北京大学学报(医学版) ›› 2023, Vol. 55 ›› Issue (6): 1082-1087. doi: 10.19723/j.issn.1671-167X.2023.06.020
胃超声检查评估剖宫产产妇术前饮用碳水化合物后胃排空的效果
- 1. 北京大学国际医院麻醉科,北京 102206
2. 北京大学国际医院妇产科,北京 102206
Evaluation of gastric emptying after drinking carbohydrates before cesarean section by gastric ultrasonography
Yue WEI1,Lan YAO1,Xi LU1,Jun WANG1,Li LIN2,Kun-peng LIU1,*( )
)
- 1. Department of Anesthesiology, Peking University International Hospital, Beijing 102206, China
2. Department of Obstetrics and Gynecology, Peking University International Hospital, Beijing 102206, China
摘要:
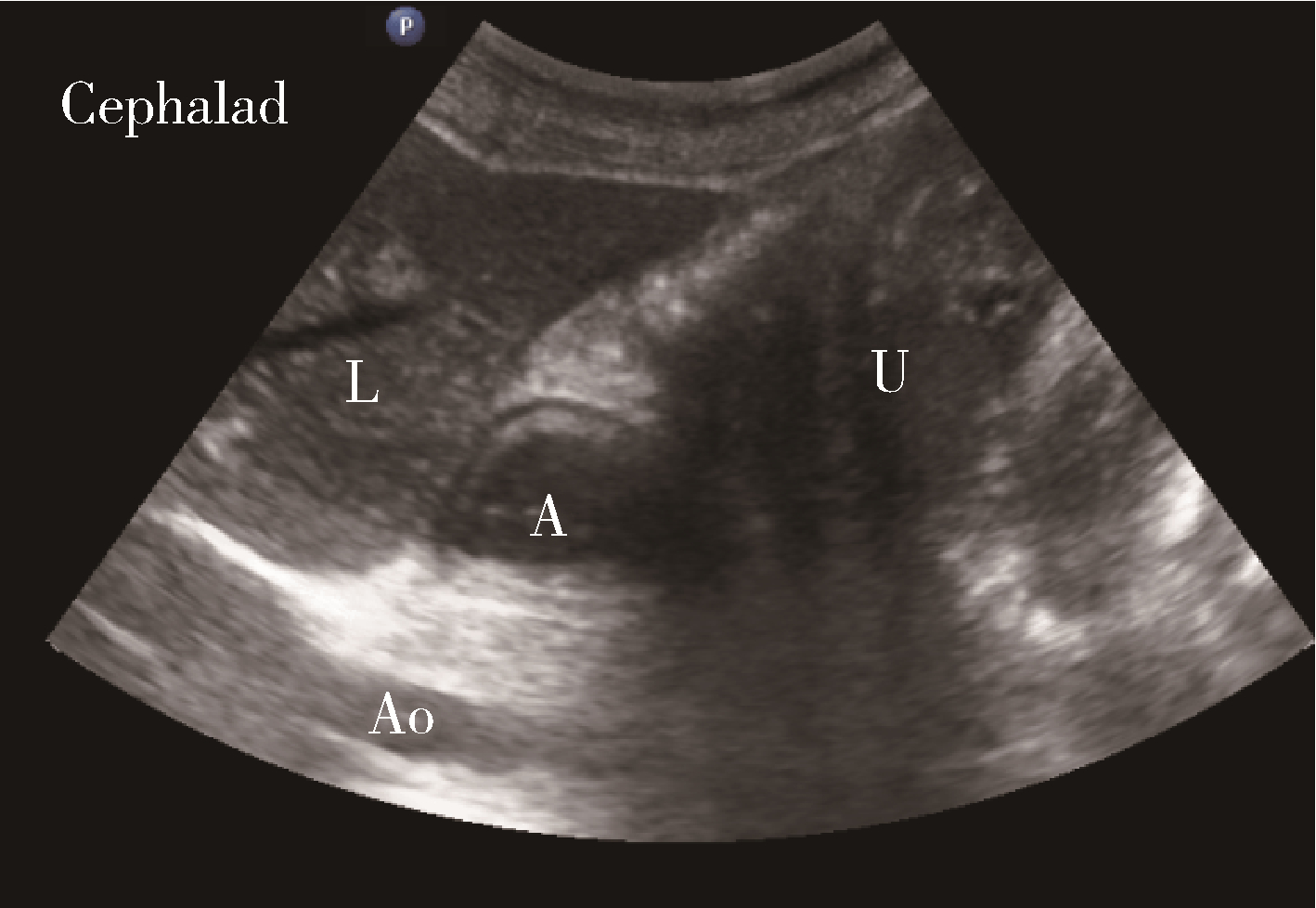
目的: 探讨胃窦部超声检查评估剖宫产产妇术前2 h口服300 mL碳水化合物后胃排空的效果, 并分析影响产妇胃排空的风险因素。方法: 选择2020年8月至2021年2月在北京大学国际医院行择期剖宫产的产妇80例, 年龄22~43岁, 体重指数(body mass index, BMI)<35 kg/m2, 孕周≥36周, 美国麻醉医师学会(American Society of Anesthesiologists, ASA)分级Ⅰ或Ⅱ级, 随机分为干预组和对照组, 每组40例。干预组产妇于术前一日22:00后禁食, 术日在预期手术开始前2 h口服碳水化合物300 mL; 对照组产妇于术前一日22:00后禁食禁饮。两组患者入手术室后行术前干渴感及饥饿感的视觉模拟评分(visual analogue scale, VAS)。麻醉前行胃窦部超声检查, 分别在半坐位和右侧卧位下测量胃窦横截面积(cross-sectional area, CSA), 并进一步计算两组患者胃容量(gastric volume, GV)及胃容量/体质量(gastric volume /weight, GV/W), 并进行Perlas A半定量评级。记录患者入室(T0)、麻醉后5 min(T1)、胎儿剖出即刻(T2)、手术结束(T3)时的血压和心率。记录术中、术后24 h恶心呕吐的发生情况。结果: 两组各有1例患者无法清晰显示胃窦部, 余78例患者可以进行CSA测量及Perlas A半定量评级。半坐位下, 干预组和对照组的CSA分别为(5.07±1.73) cm2和(5.24±1.96) cm2; 右侧卧位下, 干预组和对照组的CSA分别为(7.32±2.17) cm2和(7.25±2.24) cm2, GV分别为(91.74±32.34) mL和(90.07±31.68) mL, GV/W分别为(1.27±0.40) mL/kg和(1.22±0.41) mL/kg, 上述指标两组间差异均无统计学意义(P>0.05)。Perlas A半定量评级: 干预组0级20例(51.3%), 1级16例(41%), 2级3例(7.7%); 对照组0级22例(56.4%), 1级15例(38.5%), 2级2例(5.1%), 两组评级构成比差异无统计学意义(P>0.05)。Perlas A半定量评级为2级的患者(干预组3例及对照组2例), 麻醉前静脉注射甲氧氯普胺0.2 mg/kg, 均未发生反流误吸。与对照组比较, 干预组术前干渴感、饥饿感VAS明显降低(P<0.05)。术中各观察时点血压、心率两组差异无统计学意义(P>0.05), 术中低血压发生率两组差异无统计学意义(P>0.05)。术中、术后24 h恶心的发生率两组差异无统计学意义(P>0.05)。结论: 胃窦部超声检查能为剖宫产围术期产妇判断胃排空情况提供客观依据。剖宫产产妇术前2 h饮用300 mL碳水化合物, 可减少患者不适, 同时不增加麻醉前GV和反流误吸风险, 临床效果更好。
中图分类号:
- R614.3
| 1 |
Nygren J , Thacker J , Carli F , et al. Guidelines for perioperative care in elective rectal/pelvic surgery: Enhanced Recovery After Surgery (ERAS®) Society recommendation[J]. Clin Nutr, 2012, 31 (6): 801- 816.
doi: 10.1016/j.clnu.2012.08.012 |
| 2 |
Bouvet L , Mazoit JX , Chassard D , et al. Clinical assessment of the ultrasonographic measurement of antral area for estimating preoperative gastric content and volume[J]. Anesthesiology, 2011, 114 (5): 1086- 1092.
doi: 10.1097/ALN.0b013e31820dee48 |
| 3 |
Perlas A , Davis L , Khan M , et al. Gastric sonography in the fasted surgical patient: A prospective descriptive study[J]. Anesth Analg, 2011, 113 (1): 93- 97.
doi: 10.1213/ANE.0b013e31821b98c0 |
| 4 |
Perlas A , Mitsakakis N , Liu L , et al. Validation of a mathematical model for ultrasound assessment of gastric volume by gastroscopic examination[J]. Anesth Analg, 2013, 116 (2): 357- 363.
doi: 10.1213/ANE.0b013e318274fc19 |
| 5 |
van de Putte P , Perlas A . Ultrasound assessment of gastric content and volume[J]. Br J Anaesth, 2014, 113 (1): 12- 22.
doi: 10.1093/bja/aeu151 |
| 6 |
Gola W , Domagala M , Cugowski A . Ultrasound assessment of gastric emptying and the risk of aspiration of gastric contents in the perioperative period[J]. Anaesthesiol Intensive Ther, 2018, 50 (4): 297- 302.
doi: 10.5603/AIT.a2018.0029 |
| 7 |
Apfelbaum JL , Hawkins JL , Agarkar M , et al. Practice guidelines for obstetric anesthesia: An updated report by the American Society of Anesthesiologists task force on obstetric anesthesia and the Society for Obstetric Anesthesia and Perinatology[J]. Anesthesiology, 2016, 124 (2): 270- 300.
doi: 10.1097/ALN.0000000000000935 |
| 8 | 刘平, 干卓坤. 超声评估胃容量及胃内容物性质的研究[J]. 中国医学影像学杂志, 2016, 24 (4): 285- 288. |
| 9 |
Kruisselbrink R , Arzola C , Endersby R , et al. Intra- and interrater reliability of ultrasound assessment of gastric volume[J]. Anesthesiology, 2014, 121 (1): 46- 51.
doi: 10.1097/ALN.0000000000000193 |
| 10 |
Perlas A , Chan VW , Lupu CM , et al. Ultrasound assessment of gastric content and volume[J]. Anesthesiology, 2009, 111 (1): 82- 89.
doi: 10.1097/ALN.0b013e3181a97250 |
| 11 |
Arzola C , Cubillos J , Perlas A , et al. Interrater reliability of qua-litative ultrasound assessment of gastric content in the third trimester of pregnancy[J]. Br J Anaesth, 2014, 113 (6): 1018- 1023.
doi: 10.1093/bja/aeu257 |
| 12 |
Arzola C , Perlas A , Siddiqui NT , et al. Bedside gastric ultrasonography in term pregnant women before elective cesarean deli-very: A prospective cohort study[J]. Anesth Analg, 2015, 121 (3): 752- 758.
doi: 10.1213/ANE.0000000000000818 |
| 13 |
Roukhomovsky M , Zieleskiewicz L , Diaz A , et al. Ultrasound examination of the antrum to predict gastric content volume in the third trimester of pregnancy as assessed by MRI: A prospective cohort study[J]. Eur J Anaesthesiol, 2018, 35 (5): 379- 389.
doi: 10.1097/EJA.0000000000000749 |
| 14 |
Popivanov P , Irwin R , Walsh M , et al. Gastric emptying of carbohydrate drinks in term parturients before elective caesarean deli-very: An observational study[J]. Int J Obstet Anesth, 2020, 41, 29- 34.
doi: 10.1016/j.ijoa.2019.07.010 |
| 15 | 王以瑞, 符新春, 郑芝, 等. 口服碳水化合物溶液的容量与足月产妇胃排空时间的关系[J]. 中华医学杂志, 2018, 98 (26): 2083- 2087. |
| 16 |
Amaral CK , Benevides ML , Benevides MM , et al. Ultrasound assessment of gastric antrum in term pregnant women before elective cesarean section[J]. Rev Bras Anestesio, 2019, 69 (3): 266- 271.
doi: 10.1016/j.bjan.2019.03.001 |
| 17 |
Hakak S , McCaul CL , Crowley L . Ultrasonographic evaluation of gastric contents in term pregnant women fasted for six hours[J]. Int J Obstet Anesth, 2018, 34, 15- 20.
doi: 10.1016/j.ijoa.2018.01.004 |
| 18 |
Shiraishi T , Kurosaki D , Nakamura M , et al. Gastric fluid volume change after oral rehydration solution intake in morbidly obese and normal controls: A magnetic resonance imaging-based analysis[J]. Anesth Analg, 2017, 124 (4): 1174- 1178.
doi: 10.1213/ANE.0000000000001886 |
| [1] | 魏越,陆希,张静,刘鲲鹏,王永军,姚兰. 术前2 h口服碳水化合物对妇科腹腔镜特殊体位手术患者胃容量及反流误吸风险的影响[J]. 北京大学学报(医学版), 2023, 55(5): 893-898. |
|
||