Journal of Peking University(Health Sciences) ›› 2020, Vol. 52 ›› Issue (1): 58-63. doi: 10.19723/j.issn.1671-167X.2020.01.009
Previous Articles Next Articles
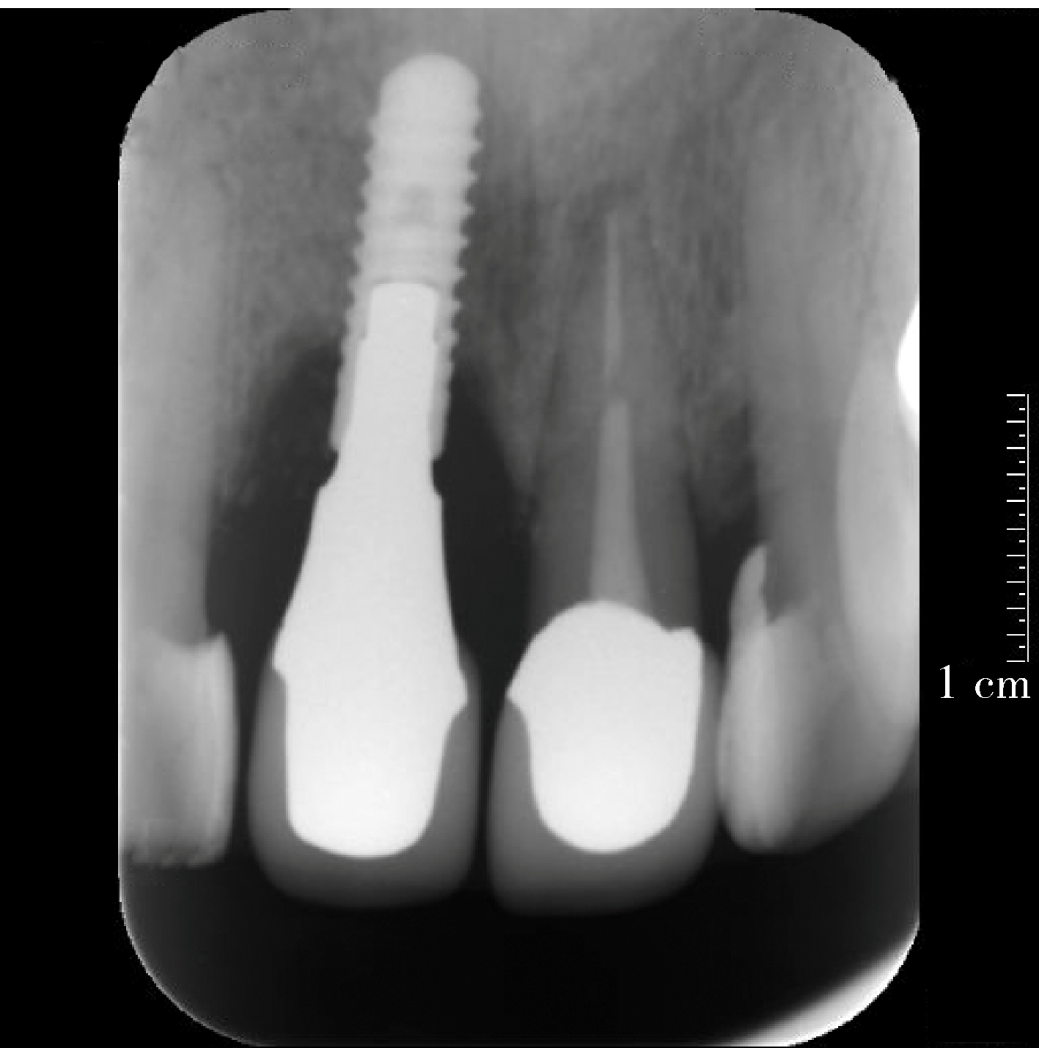
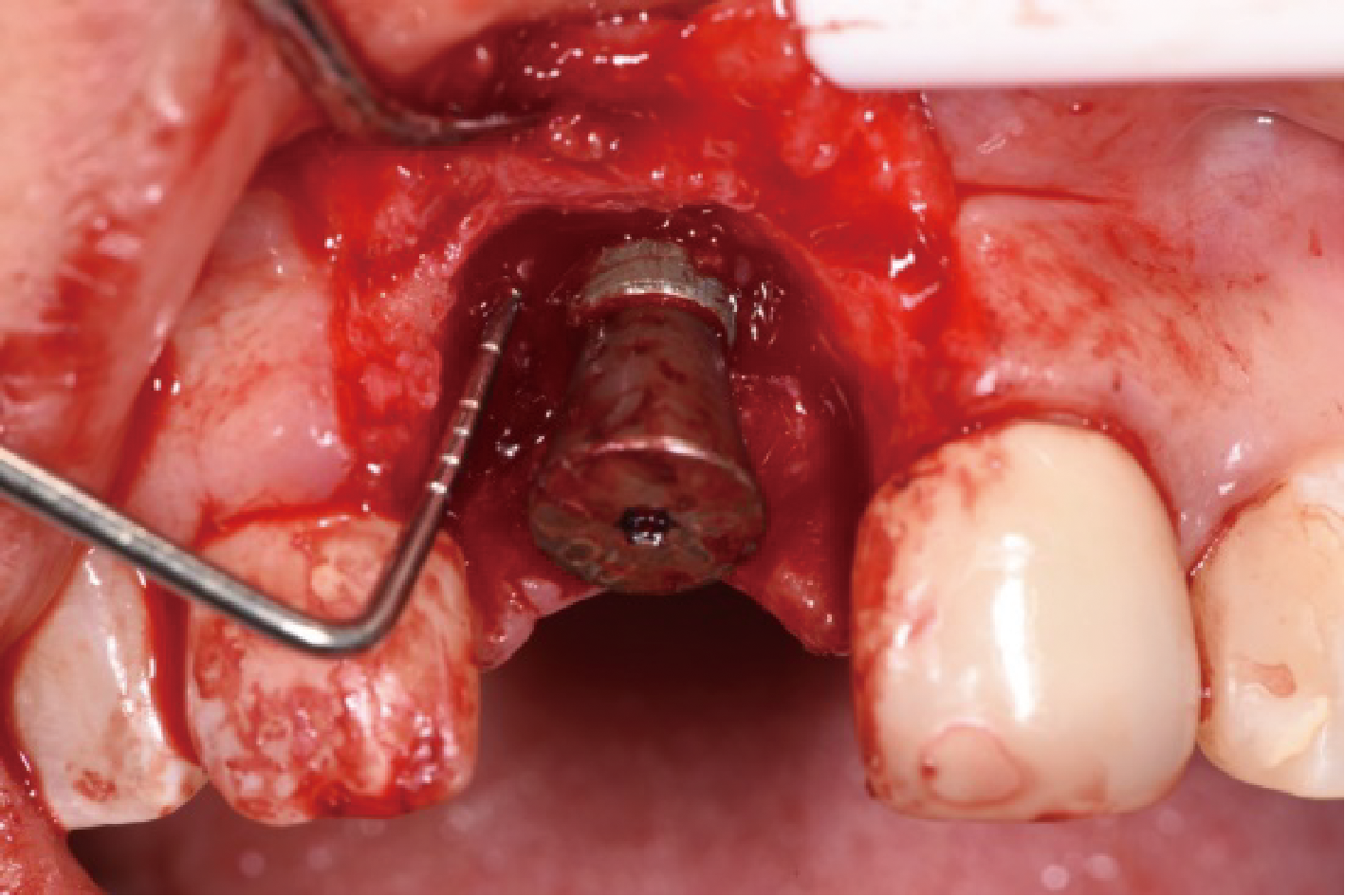
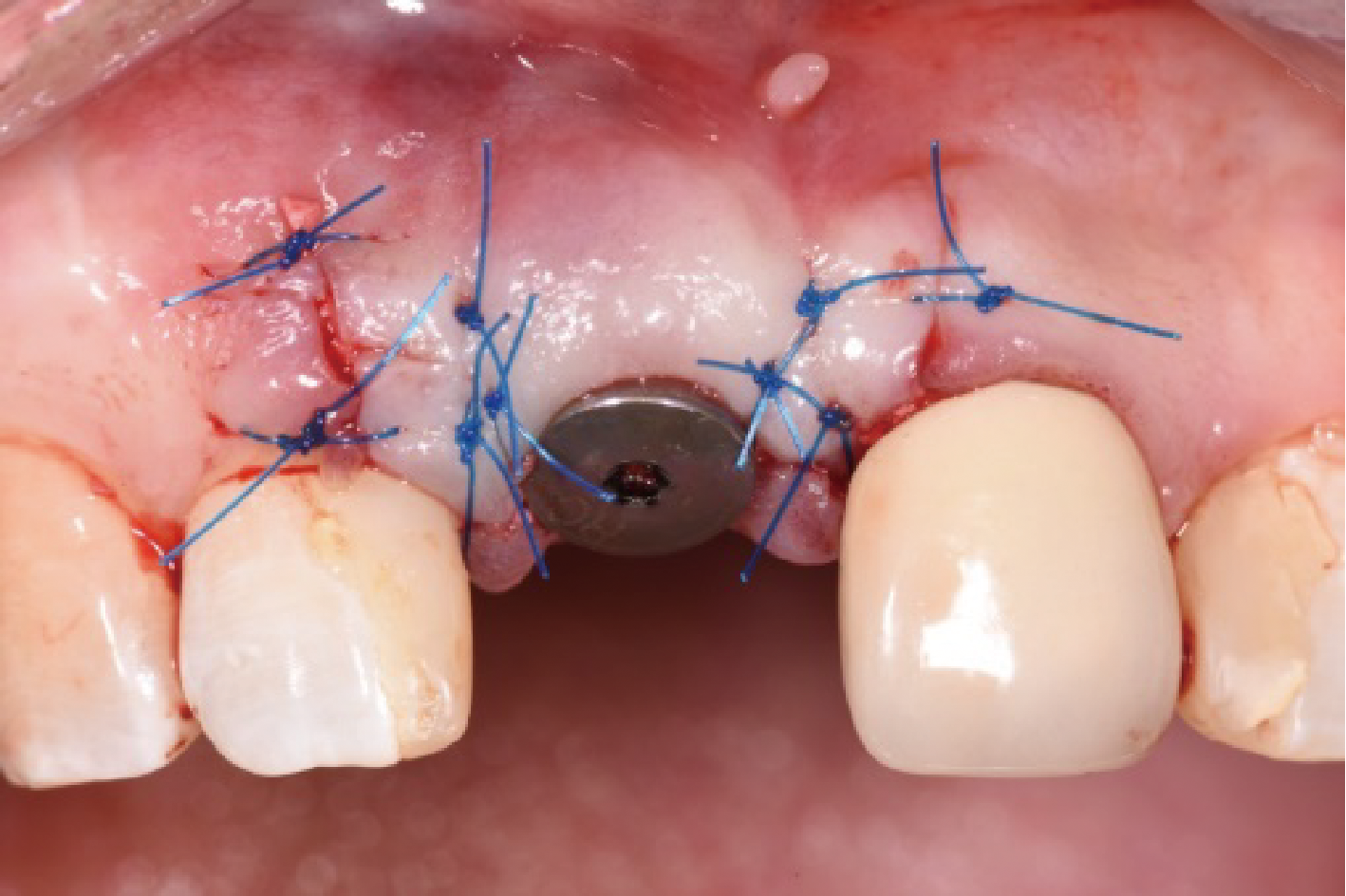
Short-term outcome of regenerative surgery treating peri-implantitis
Dong SHI,Jie CAO,Shi-ai DAI,Huan-xin MENG( )
)
- Department of Periodontology, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
CLC Number:
- R781.4
| [1] | Berglundh T, Armitage G, Araujo MG , et al. Peri-implant diseases and conditions: Consensus report of workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions[J]. J Periodontol, 2018,89(Suppl 1):313-318. |
| [2] | Khoury F, Keeve PL, Ramanauskaite A , et al. Surgical treatment of peri-implantitis: Consensus report of working group 4[J]. Int Dent J, 2019,69(Suppl 2):18-22. |
| [3] | Tomasi C, Regidor E, Ortiz-Vigón A , et al. Efficacy of reconstructive surgical therapy at peri-implantitis related bone defects. A systematic review and meta-analysis[J]. J Clin Periodontol, 2019,46(Supppl 21):340-356. |
| [4] | Clem D, Gunsolley JC . Peri-implantitis treatment using Er:YAG laser and bone grafting. A prospective consecutive case series evaluation: 1 year post therapy[J]. Int J Periodontics Restorative Dent, 2019,39(4):479-489. |
| [5] | de Tapia B, Valles C, Ribeiro-Amaral T , et al. The adjunctive effect of a titanium brush in implant surface decontamination at peri-implantitis surgical regenerative interventions: A randomized controlled clinical trial[J]. J Clin Periodontol, 2019,46(5):586-596. |
| [6] | 释栋 . 种植体周围炎再生治疗五年观察一例[J]. 中华口腔医学杂志, 2018,53(4):271-274. |
| [7] | Schwarz F, Herten M, Sager M , et al. Comparison of naturally occurring and ligature-induced peri-implantiti bone defects in humans and dogs[J]. Clin Oral Impl Res, 2007,18(2):167-170. |
| [8] | Renvert S, Persson GR, Pirih FQ , et al. Peri-implant health, peri-implant mucositis, and peri-implantitis: Case definitions and diagnostic considerations[J]. J Periodonto, 2018,89(Suppl 1):304-312. |
| [9] | Roos-Jansåker AM, Renvert H, Lindahl C , et al. Surgical treatment of peri-implantitis using a bone substitute with or without a resorbable membrane: A prospective cohort study[J]. J Clin Periodontol, 2007,34:625-632. |
| [10] | Hämmerle CH, Fourmousis I, Winkler JR , et al. Successful bone fill in late peri-implant defects using guided tissue regeneration. A short communication[J]. J Periodontol, 1995,66(4):303-308. |
| [11] | Almohandes A, Carcuac O, Abrahamsson I , et al. Re-osseointegration following reconstructive surgical therapy of experimental peri-implantitis. A pre-clinical in vivo study[J]. Clin Oral Impl Res, 2019,30(5):447-456. |
| [12] | Roos-Jansåker AM, Renvert H, Lindahl C , et al. Submerged healing following surgical treatment of peri-implantitis: A case series[J]. J Clin Periodontol, 2007,34:723-727. |
| [13] | Schwarz F, Sahm N, Schwarz K , et al. Impact of defect configuration on the clinical outcome following surgical regenerative therapy of peri-implantitis[J]. J Clin Periodontol, 2010,37(5):449-455. |
| [14] | Schwarz F, Sahm N, Becker J . Combined surgical therapy of advanced peri-implantitis lesions with concomitant soft tissue volume augmentation. A case series[J]. Clin Oral Implants Res, 2014,25(1):132-136. |
| [15] | Aghazadeh A, Rutger PG, Renvert S . A single-centre randomized controlled clinical trial on the adjunt treatment of intra-bony defects with autogenous bone or a xenograft: Results after 12 months[J]. J Clin Periodontol, 2012,39(7):666-673. |
| [16] | Roccuzzo M, Pittoni D, Roccuzzo A , et al. Surgical treatment of peri-implantitis intrabony lesions by means of deproteinized bovine bone mineral with 10% collagen: 7-year-results[J]. Clin Oral Implants Res, 2017,28(12):1577-1583. |
| [1] | Han ZHANG,Yixuan QIN,Diyuan WEI,Jie HAN. A preliminary study on compliance of supportive treatment of patients with periodontitis after implant restoration therapy [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 39-44. |
| [2] | Han ZHAO,Yan WEI,Xuehui ZHANG,Xiaoping YANG,Qing CAI,Chengyun NING,Mingming XU,Wenwen LIU,Ying HUANG,Ying HE,Yaru GUO,Shengjie JIANG,Yunyang BAI,Yujia WU,Yusi GUO,Xiaona ZHENG,Wenjing LI,Xuliang DENG. Bionic design, preparation and clinical translation of oral hard tissue restorative materials [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 4-8. |
| [3] | Congwei WANG,Min GAO,Yao YU,Wenbo ZHANG,Xin PENG. Clinical analysis of denture rehabilitation after mandibular fibula free-flap reconstruction [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 66-73. |
| [4] | Sui LI,Wenjie MA,Shimin WANG,Qian DING,Yao SUN,Lei ZHANG. Trueness of different digital design methods for incisal guidance of maxillary anterior implant-supported single crowns [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 81-87. |
| [5] | Xiaoqiang LIU,Yin ZHOU. Risk factors of perioperative hypertension in dental implant surgeries with bone augmentation [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 93-98. |
| [6] | Qian DING,Wen-jin LI,Feng-bo SUN,Jing-hua GU,Yuan-hua LIN,Lei ZHANG. Effects of surface treatment on the phase and fracture strength of yttria- and magnesia-stabilized zirconia implants [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 721-728. |
| [7] | Meng-en OU,Yun DING,Wei-feng TANG,Yong-sheng ZHOU. Three-dimensional finite element analysis of cement flow in abutment margin-crown platform switching [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 548-552. |
| [8] | Ling-wei MENG,Xue LI,Sheng-han GAO,Yue LI,Rui-tao CAO,Yi ZHANG,Shao-xia PAN. Comparison of three methods for establishing rat peri-implantitis model [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 22-29. |
| [9] | Fei SUN,Jian LIU,Si-qi LI,Yi-ping WEI,Wen-jie HU,Cui WANG. Profiles and differences of submucosal microbial in peri-implantitis and health implants: A cross-sectional study [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 30-37. |
| [10] | Fei SUN,Si-qi LI,Yi-ping WEI,Jin-sheng ZHONG,Cui WANG,Wen-jie HU. Efficacy of combined application of glycine powder air-polishing in non-surgical treatment of peri-implant diseases [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 119-125. |
| [11] | LI Yi,YU Hua-jie,QIU Li-xin. Clinical classification and treatment decision of implant fracture [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 126-133. |
| [12] | WANG Juan,YU Hua-jie,SUN Jing-de,QIU Li-xin. Application evaluation of prefabricated rigid connecting bar in implants immediate impression preparation of edentulous jaw [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 187-192. |
| [13] | Feng LIANG,Min-jie WU,Li-dong ZOU. Clinical observation of the curative effect after 5-year follow-up of single tooth implant-supported restorations in the posterior region [J]. Journal of Peking University (Health Sciences), 2021, 53(5): 970-976. |
| [14] | YOU Peng-yue,LIU Yu-hua,WANG Xin-zhi,WANG Si-wen,TANG Lin. Biocompatibility and effect on bone formation of a native acellular porcine pericardium: Results of in vitro and in vivo [J]. Journal of Peking University (Health Sciences), 2021, 53(4): 776-784. |
| [15] | WANG Si-wen,YOU Peng-yue,LIU Yu-hua,WANG Xin-zhi,TANG Lin,WANG Mei. Efficacy of two barrier membranes and deproteinized bovine bone mineral on bone regeneration in extraction sockets: A microcomputed tomographic study in dogs [J]. Journal of Peking University (Health Sciences), 2021, 53(2): 364-370. |
| Viewed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
Full text 533
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
|
Abstract 1136
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||
Cited |
|
|||||||||||||||||||||||||||||||||||||||||||||||||
| Shared | ||||||||||||||||||||||||||||||||||||||||||||||||||
| Discussed | ||||||||||||||||||||||||||||||||||||||||||||||||||
|
||