北京大学学报(医学版) ›› 2022, Vol. 54 ›› Issue (1): 62-67. doi: 10.19723/j.issn.1671-167X.2022.01.010
28例口腔基底样鳞状细胞癌的临床病理分析
- 北京大学口腔医学院·口腔医院口腔病理科,国家口腔医学中心,国家口腔疾病临床医学研究中心,口腔数字化医疗技术和材料国家工程实验室,口腔数字医学北京市重点实验室,国家卫生健康委员会口腔医学计算机应用工程技术研究中心,国家药品监督管理局口腔生物材料重点实验室,北京 100081
Clinicopathological study in 28 cases of oral basaloid squamous cell carcinomas
ZHOU Chuan-xiang,ZHOU Zheng,ZHANG Ye,LIU Xiao-xiao,GAO Yan( )
)
- Department of Oral Pathology, Peking University School and Hospital of Stomatology & National Center of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology & NHC Research Center of Engineering and Technology for Computerized Dentistry & NMPA Key Laboratory for Dental Materials, Beijing 100081, China
摘要:
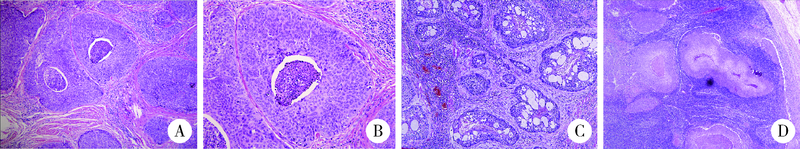
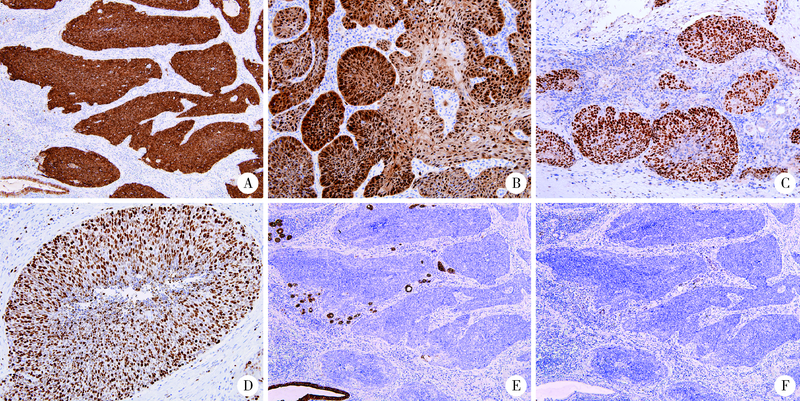
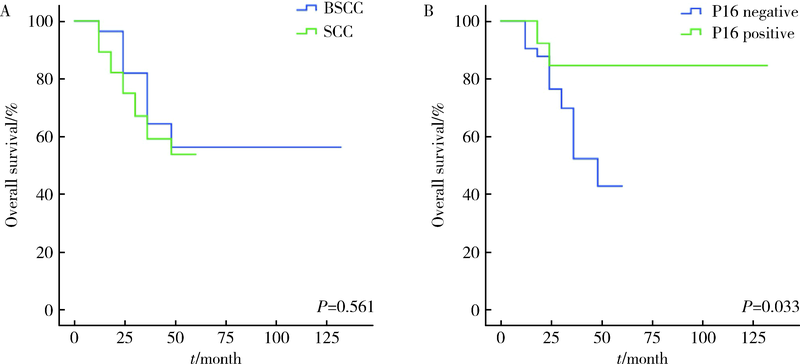
目的: 回顾性分析基底样鳞状细胞癌临床病理特征及预后相关因素。方法: 回顾性分析2002年1月至2020年12月在北京大学口腔医学院诊治并经病理确诊为基底样鳞状细胞癌患者的临床病理资料。选取诊断明确且组织学不伴有其他类型杂交瘤,并有明确手术治疗史及完善临床病理资料的基底样鳞状细胞癌28例,分析其临床病理特征,应用免疫组织化学染色筛选可用于鉴别诊断的特异性免疫标记,应用统计学方法进行生存分析,评估预后相关因素,同时随机选取28例临床分期相同的传统鳞状细胞癌患者作为对照组。结果: 28例基底样鳞状细胞癌最常发生的部位是舌及口底,为11例(11/28,39.3%),其余牙龈6例(6/28, 21.4%)、颊部5例(5/28, 17.9%)、腭部4例(4/28, 14.3%)、口咽部2例(2/28, 7.1%)。患者多为中晚期, 12例为Ⅱ期,16例为Ⅲ~Ⅳ期。经组织病理学检查证实伴淋巴结转移者12例,占总病例数42.9%(12/28),局部复发者9例,伴远处转移者1例(转移至肺)。28例传统鳞状细胞癌患者中经组织病理学检查证实伴淋巴结转移者13例,占总病例数46.4%(13/28)。局部复发者5例,伴远处转移者3例,其中2例转移至肺、1例转移至脑。临床分期相同的基底样鳞状细胞癌组和传统鳞状细胞癌组患者5年总生存率分别为54.6%、53.8%。基底样鳞状细胞癌组织学上表现为基底样细胞构成的实性癌巢,癌巢中心一般不形成角化,常可见粉刺样坏死结构。28例基底样鳞状细胞癌均呈现CK5/6、P63强阳性表达,而神经内分泌标志物CgA和Syn阴性表达,其中8例呈P16阳性表达,1例局灶阳性表达SOX10,但CK7阴性。结论: 口腔基底样鳞状细胞癌中晚期患者多见,淋巴结转移率较高,但与相同临床分期的传统鳞状细胞癌总生存率差异无统计学意义;P16阳性患者与人乳头瘤病毒感染相关,预后较好;CK7与SOX10免疫组织化学可用于基底样鳞状细胞癌与实性型腺样囊性癌的鉴别诊断。
中图分类号:
- R780.2
| [1] |
Wain SL, Kier R, Vollmer RT, et al. Basaloid-squamous carcinoma of the tongue, hypopharynx, and larynx: report of 10 cases[J]. Hum Pathol, 1986, 17(11):1158-1166.
pmid: 3770734 |
| [2] |
Paulino AF, Singh B, Shah JP, et al. Basaloid squamous cell carcinoma of the head and neck[J]. Laryngoscope, 2000, 110(9):1479-1482.
pmid: 10983946 |
| [3] |
Soriano E, Faure C, Lantuejoul S, et al. Course and prognosis of basaloid squamous cell carcinoma of the head and neck: a case-control study of 62 patients[J]. Eur J Cancer, 2008, 44(2):244-250.
doi: 10.1016/j.ejca.2007.11.008 |
| [4] |
Ramqvist T, Näsman A, Franzeén B, et al. Protein expression in tonsillar and base of tongue cancer and in relation to human papillomavirus (HPV) and clinical outcome.[J]. Int J Mol Sci, 2018, 19(4):978.
doi: 10.3390/ijms19040978 |
| [5] | Näsman A, Bersani C, Lindquist D, et al. Human papillomavirus and potentially relevant biomarkers in tonsillar and base of tongue squamous cell carcinoma[J]. Anticancer Res, 2017, 37(10):5319-5328. |
| [6] |
Xu Y, Zhao H, Tong Y, et al. Comparative analysis of clinicopathological characteristics, survival features, and protein expression between basaloid and squamous cell carcinoma of the esophagus[J]. Int J Gen Med, 2021, 14:3929-3939.
doi: 10.2147/IJGM.S314054 |
| [7] |
Linton OR, Moore MG, Brigance JS, et al. Prognostic significance of basaloid squamous cell carcinoma in head and neck can-cer[J]. JAMA Otolaryngol Head Neck Surg, 2013, 139(12):1306-1311.
doi: 10.1001/jamaoto.2013.5308 |
| [8] |
Thariat J, Badoual C, Faure C, et al. Basaloid squamous cell carcinoma of the head and neck: role of HPV and implication in treatment and prognosis[J]. J Clin Pathol, 2010, 63(10):857-866.
doi: 10.1136/jcp.2010.078154 pmid: 20876315 |
| [9] |
de Sampaio Góes FC, Oliveira DT, Dorta RG, et al. Prognoses of oral basaloid squamous cell carcinomas and squamous cell carcinoma: a comparison[J]. Arch Otolaryngol Head Neck Surg, 2004, 130(1):83-86.
doi: 10.1001/archotol.130.1.83 |
| [10] |
Yu GY, Gao Y, Peng X, et al. A clinicopathologic study on basaloid squamous cell carcinoma in the oral and maxillofacial region[J]. Int J Oral Maxillofac Surg, 2008, 37(11):1003-1008.
doi: 10.1016/j.ijom.2008.05.019 |
| [11] | 代璐岭, 杨秀秀, 赵好为, 等. 牙龈基底细胞样鳞状细胞癌1例[J]. 华西口腔医学杂志, 2020, 38(3):347-350. |
| [12] | Sato F, Bhawal UK, Tojyo I, et al. Differential expression of claudin-4, occludin, SOX2 and proliferating cell nuclear antigen between basaloid squamous cell carcinoma and squamous cell carcinoma[J]. Mol Med Rep, 2019, 20(2):1977-1985. |
| [13] |
Schuch LF, Nóbrega KHS, Gomes APN, et al. Basaloid squamous cell carcinoma: a 31-year retrospective study and analysis of 214 cases reported in the literature[J]. Oral Maxillofac Surg, 2020, 24(1):103-108.
doi: 10.1007/s10006-020-00828-9 |
| [14] |
Lee JH, Kang HJ, Yoo CW, et al. PLAG1, SOX10, and Myb expression in benign and malignant salivary gland neoplasms[J]. J Pathol Transl Med, 2019, 53(1):23-30.
doi: 10.4132/jptm.2018.10.12 |
| [15] |
Hsieh MS, Lee YH, Chang YL. SOX10-positive salivary gland tumors: a growing list, including mammary analogue secretory carcinoma of the salivary gland, sialoblastoma, low-grade salivary duct carcinoma, basal cell adenoma/adenocarcinoma, and a subgroup of mucoepidermoid carcinoma[J]. Hum Pathol, 2016, 56:134-142.
doi: 10.1016/j.humpath.2016.05.021 |
| [16] |
Adkins BD, Geromes A, Zhang LY, et al. SOX10 and GATA3 in adenoid cystic carcinoma and polymorphous adenocarcinoma[J]. Head Neck Pathol, 2020, 14(2):406-411.
doi: 10.1007/s12105-019-01046-w pmid: 31222589 |
| [17] |
Nakaguro M, Tada Y, Faquin WC, et al. Salivary duct carcinoma: updates in histology, cytology, molecular biology, and treatment[J]. Cancer Cytopathol, 2020, 128(10):693-703.
doi: 10.1002/cncy.22288 pmid: 32421944 |
| [18] |
Boon E, Bel M, van Boxtel W, et al. A clinicopathological study and prognostic factor analysis of 177 salivary duct carcinoma patients from The Netherlands[J]. Int J Cancer, 2018, 143(4):758-766.
doi: 10.1002/ijc.31353 |
| [19] |
Santana T, Pavel A, Martinek P, et al. Biomarker immunoprofile and molecular characteristics in salivary duct carcinoma: clinicopathological and prognostic implications[J]. Hum Pathol, 2019, 93:37-47.
doi: 10.1016/j.humpath.2019.08.009 |
| [20] |
Villada G, Kryvenko ON, Campuzano-Zuluaga G, et al. A limited immunohistochemical panel to distinguish basal cell carcinoma of cutaneous origin from basaloid squamous cell carcinoma of the head and neck[J]. Appl Immunohistochem Mol Morphol, 2018, 26(2):126-131.
doi: 10.1097/PAI.0000000000000394 |
| [21] |
Mendelsohn AH, Lai CK, Shintaku IP, et al. Histopathologic findings of HPV and p16 positive HNSCC[J]. Laryngoscope, 2010, 120(9):1788-1794.
doi: 10.1002/lary.21044 |
| [22] |
Begum S, Westra WH. Basaloid squamous cell carcinoma of the head and neck is a mixed variant that can be further resolved by HPV status[J]. Am J Surg Pathol, 2008, 32(7):1044-1050.
doi: 10.1097/PAS.0b013e31816380ec |
| [23] |
Lai K, Killingsworth M, Matthews S, et al. Differences in survival outcome between oropharyngeal and oral cavity squamous cell carcinoma in relation to HPV status[J]. J Oral Pathol Med, 2017, 46(8):574-582.
doi: 10.1111/jop.2017.46.issue-8 |
| [24] |
Duncan LD, Winkler M, Carlson ER, et al. P16 immunohistochemistry can be used to detect human papillomavirus in oral cavity squamous cell carcinoma[J]. J Oral Maxillofac Surg, 2013, 71(8):1367-1375.
doi: 10.1016/j.joms.2013.02.019 |
| [1] | 苏俊琪,王晓颖,孙志强. 舌鳞状细胞癌根治性切除术后患者预后预测列线图的构建与验证[J]. 北京大学学报(医学版), 2024, 56(1): 120-130. |
| [2] | 李辉,彭敏,武娇,张青霞,宁博涵,董颖. p16/Ki67细胞学双染在子宫颈癌前病变及宫颈癌筛查中的应用[J]. 北京大学学报(医学版), 2023, 55(6): 1144-1148. |
| [3] | 卢汉,张建运,杨榕,徐乐,李庆祥,郭玉兴,郭传瑸. 下颌牙龈鳞状细胞癌患者预后的影响因素[J]. 北京大学学报(医学版), 2023, 55(4): 702-707. |
| [4] | 苏俊琪,宋扬,谢尚. 口腔鳞状细胞癌患者修复重建术后感染的病原学特征及感染风险预测模型的构建[J]. 北京大学学报(医学版), 2022, 54(1): 68-76. |
| [5] | 苏雷震,陈洁,李显,季平. 沙利霉素对口腔鳞癌细胞增殖和凋亡的影响[J]. 北京大学学报(医学版), 2020, 52(5): 902-906. |
| [6] | 陶船思博,董凡,王佃灿,郭传瑸. 红外热成像技术诊断口腔鳞状细胞癌颈淋巴结转移[J]. 北京大学学报(医学版), 2019, 51(5): 959-963. |
| [7] | 刘洋,高岩,陈学杰,华红. 脱落细胞DNA 定量分析在口腔潜在恶性疾病诊断中的准确性[J]. 北京大学学报(医学版), 2019, 51(1): 16-20. |
| [8] | 张春凤,刘云,陆敏,杜晓娟. hUTP14a在非小细胞肺癌组织中的表达[J]. 北京大学学报(医学版), 2019, 51(1): 145-150. |
| [9] | 梁凌云*, 杜辉*, 王纯, 张薇, 陈芸, 渠新风, 杨斌, 吴波, 吴若松, Jerome L. Belinson, 吴瑞芳. 深圳人群人乳头瘤病毒感染亚型分布与宫颈上皮内瘤变现况横断面调查[J]. 北京大学学报(医学版), 2013, 45(1): 114-118. |
| [10] | 吕文平, 周开伦, 高彬, 陈永亮, 向昕, 苏明, 董家鸿. HBx诱导p16INK4a高甲基化在Chang细胞株恶性转化倾向中的作用[J]. 北京大学学报(医学版), 2012, 44(6): 932-936. |
| [11] | 崔素萍, 王花丽, 彭伟, 刘海静, 侯琳, 张波. 乳腺癌组织P16异常表达的相关分析[J]. 北京大学学报(医学版), 2012, 44(5): 755-759. |
| [12] | 郭艳利, 耿力, 游珂, 乔杰, 刘从容. 外阴和阴道上皮内瘤变的临床初步研究[J]. 北京大学学报(医学版), 2009, 41(5): 561-564. |
| [13] | 董采萱, 邓大君, 周静, 张联, 马峻岭, 潘凯枫, 游伟程. 人群胃黏膜不确定性异型增生和异型增生组织p16甲基化及与幽门螺杆菌等暴露因素相关分析[J]. 北京大学学报(医学版), 2008, 40(3): 280-284. |
| [14] | 赵英芳, 田新霞, 杜娟, 张云岗, 刘松年, 林杰, 郑杰. 胃癌中p16INK4a和RB基因甲基化状况及其表达[J]. 北京大学学报(医学版), 2003, 35(4): 382-385. |
| [15] | 刘波, 李运海, 栾文忠, 梁冶矢, 虞有智, 郑爱萍. P16蛋白和Ki-67抗原在人脑胶质瘤中的表达及其意义[J]. 北京大学学报(医学版), 2003, 35(2): 223-224. |
|
||