北京大学学报(医学版) ›› 2020, Vol. 52 ›› Issue (4): 646-650. doi: 10.19723/j.issn.1671-167X.2020.04.009
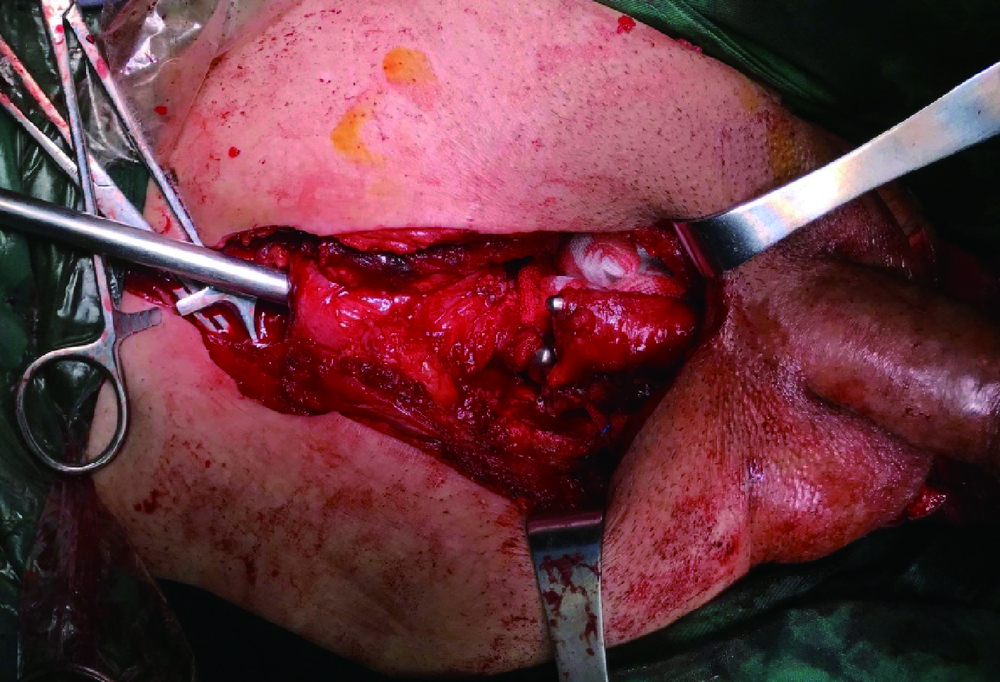
耻骨会阴联合切口后尿道吻合术治疗复杂男性骨盆骨折后尿道离断
王建伟,满立波( ),徐啸,刘振华,何峰,黄广林,翟建坡,周宁,李玮
),徐啸,刘振华,何峰,黄广林,翟建坡,周宁,李玮
- 北京积水潭医院,北京大学第四临床医学院泌尿外科,北京 100096
Combined transperineal and transpubic urethroplasty for patients with complex male pelvic fracture urethral distraction defect
Jian-wei WANG,Li-bo MAN( ),Xiao XU,Zhen-hua LIU,Feng HE,Guang-lin HUANG,Jian-po ZHAI,Ning ZHOU,Wei LI
),Xiao XU,Zhen-hua LIU,Feng HE,Guang-lin HUANG,Jian-po ZHAI,Ning ZHOU,Wei LI
- Department of Urology, Beijing Jishuitan Hospital, the Fourth Medical College of Peking University, Beijing 100096, China
摘要:
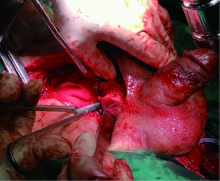
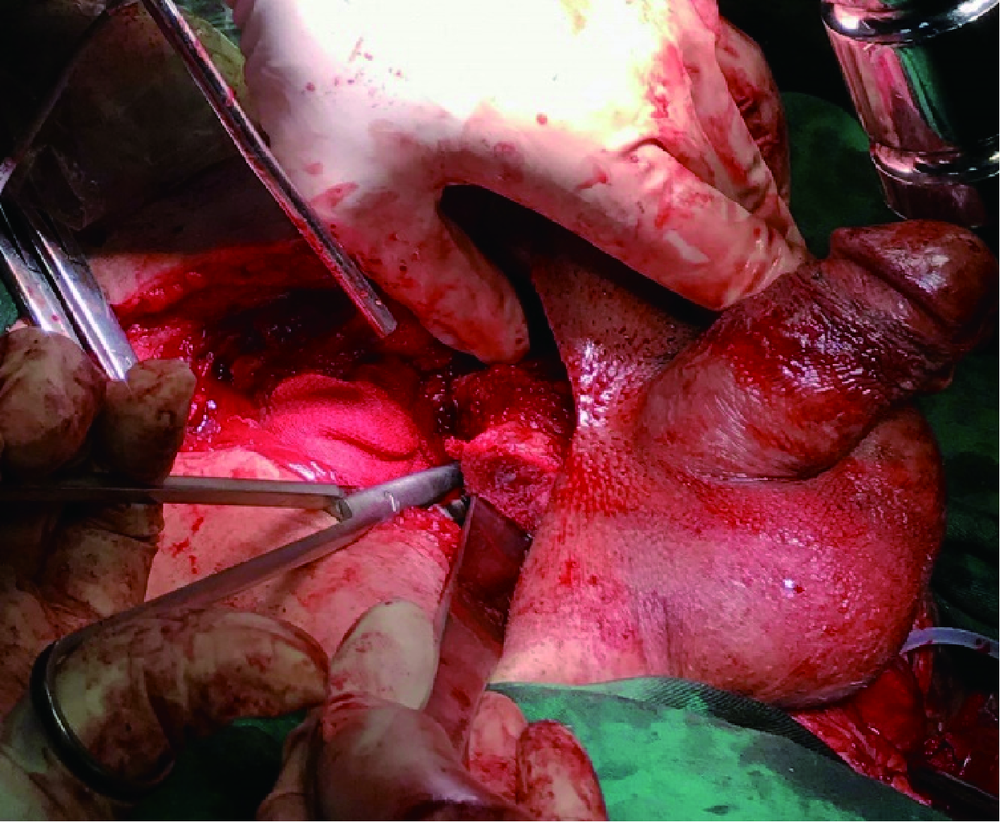
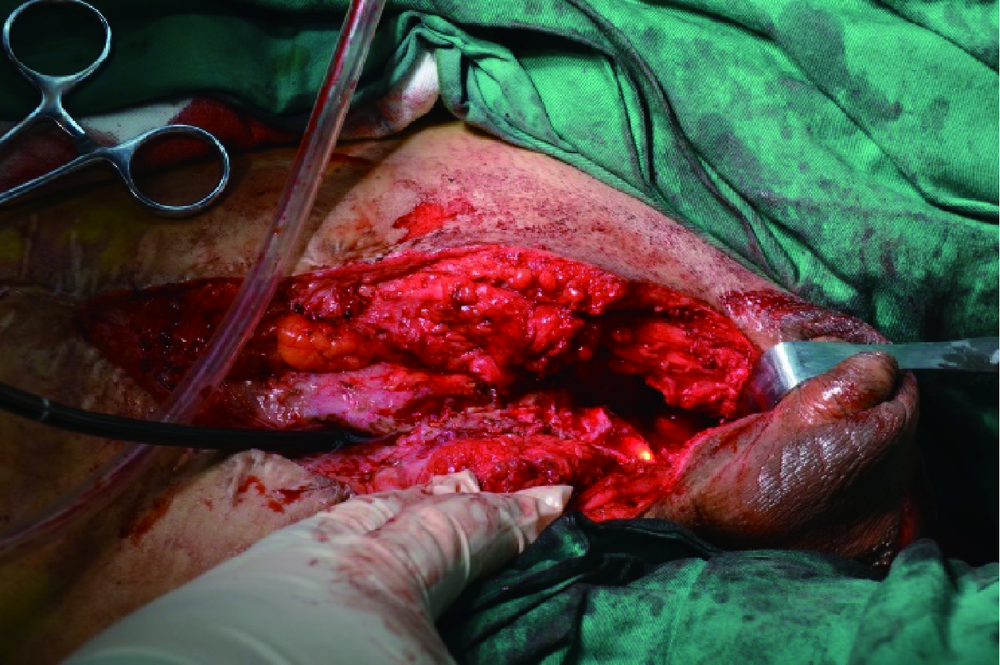
目的: 总结耻骨会阴联合切口耻骨整块切除后尿道吻合治疗复杂男性骨盆骨折后尿道离断(pelvic fracture urethral distraction defect, PFUDD)的临床效果及体会。方法: 回顾性分析2010年1月至2019年12月采用耻骨会阴联合切口后尿道吻合术治疗的复杂PFUDD患者17例,其中合并尿道直肠瘘2例(11.8%)、尿道会阴皮肤瘘1例(5.9%)。既往经会阴后尿道吻合失败6例(35.3%),其中2例(11.8%)为2次开放手术失败;尿道扩张治疗3例(17.6%);内切开治疗1例(5.9%)。所有患者均采用经耻骨会阴联合切口整块切除耻骨再行后吻合尿道。结果: 本组患者平均年龄35.5(21~62)岁,尿道狭窄的长度平均5.5 (4.5~7.0) cm,手术时间平均190 (150~260) min,平均术中估计失血460 (200~1 200) mL。术后局部伤口感染4例(23.5%),下肢静脉血栓1例,患者平均随访27 (7~110)个月。术后平均尿流率22.7 (15.5~40.7) mL/s,合并尿道直肠瘘、尿道会阴瘘等均治愈。1例患者拔管后2周出现尿线变细及尿频、尿急等泌尿系感染症状,行膀胱镜检查示吻合口处狭窄,给予内切开并留置尿管2周,术后随访排尿通畅。本组17例患者手术成功率为94.1%(16/17)。结论: 耻骨会阴联合切口后尿道吻合术治疗复杂男性PFUDD效果明确,成功率为94.1%。此类手术损伤大、耗时长、术后并发症高,适合在区域性尿道修复重建中心开展。
中图分类号:
- R699.6
| [1] | 满立波, 王建伟. 图解尿道成形术 [M]. 北京: 人民卫生出版社, 2018: 43-51. |
| [2] | 王建伟, 满立波, 黄广林, 等. 经会阴三步法手术策略治疗单纯性男性骨盆骨折后尿道离断[J]. 北京大学学报(医学版), 2018,50(4):617-620. |
| [3] |
Gelman J. Tips for successful open surgical reconstruction of posterior urethral disruption injuries[J]. Urol Clin North Am, 2013,40(3):381-392.
doi: 10.1016/j.ucl.2013.04.007 pmid: 23905936 |
| [4] |
Barratt RC, Bernard J, Mundy AR, et al. Pelvic fracture urethral injury in males—mechanisms of injury, management options and outcomes[J]. Transl Androl Urol, 2018,7(Suppl 1):S29-S62.
pmid: 29644168 |
| [5] |
Koraitim MM. Predictors of surgical approach to repair pelvic fracture urethral distraction defects[J]. J Urol, 2009,182(4):1435-1439.
pmid: 19683294 |
| [6] | Horiguchi A. Management of male pelvic fracture urethral injuries: review and current topics[J]. Int J Urol, 2019,26(6):596-607. |
| [7] |
Pierce JM Jr. Exposure of the membranous and posterior urethra by total pubectomy[J]. J Urol, 1962,88:256-258.
pmid: 14486460 |
| [8] |
Koraitim MM. The combined perineo-abdominal transpubic urehtroplasty[J]. Arab J Urol, 2015,13(1):24-26.
pmid: 26019974 |
| [9] | Koraitim MM. Optimising the outcome after anastomotic posterior urethroplasty[J]. Arab J Urol, 2015,13(1):27-31. |
| [10] | Horiguchi A, Edo H, Soga S, et al. Pubourethral stump angle measured on preoperative magnetic resonance imaging predicts urethroplasty type for pelvic fracture urethral injury repair[J]. Urology, 2018,112:198-204. |
| [11] | Barbagli G. History and evolution of transpubic urethroplasty: a lesson for young urologists in training[J]. Eur Urol, 2009,52(5):1290-1292. |
| [12] | Johnsen NV, Moses RA, Ellliott SP, et al. Multicenter analysis of posterior urethroplasty complexity and outcomes following pelvic fracture urethral injury[J]. World J Urol, 2019,38(4):1073-1079. |
| [13] |
Angulo JC, Gómez RG, Nikolavsky D. Reconstruction of membranous urethral strictures[J]. Curr Urol Rep, 2018,19(6):37.
pmid: 29644478 |
| [14] | Mathur RK, Tiwari NS, Odiya SA. Transpubic urethroplasty: a single center experience[J]. Adv Urol, 2014,2014:826710. doi: 10.1155/2014/826710. |
| [15] | Koraitim MM. Complex pelvic fracture urethral distraction defects revisited[J]. Scand J Urol, 2014,48(1):84-89. |
| [16] | Podesta M, Podesta M Jr. Delayed surgical repair of posttraumatic posterior urethral distraction defects in children and adolesents: long-term results [J]. J Pediatr Urol, 2015, 11(2): 67.e1-6. |
| [17] |
Joshi PM, Batra V, Kulkarni SB. Controversies in the management of pelvic fracture urethral distraction defects[J]. Turk J Urol, 2019,45(1):1-6.
pmid: 30668305 |
| [18] |
Kulkarni SB, Surana S, Desai DJ, et al. Management of complex and redo cases of pelvic fracture urethral injuries[J]. Asian J Urol, 2018,5(2):107-117.
pmid: 29736373 |
| [19] |
Gomez RG, Mundy T, Dubey D, et al. SIU/ICUD consultation on urethral strictures: pelvic fracture urethral injuries[J]. Urology, 2014,83(3 Suppl):S48-S58.
doi: 10.1016/j.urology.2013.09.023 pmid: 24210734 |
| [20] |
Pratap A, Agrawal CS, Pandit RK, et al. Factors contributing to a successful outcome of combined abdominal transpubic perineal urethroplasty for complex posterior urethral disruptions[J]. J Urol, 2006,176(6 Pt 1):2514-2517.
pmid: 17085145 |
| [1] | 王建伟,徐啸,鲍正清,刘振华,何峰,黄广林,满立波. 耻骨下缘部分切除辅助后尿道吻合术在男性骨盆骨折后尿道离断修复中的应用[J]. 北京大学学报(医学版), 2021, 53(4): 798-802. |
| [2] | 王建伟,满立波,黄广林,王海,徐啸,朱晓斐,李玮,刘振华. 经会阴三步法手术策略治疗单纯性男性骨盆骨折后尿道离断[J]. 北京大学学报(医学版), 2018, 50(4): 617-620. |
|
||