Journal of Peking University (Health Sciences) ›› 2021, Vol. 53 ›› Issue (5): 970-976. doi: 10.19723/j.issn.1671-167X.2021.05.027
Previous Articles Next Articles
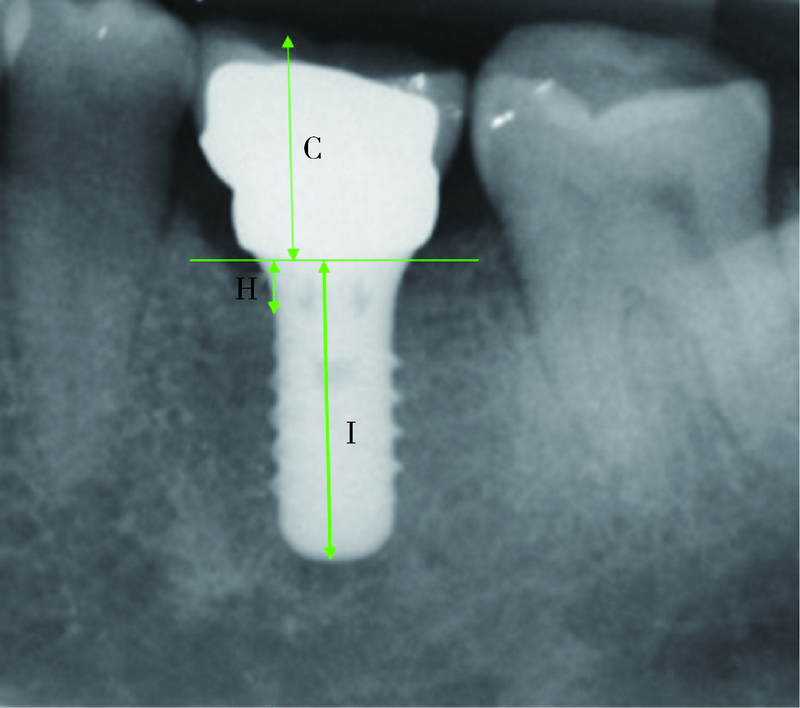
Clinical observation of the curative effect after 5-year follow-up of single tooth implant-supported restorations in the posterior region
LIANG Feng,WU Min-jie( ),ZOU Li-dong
),ZOU Li-dong
- Second Clinical Division, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100101, China
CLC Number:
- R783.6
| [1] |
Jung RE, Pjetrusson BE, Glauser R, et al. A systematic review of the 5-year survival and complication rates of implant-supported single crowns [J]. Clin Oral Implants Res, 2008, 19(2):119-130.
doi: 10.1111/clr.2008.19.issue-2 |
| [2] | Pjetursson BE, Thoma D, Jung R, et al. A systematic review of the survival and complication rates of implant-supported fixed dental prostheses (FDPs) after a mean observation period of at least 5 years [J]. Clin Oral Implants Res, 2012, 23(Suppl 6):22-38. |
| [3] | Zembic A, Kim S, Zwahlen M, et al. Systematic review of the survival rate and incidence of biologic, technical, and esthetic complications of single implant abutments supporting fixed prostheses [J]. Int J Oral Maxillofac Implants, 2014, 29(Suppl):99-116. |
| [4] | Hjalmarsson L, Gheisarifar M, Jemt T. A systematic review of survival of single implants as presented in longitudinal studies with a follow-up of at least 10 years [J]. I Eur J Oral Implantol, 2016, 9(Suppl 1):S155-162. |
| [5] | Garlini G, Chierichetti V, D’Amato S, et al. A long term follow-up of single-tooth Xive implant: 15 year results [J]. Dent Oral Craniofac Res, 2016, 3(1):1-4. |
| [6] |
Arunyanak SP, Pollini A, Ntounis A, et al. Clinician assessments and patient perspectives of single-tooth implant restorations in the esthetic zone of the maxilla: A systematic review [J]. J Prosthet Dent, 2017, 118(1):10-17.
doi: S0022-3913(16)30691-6 pmid: 28385430 |
| [7] |
Chrcanovic BR, Kisch J, Larsson C. Retrospective clinical evaluation of implant-supported single crowns: Mean follow-up of 15 years [J]. Clin Oral Implants Res, 2019, 30(7):691-701
doi: 10.1111/clr.2019.30.issue-7 |
| [8] | 林野, 李健慧, 邱立新, 等. 口腔种植修复临床效果十年回顾研究 [J]. 中华口腔医学杂志, 2006, 41(3):131-135. |
| [9] | 朱艳香, 程然, 林梓桐, 等. 上颌后牙区种植修复后6~9年临床疗效观察 [J]. 东南大学学报(医学版), 2017, 36(5):841-846. |
| [10] | 张燕婷, 李悦, 何晶, 等. 上颌后牙区不同术式种植修复10年累计存留率及患者相关因素对其成功率的影响分析 [J]. 中国实用口腔科杂志, 2017, 10(1):31-35. |
| [11] | Wheeler SL, Holmes RE, Calhoun CJ. Six-year clinical and histologic study of sinus-lift grafts [J]. Int J Oral Maxillofac Implants, 1996, 11(1):26-34. |
| [12] |
Renouard F, Nisand D. Impact of implant length and diameter on survival rates [J]. Clin Oral Implants Res, 2006, 17(Suppl 2):35-51.
doi: 10.1111/clr.2006.17.issue-s2 |
| [13] |
Zimmermann J, Sommer M, Grize L, et al. Marginal bone loss 1 year after implantation: a systematic review for fixed and removable restorations [J]. Clin Cosmet Investig Dent, 2019, 11:195-218.
doi: 10.2147/CCIDE |
| [14] | Pellicer-Chover H, Díaz-Sanchez M, Soto-Penaloza D, et al. Impact of crestal and subcrestal implant placement upon changes in marginal peri-implant bone level: A systematic review [J]. Med Oral Patol Oral Cir Bucal, 2019, 24(5):673-683. |
| [15] | Galindo-Moreno P, León-Cano A, Ortega-Oller I, et al. Marginal bone loss as success criterion in implant dentistry: beyond 2 mm [J]. Clin Oral Implants Res, 2015, 26(4):28-34. |
| [1] | Han ZHANG,Yixuan QIN,Diyuan WEI,Jie HAN. A preliminary study on compliance of supportive treatment of patients with periodontitis after implant restoration therapy [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 39-44. |
| [2] | Congwei WANG,Min GAO,Yao YU,Wenbo ZHANG,Xin PENG. Clinical analysis of denture rehabilitation after mandibular fibula free-flap reconstruction [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 66-73. |
| [3] | Sui LI,Wenjie MA,Shimin WANG,Qian DING,Yao SUN,Lei ZHANG. Trueness of different digital design methods for incisal guidance of maxillary anterior implant-supported single crowns [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 81-87. |
| [4] | Xiaoqiang LIU,Yin ZHOU. Risk factors of perioperative hypertension in dental implant surgeries with bone augmentation [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 93-98. |
| [5] | Qian DING,Wen-jin LI,Feng-bo SUN,Jing-hua GU,Yuan-hua LIN,Lei ZHANG. Effects of surface treatment on the phase and fracture strength of yttria- and magnesia-stabilized zirconia implants [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 721-728. |
| [6] | Meng-en OU,Yun DING,Wei-feng TANG,Yong-sheng ZHOU. Three-dimensional finite element analysis of cement flow in abutment margin-crown platform switching [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 548-552. |
| [7] | Fei SUN,Jian LIU,Si-qi LI,Yi-ping WEI,Wen-jie HU,Cui WANG. Profiles and differences of submucosal microbial in peri-implantitis and health implants: A cross-sectional study [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 30-37. |
| [8] | MA Ke-nan,CHEN Hu,SHEN Yan-ru,ZHOU Yong-sheng,WANG Yong,SUN Yu-chun. Finite element analyses of retention of removable partial denture circumferential clasps manufactured by selective laser melting [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 105-112. |
| [9] | LI Yi,YU Hua-jie,QIU Li-xin. Clinical classification and treatment decision of implant fracture [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 126-133. |
| [10] | WANG Juan,YU Hua-jie,SUN Jing-de,QIU Li-xin. Application evaluation of prefabricated rigid connecting bar in implants immediate impression preparation of edentulous jaw [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 187-192. |
| [11] | SUN Yu-chun,GUO Yu-qing,CHEN Hu,DENG Ke-hui,LI Wei-wei. Independent innovation research, development and transformation of precise bionic repair technology for oral prosthesis [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 7-12. |
| [12] | LIU Xiao-qiang,YANG Yang,ZHOU Jian-feng,LIU Jian-zhang,TAN Jian-guo. Blood pressure and heart rate changes of 640 single dental implant surgeries [J]. Journal of Peking University (Health Sciences), 2021, 53(2): 390-395. |
| [13] | YUE Zhao-guo,ZHANG Hai-dong,YANG Jing-wen,HOU Jian-xia. Comparison of residual cement between CAD/CAM customized abutments and stock abutments via digital measurement in vitro [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 69-75. |
| [14] | LI Peng,PIAO Mu-zi,HU Hong-cheng,WANG Yong,ZHAO Yi-jiao,SHEN Xiao-jing. Radiography study on osteotome sinus floor elevation with placed implant simultaneously with no graft augmentation [J]. Journal of Peking University (Health Sciences), 2021, 53(1): 95-101. |
| [15] | Ke-yi HAO,Jia LUO,Ping DI,Hou-zuo GUO,Hui-dan SHEN,Yan-ping LIU,Yu ZHANG,Ye LIN. Validation of the digital integration technology for evaluating the nasolabial morphology variation after the cross-arch fixed restoration of maxillary implant-supported prostheses [J]. Journal of Peking University (Health Sciences), 2020, 52(5): 924-930. |
|
||