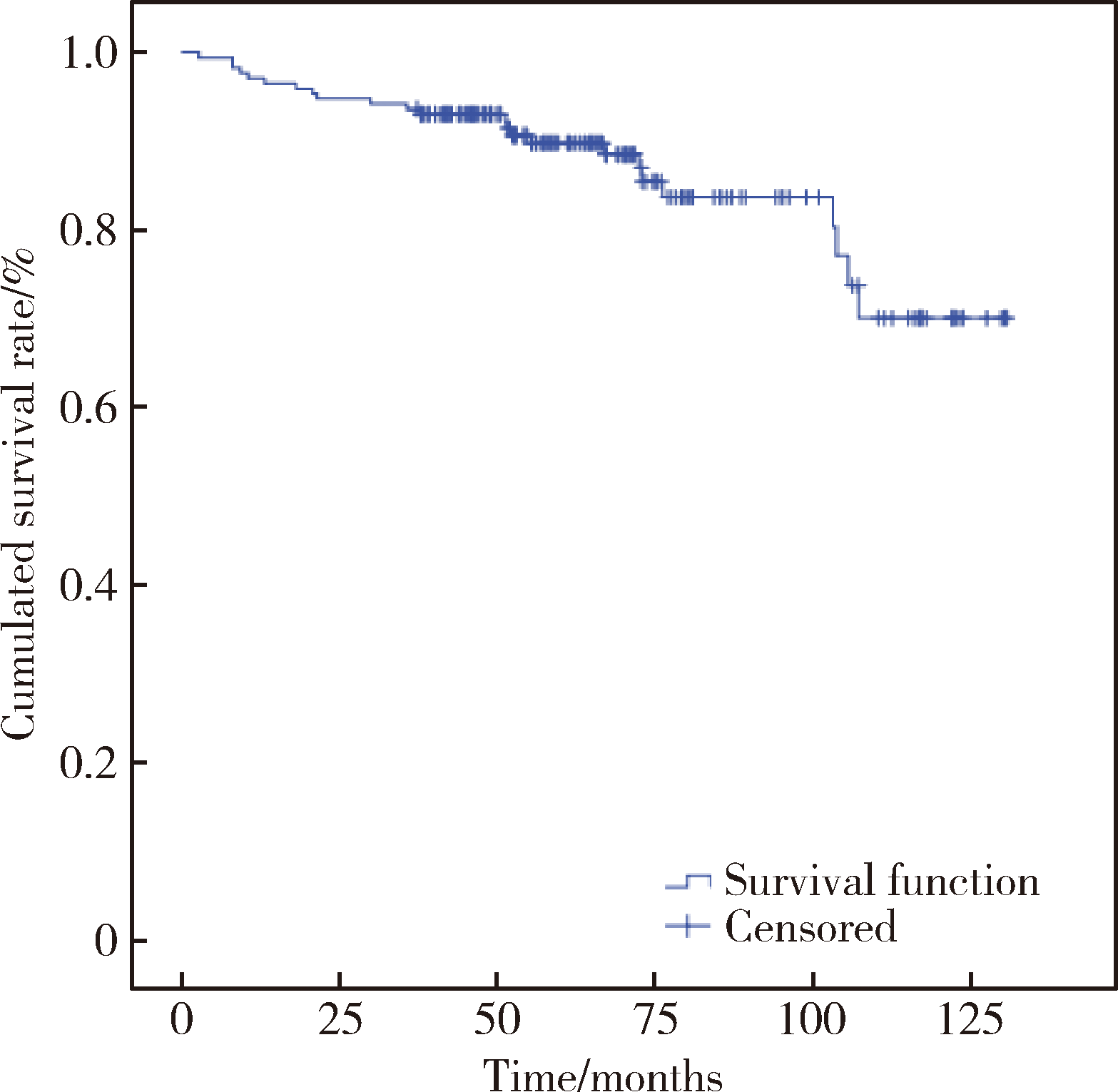
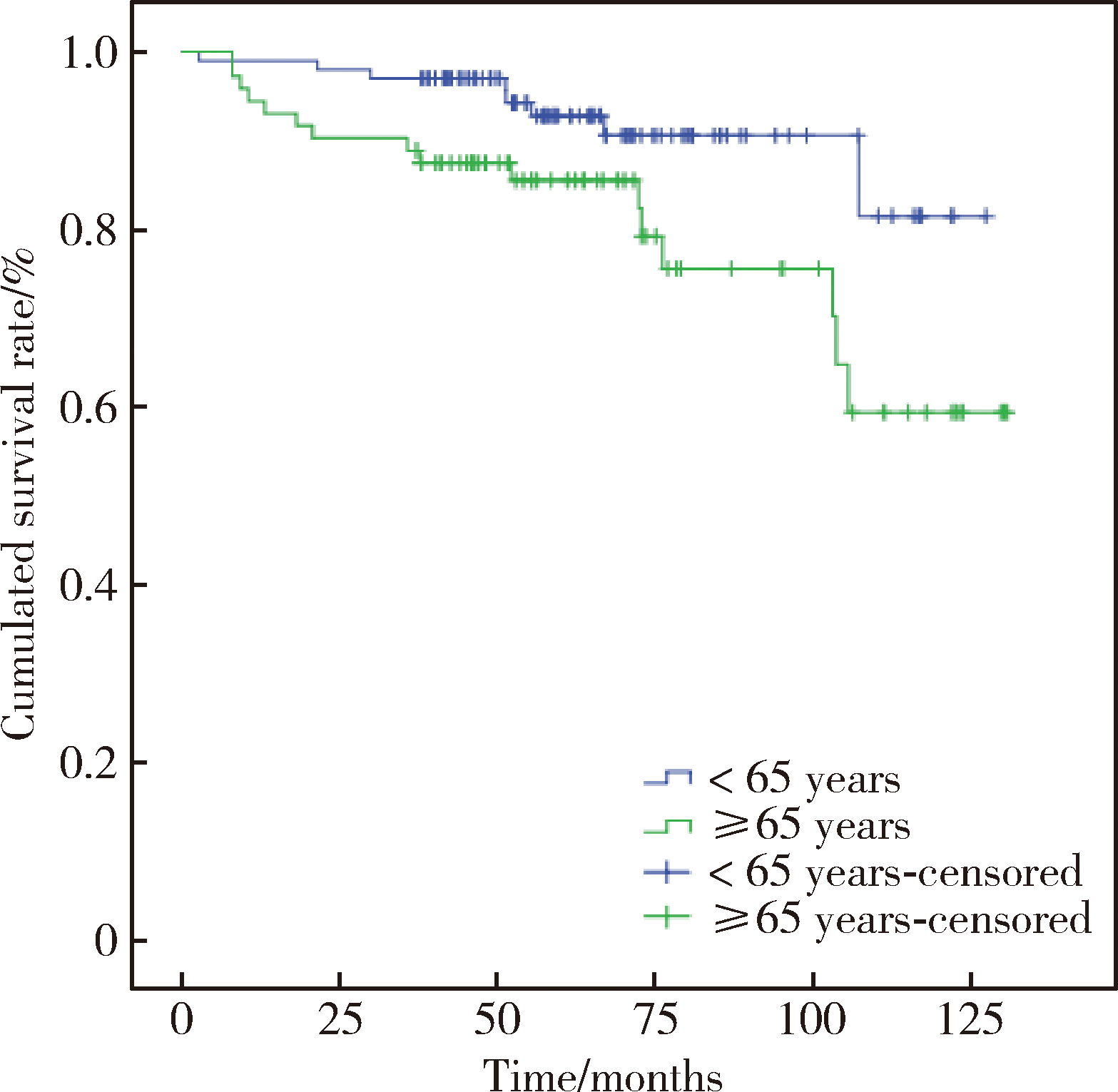
目的:探讨影响恶性孤立性肺结节患者术后生存的因素,为早期肺癌患者的预后危险分层提供参考。方法:选择2006年4月至2013年12月在北京大学第一医院诊治的影像学诊断为孤立性肺结节、经手术病理诊断为非小细胞肺癌Ⅰa期的患者,共172例,对临床及随访资料进行回顾,分析性别、年龄、症状、吸烟、合并症、肿瘤标志物、结节类型、手术方式、结节部位、病理类型、结节大小、分化程度、Ki-67表达水平、EGFR突变等因素对患者生存率的影响。采用Kaplan-Meier生存分析、Cox回归分析评估影响患者生存的预后因素。结果:恶性孤立性肺结节患者的术后3年总生存率为93.6%、5年总生存率为89.8%,Kaplan-Meier生存分析和Cox单因素回归分析显示男性患者的总生存率显著低于女性,老年和高Ki-67增殖指数同样与患者较差的总生存率相关(P<0.05)。Cox多因素分析显示,年龄大于等于65岁和高Ki-67增殖指数是恶性孤立性肺结节术后患者总生存率的独立危险因素(年龄:P=0.023, HR=3.531, 95%CI 1.190~10.472;Ki-67:P=0.004, HR=1.021, 95%CI 1.007~1.035)。结论:对于恶性孤立性肺结节(即Ⅰa期非小细胞肺癌)患者,年龄、性别、Ki-67表达水平是影响恶性孤立性肺结节患者生存的预后因素。将Ki-67增殖指数与临床病理学特征综合考虑可能有助于对恶性孤立性肺结节患者进行更准确的预后危险分层,从而指导治疗方案的制定。
中图分类号:
- R734.2
| [1] | Al-Ameri A, Malhotra P, Thygesen H , et al. Risk of malignancy in pulmonary nodules: a validation study of four prediction models[J]. Lung Cancer, 2015,89(1):27-30. |
| [2] | Perandini S, Soardi GA, Motton M , et al. Solid pulmonary nodule risk assessment and decision analysis: comparison of four prediction models in 285 cases[J]. Eur Radiol, 2016,26(9):3071-3076. |
| [3] | 何权瀛, 高莹慧 . 关于吸烟问题若干名词定义[J]. 中华结核和呼吸杂志, 2009,32(1):56. |
| [4] | Higuchi M, Yaginuma H, Yonechi A , et al. Long-term outcomes after video-assisted thoracic surgery (VATS) lobectomy versus lobectomy via open thoracotomy for clinical stage IA non-small cell lung cancer[J]. J Cardiothorac Surg, 2014,9:88. |
| [5] | Khullar OV, Liu Y, Gillespie T , et al. Survival after sublobar resection versus lobectomy for clinical stage Ⅰa lung cancer: an analysis from the national cancer data base[J]. J Thorac Oncol, 2015,10(11):1625-1633. |
| [6] | Wang BY, Huang JY, Cheng CY , et al. Lung cancer and prognosis in taiwan: a population-based cancer registry[J]. J Thorac Oncol, 2013,8(9):1128-1135. |
| [7] | Yoshida Y, Murayama T, Sato Y , et al. Gender differences in long-term survival after surgery for non-small cell lung cancer[J]. Thorac Cardiovasc Surg, 2016,64(6):507-514. |
| [8] | Ryu JS, Choi CM, Yang SC , et al. Prognostic effect of age on survival of patients with stage I adenocarcinoma of the lung[J]. Tumori, 2012,98(1):99-104. |
| [9] | Dowsett M, Nielsen TO, A’Hern R , et al. Assessment of Ki67 in breast cancer: recommendations from the International Ki67 in breast cancer working group[J]. J Natl Cancer Inst, 2011,103(22):1656-1664. |
| [10] | Luo Y, Ren F, Liu Y , et al. Clinicopathological and prognostic significance of high Ki-67 labeling index in hepatocellular carcinoma patients: a meta-analysis[J]. Int J Clin Exp Med, 2015,8(7):10235-10247. |
| [11] | Pyo JS, Kang G, Sohn JH . Ki-67 labeling index can be used as a prognostic marker in gastrointestinal stromal tumor: a systematic review and meta-analysis[J]. Int J Biol Markers, 2016,31(2):e204-e210. |
| [12] | Ahn HK, Jung M, Ha SY , et al. Clinical significance of Ki-67 and p53 expression in curatively resected non-small cell lung cancer[J]. Tumour Biol, 2014,35(6):5735-5740. |
| [13] | Sofocleous CT, Garg SK, Cohen P , et al. Ki 67 is an independent predictive biomarker of cancer specific and local recurrence-free survival after lung tumor ablation[J]. Ann Surg Oncol, 2013,20(Suppl 3):S676-S683. |
| [14] | Wen S, Zhou W, Li CM , et al. Ki-67 as a prognostic marker in early-stage non-small cell lung cancer in Asian patients: a meta-analysis of published studies involving 32 studies[J]. BMC Cancer, 2015,15:520. |
| [1] | 刘瑾,熊耕砚,唐琦,方冬,李学松,周利群. 上尿路尿路上皮癌中RASSF1A基因启动子区域的甲基化状态及其临床意义[J]. 北京大学学报(医学版), 2016, 48(4): 571-578. |
|
||