北京大学学报(医学版) ›› 2024, Vol. 56 ›› Issue (4): 567-574. doi: 10.19723/j.issn.1671-167X.2024.04.004
双参数MRI改良PI-RADS评分4分和5分病灶的最大径对临床有意义前列腺癌的预测效果
田宇轩1,阮明健1,刘毅1,李德润1,吴静云2,沈棋1,范宇1,3,*( ),金杰1,*(
),金杰1,*( )
)
- 1. 北京大学第一医院泌尿外科,北京大学泌尿外科研究所,国家泌尿男生殖系肿瘤中心,北京 100034
2. 北京大学第一医院影像科,北京 100034
3. 北京大学第一医院临床药物试验机构,北京 100034
Predictive effect of the dual-parametric MRI modified maximum diameter of the lesions with PI-RADS 4 and 5 on the clinically significant prostate cancer
Yuxuan TIAN1,Mingjian RUAN1,Yi LIU1,Derun LI1,Jingyun WU2,Qi SHEN1,Yu FAN1,3,*( ),Jie JIN1,*(
),Jie JIN1,*( )
)
- 1. Department of Urology, Peking University First Hospital; Institute of Urology, Peking University; National Urological Cancer Center, Beijing 100034, China
2. Department of Radiology, Peking University First Hospital, Beijing 100034, China
3. Drug Clinical Trial Institution, Peking University First Hospital, Beijing 100034, China
摘要:
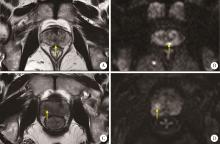
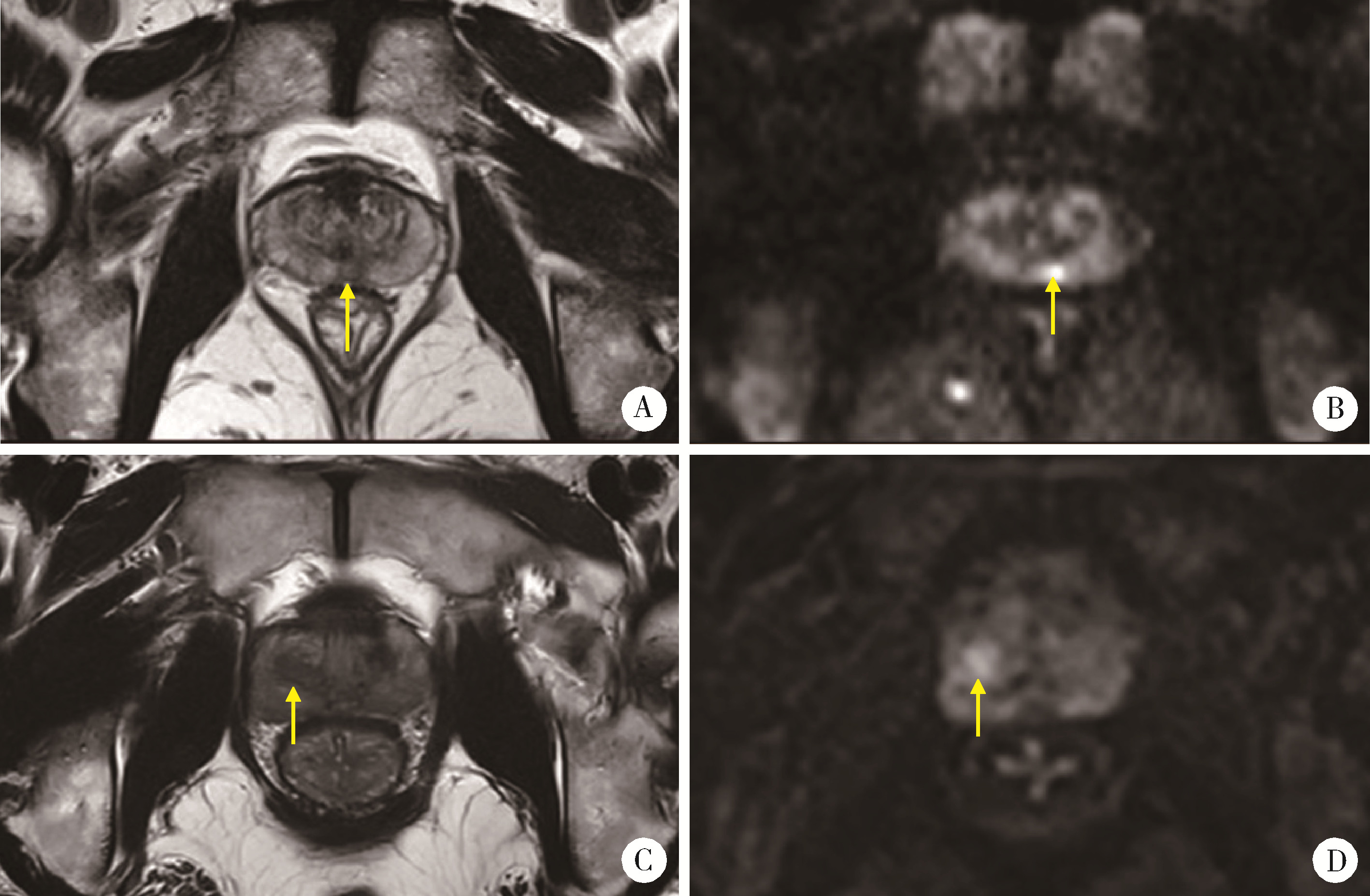
目的: 评估前列腺影像报告和数据评分系统(prostate imaging reporting and data system,PI-RADS)中将病灶最大径15 mm作为4分升级为5分标准的合理性并进行改良,以提升对临床有意义前列腺癌(clinical significant prostate cancer,csPCa)的预测效果。方法: 回顾性分析北京大学第一医院2019—2022年间接受前列腺MRI检查及穿刺的患者,将这组患者作为训练集,2023年的患者作为验证集,对病灶进行定位及测量最大径。采用受试者操作特征(receiver operating characteristics,ROC)曲线计算出病灶最大径预测csPCa的曲线下面积(area under curve,AUC)及最佳截断值,采用倾向性评分匹配(propensity score matching, PSM)缩小组间差异,在验证集中进行诊断效能的比较。结果: 训练集的589例患者中,358例(60.8%)的病灶位于外周带,231例(39.2%)位于移行带,496例(84.2%)为csPCa病变。外周带病灶的中位直径小于移行带病灶(14 mm vs. 19 mm,P < 0.001)。ROC分析最大径对csPCa的预测效果,外周带病灶(AUC=0.709)与移行带病灶(AUC=0.673)相比差异无统计学意义(P=0.585),计算得出外周带病灶的截断值为11.5 mm,移行带病灶为16.5 mm。通过在验证集中计算截断值对应的约登指数(Youden index),发现按病灶位置进行分层可以取得更好的预测效果,计算净重新分类指数(net reclassification index, NRI)为0.170。结论: 将15 mm作为病灶PI-RADS评分4分升级为5分的标准过于笼统,外周带病灶的截断值小于移行带病灶,应考虑对不同位置的病灶分开设定截断值。
中图分类号:
- R737.25
| 1 |
Sung H , Ferlay J , Siegel RL , et al. Global cancer statistics 2020: Globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2021, 71 (3): 209- 249.
doi: 10.3322/caac.21660 |
| 2 |
Culp MB , Soerjomataram I , Efstathiou JA , et al. Recent global patterns in prostate cancer incidence and mortality rates[J]. Eur Urol, 2020, 77 (1): 38- 52.
doi: 10.1016/j.eururo.2019.08.005 |
| 3 |
Schaeffer EM , Srinivas S , Adra N , et al. Prostate cancer, version 4.2023, NCCN clinical practice guidelines in oncology[J]. J Natl Compr Canc Netw, 2023, 21 (10): 1067- 1096.
doi: 10.6004/jnccn.2023.0050 |
| 4 |
Elkhoury FF , Felker ER , Kwan L , et al. Comparison of targeted vs systematic prostate biopsy in men who are biopsy naive: The prospective assessment of image registration in the diagnosis of prostate cancer (PAIREDCAP) study[J]. JAMA Surg, 2019, 154 (9): 811- 818.
doi: 10.1001/jamasurg.2019.1734 |
| 5 |
Mehralivand S , Bednarova S , Shih JH , et al. Prospective evaluation of PI-RADSTM version 2 using the International Society of Urological Pathology prostate cancer grade group system[J]. J Urol, 2017, 198 (3): 583- 590.
doi: 10.1016/j.juro.2017.03.131 |
| 6 |
Turkbey B , Rosenkrantz AB , Haider MA , et al. Prostate imaging reporting and data system version 2.1: 2019 update of prostate imaging reporting and data system version 2[J]. Eur Urol, 2019, 76 (3): 340- 351.
doi: 10.1016/j.eururo.2019.02.033 |
| 7 |
Weinreb JC , Barentsz JO , Choyke PL , et al. PI-RADS Prostate Imaging: Reporting and data system: 2015, version 2[J]. Eur Urol, 2016, 69 (1): 16- 40.
doi: 10.1016/j.eururo.2015.08.052 |
| 8 |
Borkowetz A , Platzek I , Toma M , et al. Direct comparison of multiparametric magnetic resonance imaging (MRI) results with final histopathology in patients with proven prostate cancer in MRI/ultrasonography-fusion biopsy[J]. BJU Int, 2016, 118 (2): 213- 220.
doi: 10.1111/bju.13461 |
| 9 |
Cash H , Maxeiner A , Stephan C , et al. The detection of significant prostate cancer is correlated with the prostate imaging reporting and data system (PI-RADS) in MRI/transrectal ultrasound fusion biopsy[J]. World J Urol, 2016, 34 (4): 525- 532.
doi: 10.1007/s00345-015-1671-8 |
| 10 |
Kasivisvanathan V , Rannikko AS , Borghi M , et al. MRI-targeted or standard biopsy for prostate-cancer diagnosis[J]. N Engl J Med, 2018, 378 (19): 1767- 1777.
doi: 10.1056/NEJMoa1801993 |
| 11 |
Radtke JP , Schwab C , Wolf MB , et al. Multiparametric magnetic resonance imaging (MRI) and MRI-transrectal ultrasound fusion biopsy for index tumor detection: correlation with radical prostatectomy specimen[J]. Eur Urol, 2016, 70 (5): 846- 853.
doi: 10.1016/j.eururo.2015.12.052 |
| 12 |
Turkbey B , Mani H , Aras O , et al. Correlation of magnetic resonance imaging tumor volume with histopathology[J]. J Urol, 2012, 188 (4): 1157- 1163.
doi: 10.1016/j.juro.2012.06.011 |
| 13 |
Nelson BA , Shappell SB , Chang SS , et al. Tumour volume is an independent predictor of prostate-specific antigen recurrence in patients undergoing radical prostatectomy for clinically localized prostate cancer[J]. BJU Int, 2006, 97 (6): 1169- 1172.
doi: 10.1111/j.1464-410X.2006.06148.x |
| 14 |
Ploussard G , Beauval JB , Renard-Penna R , et al. Assessment of the minimal targeted biopsy core number per MRI lesion for improving prostate cancer grading prediction[J]. J Clin Med, 2020, 9 (1): 225.
doi: 10.3390/jcm9010225 |
| 15 |
Rais-Bahrami S , Türkbey B , Rastinehad AR , et al. Natural history of small index lesions suspicious for prostate cancer on multiparametric MRI: Recommendations for interval imaging follow-up[J]. Diagn Interv Radiol, 2014, 20 (4): 293- 298.
doi: 10.5152/dir.2014.13319 |
| 16 |
Wolters T , Roobol MJ , van Leeuwen PJ , et al. A critical analysis of the tumor volume threshold for clinically insignificant prostate cancer using a data set of a randomized screening trial[J]. J Urol, 2011, 185 (1): 121- 125.
doi: 10.1016/j.juro.2010.08.082 |
| 17 |
Johnson DC , Raman SS , Mirak SA , et al. Detection of individual prostate cancer foci via multiparametric magnetic resonance imaging[J]. Eur Urol, 2019, 75 (5): 712- 720.
doi: 10.1016/j.eururo.2018.11.031 |
| 18 |
Matoso A , Epstein JI . Defining clinically significant prostate cancer on the basis of pathological findings[J]. Histopathology, 2019, 74 (1): 135- 145.
doi: 10.1111/his.13712 |
| 19 |
Mahjoub S , Baur ADJ , Lenk J , et al. Optimizing size thresholds for detection of clinically significant prostate cancer on MRI: Peripheral zone cancers are smaller and more predictable than transition zone tumors[J]. Eur J Radiol, 2020, 129, 109071.
doi: 10.1016/j.ejrad.2020.109071 |
| 20 |
Sakala MD , Dyer RB , Tappouni R . The "erased charcoal" sign[J]. Abdom Radiol (NY), 2017, 42 (3): 981- 982.
doi: 10.1007/s00261-016-0938-x |
| 21 |
Alanee S , Deebajah M , Dabaja A , et al. Utilizing lesion diameter and prostate specific antigen density to decide on magnetic resonance imaging guided confirmatory biopsy of prostate imaging reporting and data system score three lesions in African American prostate cancer patients managed with active surveillance[J]. Int Urol Nephrol, 2022, 54 (4): 799- 803.
doi: 10.1007/s11255-022-03136-1 |
| 22 |
Kilic M , Madendere S , Vural M , et al. The role of the size and number of index lesion in the diagnosis of clinically significant prostate cancer in patients with PI-RADS 4 lesions who underwent in-bore MRI-guided prostate biopsy[J]. World J Urol, 2023, 41 (2): 449- 454.
doi: 10.1007/s00345-022-04274-y |
| 23 |
Park MY , Park KJ , Lim B , et al. Comparison of biopsy strategies for prostate biopsy according to lesion size and PSA density in MRI-directed biopsy pathway[J]. Abdom Radiol (NY), 2020, 45 (12): 4166- 4177.
doi: 10.1007/s00261-020-02667-4 |
| 24 | Senel S , Koudonas A , Uzun E , et al. The value of prostate-specific antigen density in combination with lesion diameter for the accuracy of prostate cancer prediction in prostate imaging-reporting and data system 3 prostate lesions[J]. Urol Int, 2023, 107 (10/11/12): 965- 970. |
| 25 |
Costa DN , Goldberg K , Leon AD , et al. Magnetic resonance imaging-guided in-bore and magnetic resonance imaging-transrectal ultrasound fusion targeted prostate biopsies: An adjusted comparison of clinically significant prostate cancer detection rate[J]. Eur Urol Oncol, 2019, 2 (4): 397- 404.
doi: 10.1016/j.euo.2018.08.022 |
| 26 |
Schoots IG , Padhani AR , Rouvière O , et al. Analysis of magnetic resonance imaging-directed biopsy strategies for changing the paradigm of prostate cancer diagnosis[J]. Eur Urol Oncol, 2020, 3 (1): 32- 41.
doi: 10.1016/j.euo.2019.10.001 |
| [1] | 李志存, 吴天俣, 梁磊, 范宇, 孟一森, 张骞. 穿刺活检单针阳性前列腺癌术后病理升级的危险因素分析及列线图模型构建[J]. 北京大学学报(医学版), 2024, 56(5): 896-901. |
| [2] | 邢念增,王明帅,杨飞亚,尹路,韩苏军. 前列腺免活检创新理念的临床实践及其应用前景[J]. 北京大学学报(医学版), 2024, 56(4): 565-566. |
| [3] | 姚凯烽,阮明健,李德润,田宇轩,陈宇珂,范宇,刘毅. 靶向穿刺联合区域系统穿刺对PI-RADS 4~5分患者的前列腺癌诊断效能[J]. 北京大学学报(医学版), 2024, 56(4): 575-581. |
| [4] | 欧俊永,倪坤明,马潞林,王国良,颜野,杨斌,李庚午,宋昊东,陆敏,叶剑飞,张树栋. 肌层浸润性膀胱癌合并中高危前列腺癌患者的预后因素[J]. 北京大学学报(医学版), 2024, 56(4): 582-588. |
| [5] | 薛蔚,董樑,钱宏阳,费笑晨. 前列腺癌新辅助治疗与辅助治疗的现状及进展[J]. 北京大学学报(医学版), 2023, 55(5): 775-780. |
| [6] | 刘毅,袁昌巍,吴静云,沈棋,肖江喜,赵峥,王霄英,李学松,何志嵩,周利群. 靶向穿刺+6针系统穿刺对PI-RADS 5分患者的前列腺癌诊断效能[J]. 北京大学学报(医学版), 2023, 55(5): 812-817. |
| [7] | 毛海,张帆,张展奕,颜野,郝一昌,黄毅,马潞林,褚红玲,张树栋. 基于MRI前列腺腺体相关参数构建腹腔镜前列腺癌术后尿失禁的预测模型[J]. 北京大学学报(医学版), 2023, 55(5): 818-824. |
| [8] | 袁昌巍,李德润,李志华,刘毅,山刚志,李学松,周利群. 多参数磁共振成像中动态对比增强状态在诊断PI-RADS 4分前列腺癌中的应用[J]. 北京大学学报(医学版), 2023, 55(5): 838-842. |
| [9] | 田聪,刘军,杨波,乔佳佳,黄晓波,许清泉. 经皮肾镜取石术中异常肾盂黏膜活检结果分析[J]. 北京大学学报(医学版), 2023, 55(5): 948-952. |
| [10] | 郑丹枫,李君禹,李佳曦,张英爽,钟延丰,于淼. 青少年特发性脊柱侧凸椎旁肌的病理特征[J]. 北京大学学报(医学版), 2023, 55(2): 283-291. |
| [11] | 刘毅,刘志坚,沈棋,吴静云,范宇,李德润,虞巍,何志嵩. 14例恶性潜能未定的前列腺间质肿瘤病例分析[J]. 北京大学学报(医学版), 2020, 52(4): 621-624. |
| [12] | 郝一昌,颜野,张帆,邱敏,周朗,刘可,卢剑,肖春雷,黄毅,刘承,马潞林. 穿刺活检单针阳性的前列腺癌手术策略选择及经验总结[J]. 北京大学学报(医学版), 2020, 52(4): 625-631. |
| [13] | 颜野,夏海缀,李旭升,何为,朱学华,张智荧,肖春雷,刘余庆,黄华,何良华,卢剑. 基于U型卷积神经网络学习的前列腺癌影像重建模型在手术导航中的应用[J]. 北京大学学报(医学版), 2019, 51(3): 596-601. |
| [14] | 张帆,肖春雷,张树栋,黄毅,马潞林. 前列腺体积及前列腺突入膀胱长度与腹腔镜前列腺癌根治术后控尿功能恢复的相关性[J]. 北京大学学报(医学版), 2018, 50(4): 621-625. |
| [15] | 毕永祥,肖民辉,张宁南,李晓云,毛晓鹏,张科,章卓睿,赵良运. 小鼠不同部位体内前列腺癌骨转移模型的建立及方法改进[J]. 北京大学学报(医学版), 2017, 49(4): 590-596. |
|
||