Journal of Peking University (Health Sciences) ›› 2026, Vol. 58 ›› Issue (1): 74-83. doi: 10.19723/j.issn.1671-167X.2026.01.010
Previous Articles Next Articles
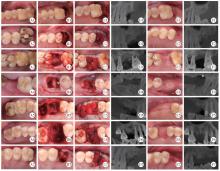
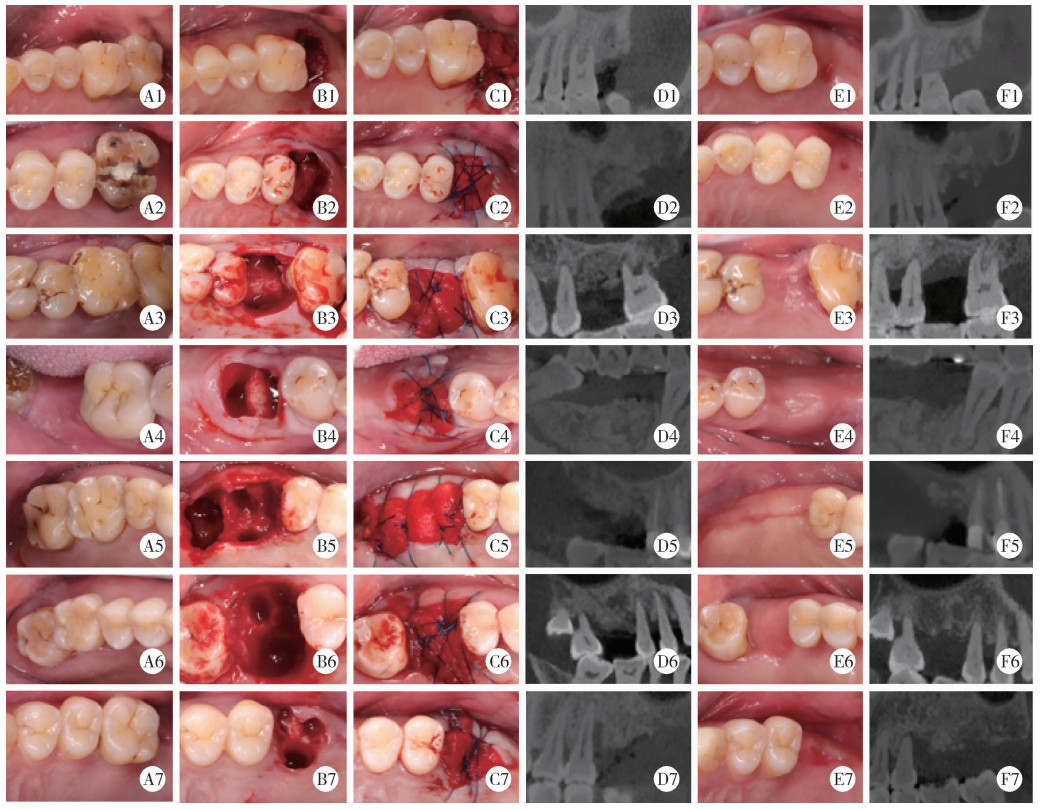
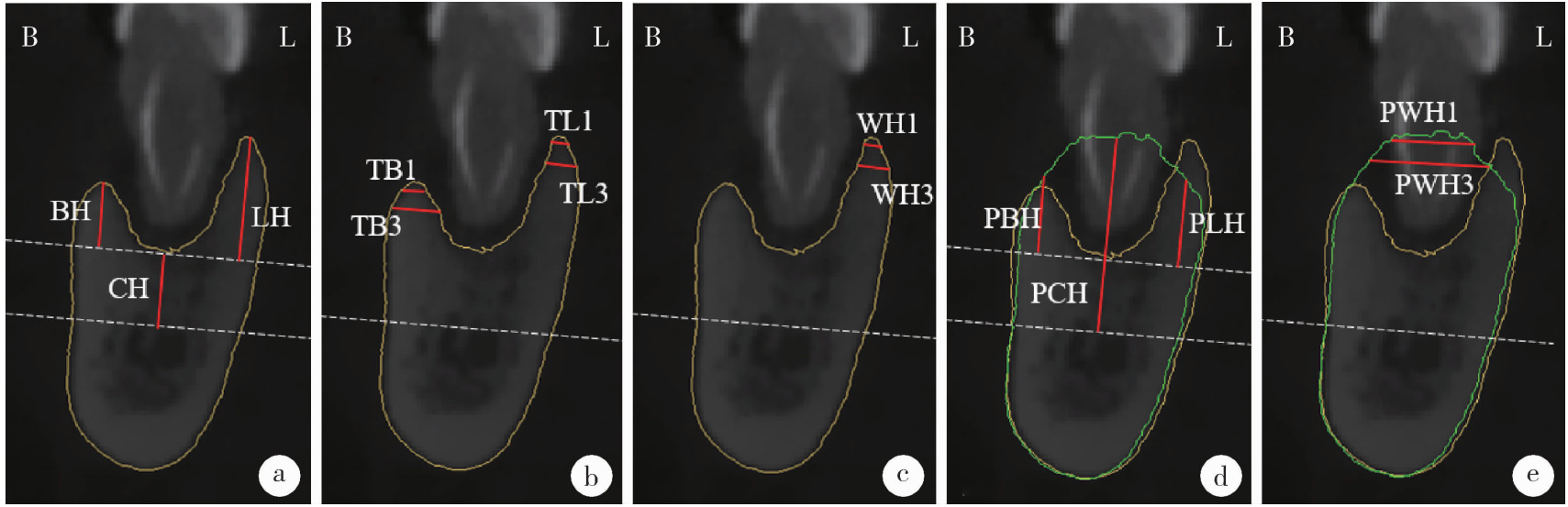
Clinical comparison of xenograft versus synthetic bone graft materials in micro crestal flap-alveolar ridge preservation following extraction of molars
Siqiao ZHANG1, Jian LIU1, Tao XU2,*( ), Wenjie HU1,*(
), Wenjie HU1,*( ), Haoyun ZHANG1, Yiping WEI1
), Haoyun ZHANG1, Yiping WEI1
- 1. Department of Periodontology, Peking University School and Hospital of Stomatology & National Center for Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Research Center of Oral Biomaterials and Digital Medical Devices & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
2. Department of Oral Emergency, Peking University School and Hospital of Stomatology & National Center for Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Research Center of Oral Biomaterials and Digital Medical Devices & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
CLC Number:
- R782.1
| 1 |
doi: 10.1111/clr.13975 |
| 2 |
doi: 10.1111/cid.12585 |
| 3 |
|
| 4 |
doi: 10.11607/jomi.6399 |
| 5 |
doi: 10.1111/j.1600-0501.2009.01891.x |
| 6 |
|
| 7 |
doi: 10.1111/jcpe.13231 |
| 8 |
doi: 10.1111/clr.13436 |
| 9 |
doi: 10.1007/s00784-021-04204-z |
| 10 |
|
| 11 |
doi: 10.1111/clr.12911 |
| 12 |
doi: 10.1002/JPER.19-0211 |
| 13 |
doi: 10.1111/prd.12469 |
| 14 |
doi: 10.1111/jcpe.14045 |
| 15 |
赵丽萍, 詹雅琳, 胡文杰, 等. 不同测量方法评价磨牙拔牙位点保存术后牙槽骨的变化[J]. 北京大学学报(医学版), 2016, 48 (1): 126- 132.
doi: 10.3969/j.issn.1671-167X.2016.01.023 |
| 16 |
赵丽萍, 胡文杰, 徐涛, 等. 罹患重度牙周病变磨牙拔牙后两种牙槽嵴保存方法的比较[J]. 北京大学学报(医学版), 2019, 51 (3): 579- 585.
doi: 10.19723/j.issn.1671-167X.2019.03.030 |
| 17 |
doi: 10.1111/clr.14204 |
| 18 |
|
| 19 |
|
| 20 |
doi: 10.1111/clr.12170 |
| 21 |
doi: 10.1111/clr.12712 |
| 22 |
|
| 23 |
doi: 10.1186/s40729-021-00305-2 |
| 24 |
doi: 10.11607/prd.4444 |
| 25 |
doi: 10.1016/j.jdent.2022.104323 |
| 26 |
|
| 27 |
朱磊, 刘庆成, 于洪波. 牙槽骨增量骨皮质切开术后2种植骨材料成骨的影像学分析[J]. 中国口腔颌面外科杂志, 2021, 19 (6): 525- 530.
|
| 28 |
doi: 10.1186/s12903-024-04803-8 |
| 29 |
|
| 30 |
doi: 10.1016/j.jds.2021.05.003 |
| 31 |
doi: 10.1111/j.1600-0501.2010.01918.x |
| 32 |
doi: 10.1007/s00784-025-06272-x |
| 33 |
doi: 10.11607/prd.0734 |
| 34 |
doi: 10.1111/jcpe.12027 |
| 35 |
|
| 36 |
doi: 10.1111/clr.13594 |
| 37 |
doi: 10.1186/s40902-021-00328-0 |
| [1] | Lianfei PAN, Wenjing LI, Ruiyang WANG, Jian JIAO, Zhanqiang CAO, Li GAO, Dong SHI. Short-term efficacy and influencing factors of systemic antibiotics as an adjunct to mechanical periodontal therapy for stages Ⅲ/Ⅳ periodontitis [J]. Journal of Peking University (Health Sciences), 2026, 58(1): 30-36. |
| [2] | Rentao TANG, Liuchang YANG, Jie NIE, Xiaoyan WANG. Microbial communities in extraradicular infections of post-treatment apical periodontitis without or with sinus tracts [J]. Journal of Peking University (Health Sciences), 2026, 58(1): 43-49. |
| [3] | Baojin MA, Jianhua LI, Yuanhua SANG, Yang YU, Jichuan QIU, Jinlong SHAO, Kai LI, Shiyue LIU, Mi DU, Lingling SHANG, Shaohua GE. Establishment and application of key technologies for periodontal tissue regeneration based on microenvironment and stem cell regulation [J]. Journal of Peking University (Health Sciences), 2025, 57(5): 841-846. |
| [4] | Pei CAO, Qingxian LUAN. Periodontitis and systemic diseases: Thinking and explorations [J]. Journal of Peking University (Health Sciences), 2025, 57(5): 852-858. |
| [5] | Zhenying BAO, Yajie WANG. Application of combined detection of inflammatory indexes and cytokines in chronic periodontitis [J]. Journal of Peking University (Health Sciences), 2025, 57(4): 772-778. |
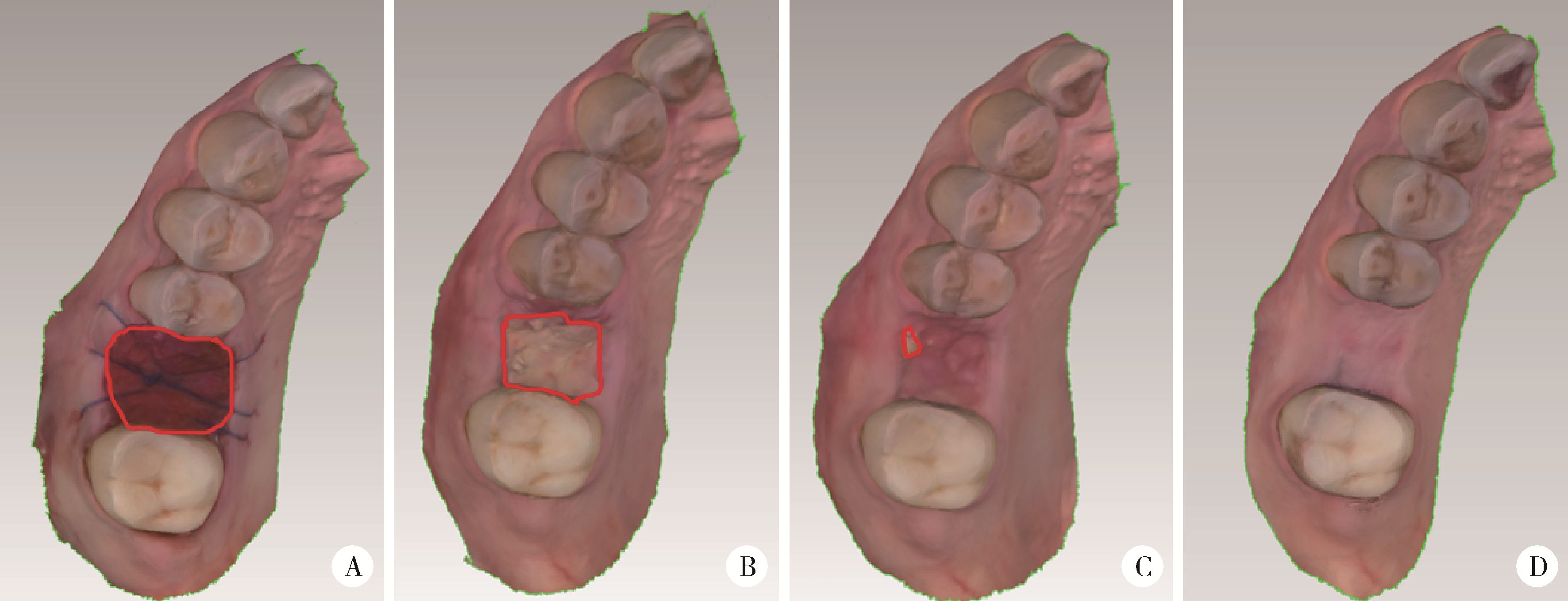
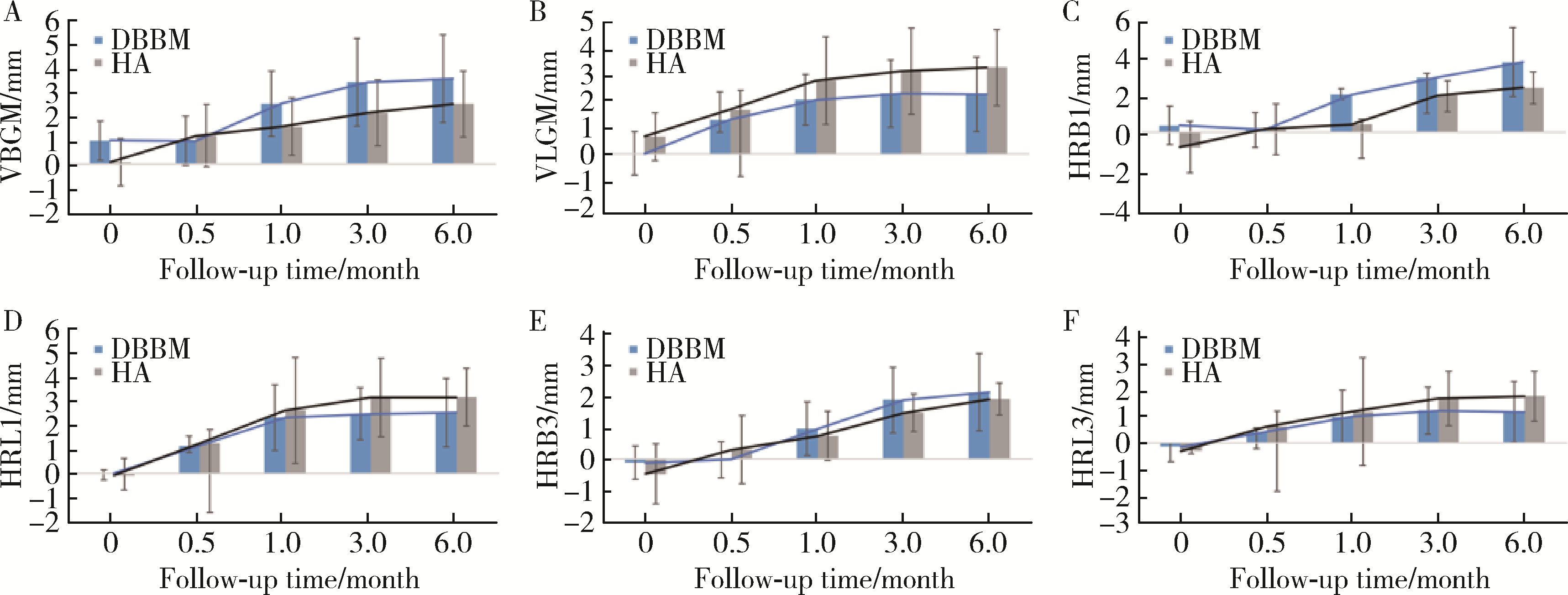
| [6] | Yutong SHI, Yiping WEI, Wenjie HU, Tao XU, Haoyun ZHANG. Evaluation of micro crestal flap-alveolar ridge preservation following extraction of mandibular molars with severe periodontitis [J]. Journal of Peking University (Health Sciences), 2025, 57(1): 33-41. |
| [7] | Jingqian LI, Zilu ZHU, Jian JIAO, Jie SHI. Clinical efficacy of clear aligner treatment for pathologically migrated teeth in the anterior region of patients with severe periodontitis [J]. Journal of Peking University (Health Sciences), 2025, 57(1): 51-56. |
| [8] | Yuru HU,Juan LIU,Wenjing LI,Yibing ZHAO,Qiqiang LI,Ruifang LU,Huanxin MENG. Relationship between short-chain fatty acids in the gingival crevicular fluid and periodontitis of stage Ⅲ or Ⅳ [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 332-337. |
| [9] | Han ZHANG,Yixuan QIN,Diyuan WEI,Jie HAN. A preliminary study on compliance of supportive treatment of patients with periodontitis after implant restoration therapy [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 39-44. |
| [10] | Chang SHU,Ye HAN,Yuzhe SUN,Zaimu YANG,Jianxia HOU. Changes of parameters associated with anemia of inflammation in patients with stage Ⅲ periodontitis before and after periodontal initial therapy [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 45-50. |
| [11] | Xi-yan PEI,Wen YANG,Xiang-ying OUYANG,Feng SUN. Comparison of clinical effects between periodontal endoscopy aiding subgingival debridement and flap surgery [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 716-720. |
| [12] | Jing WEN,Xiang-ying OUYANG,Xi-yan PEI,Shan-yong QIU,Jian-ru LIU,Wen-yi LIU,Cai-fang CAO. Multivariable analysis of tooth loss in subjects with severe periodontitis over 4-year natural progression [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 70-77. |
| [13] | ZHU Xiao-ling,LI Wen-jing,WANG Xian-e,SONG Wen-li,XU Li,ZHANG Li,FENG Xiang-hui,LU Rui-fang,SHI Dong,MENG Huan-xin. Gene polymorphisms of cytochrome B-245 alpha chain (CYBA) and cholesteryl ester transfer protein (CETP) and susceptibility to generalized aggressive periodontitis [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 18-22. |
| [14] | XU Xin-ran,HUO Peng-cheng,HE Lu,MENG Huan-xin,ZHU Yun-xuan,JIN Dong-si-qi. Comparison of initial periodontal therapy and its correlation with white blood cell level in periodontitis patients with or without diabetes mellitus [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 48-53. |
| [15] | GAO Hong-yu,MENG Huan-xin,HOU Jian-xia,HUANG Bao-xin,LI Wei. Expression and distribution of calprotectin in healthy and inflamed periodontal tissues [J]. Journal of Peking University (Health Sciences), 2021, 53(4): 744-749. |
|
||