Journal of Peking University (Health Sciences) ›› 2021, Vol. 53 ›› Issue (6): 1094-1098. doi: 10.19723/j.issn.1671-167X.2021.06.015
Previous Articles Next Articles
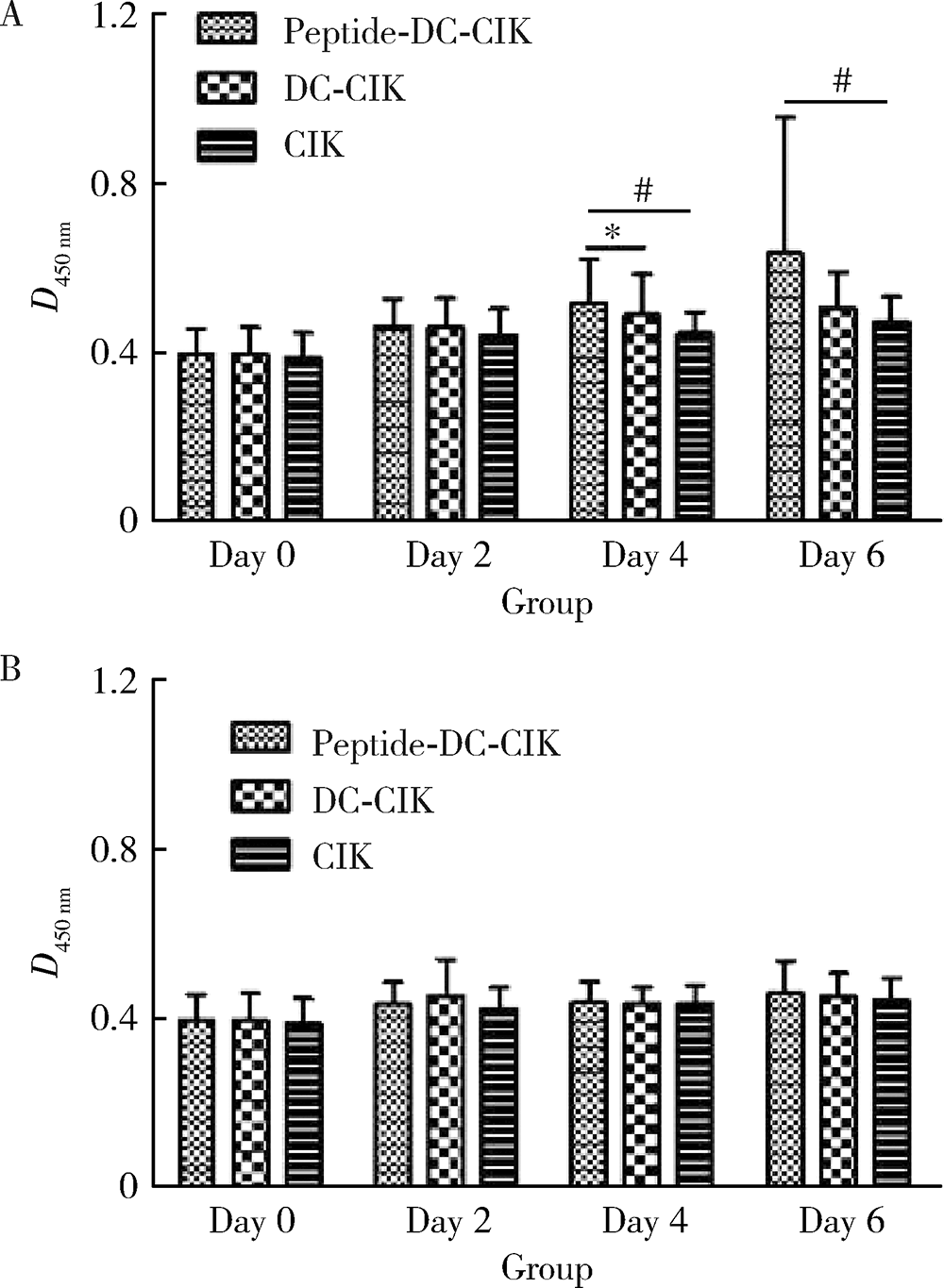
Assessment of lymphocytic function in vitro stimulated by specific tumor polypeptide combined with dendritic cells
YANG Duo1,ZHOU Xin-na1,WANG Shuo1,WANG Xiao-li1,YUAN Yan-hua1,YANG Hua-bin1,GENG Hui-zhen2,PENG Bing2,LI Zi-bo2,LI Bin2,REN Jun1,△( )
)
- 1. Department of Oncology, Beijing Shijitan Hospital, Capital Medical University Beijing Key Laboratory of Therapeutic Vaccines, Beijing 100038, China
2. Hebei Bio-High Technology Company Limited, Shijiazhuang 050035, China
CLC Number:
- R73-36+2
| [1] | 黄芸, 高建鹏, 王辉. 肿瘤疫苗临床研究评价及进展[J]. 肿瘤学杂志, 2019, 25(3):196-201. |
| [2] | 沈季敏, 刘欣. 基于树突状细胞的肿瘤免疫治疗临床应用方式的研究进展[J]. 临床血液学杂志, 2018, 31(1):62-65. |
| [3] | 邵小钧, 席庆. 精准医疗: 肿瘤诊治的新模式[J]. 现代肿瘤医学, 2016, 24(4):675-677. |
| [4] |
Jang GY, Kim YS, Lee SE, et al. Improvement of DC-based vaccines using adjuvant TLR4-binding 60S acidic ribosomal protein P2 and immune checkpoint inhibitors[J]. Cancer Immunol Immunother, 2021, 70(4):1075-1088.
doi: 10.1007/s00262-020-02759-6 |
| [5] |
Jiang N, Qiao G, Wang X, et al. Dendritic cell/cytokine-induced killer cell immunotherapy combined with s-1 in patients with advanced pancreatic cancer: A prospective study[J]. Clin Cancer Res, 2017, 23(17):5066-5073.
doi: 10.1158/1078-0432.CCR-17-0492 pmid: 28611200 |
| [6] | Calmeiro J, Carrascal MA, Tavares AR, et al. Pharmacological combination of nivolumab with dendritic cell vaccines in cancer immunotherapy: An overview[J/OL]. Pharmacol Res, 2021, 164: 105309[2021-01-01]. https://doi.org/10.1016/j.phrs.2020.105309. |
| [7] | Perez CR, De Palma M. Engineering dendritic cell vaccines to improve cancer immunotherapy[J/OL]. Nat Commun, 2019, 10(1): 5408[2021-01-01]. https://doi.org/10.1038/s41467-019-13368-y. |
| [8] | 黄聪, 白丽. 树突状细胞肿瘤疫苗及其联合应用的研究进展[J]. 细胞与分子免疫学杂志, 2019, 35(12):1141-1145. |
| [9] | Zhou JY, Alvarez CA, Cobb BA, Integration of IL-2 and IL-4 signals coordinates divergent regulatory T cell responses and drives therapeutic efficacy[J/OL]. Elife, 2021, 10: e57417(2021-02-22)[2021-03-01]. https://doi.org/10.7554/eLife.57417. |
| [10] | 于甜, 胡小鹏, 祝小红, 等. 干扰素及肿瘤坏死因子抗病毒作用研究进展[J]. 中国免疫学杂志, 2014, 30(3):409-415. |
| [11] | 马守宝, 林丹丹, 刘海燕. 炎症细胞因子在肿瘤微环境中的作用及其作为治疗靶点的研究进展[J]. 生命科学, 2016, 28(2):182-191. |
| [12] | 林雨虹, 吕合作, 吴俊英. GM-CSF/IL-3/IL-5的免疫调节作用[J]. 中国免疫学杂志, 2019, 35(4):500-504. |
| [13] | 姜南雁, 唐隽, 徐云升. GM-CSF在肿瘤免疫治疗中的作用最新研究进展[J]. 免疫学杂志, 2015, 31(8):717-722. |
| [14] | 吴晋楠, 陈建荣, 陈金亮, 等. 肺癌肿瘤微环境中白细胞介素的研究进展[J]. 临床肺科杂志, 2019, 24(12):2280-2283. |
| [15] | 李琬琼, 高艳锋. 抗肿瘤多肽药物研究进展[J]. 药学进展, 2019, 43(10):759-766. |
| [1] | Jiajun LIU, Guokang LIU, Yuhu ZHU. Immune-related severe pneumonia: A case report [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 932-937. |
| [2] | Yao ZHANG,Jinxin GUO,Shijia ZHAN,Enyu HONG,Hui YANG,Anna JIA,Yan CHANG,Yongli GUO,Xuan ZHANG. Role and mechanism of cysteine and glycine-rich protein 2 in the malignant progression of neuroblastoma [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 495-504. |
| [3] | Jing XIE,Yu-ming ZHAO,Nan-quan RAO,Xiao-tong WANG,Teng-jiao-zi FANG,Xiao-xia LI,Yue ZHAI,Jing-zhi LI,Li-hong GE,Yuan-yuan WANG. Comparative study of differentiation potential of mesenchymal stem cells derived from orofacial system into vascular endothelial cells [J]. Journal of Peking University(Health Sciences), 2019, 51(5): 900-906. |
| [4] | Fan ZHANG,Tai-qiang YAN,Wei GUO. Rasfonin inhibits proliferation and migration of osteosarcoma 143B cells [J]. Journal of Peking University(Health Sciences), 2019, 51(2): 234-238. |
| [5] | Jia-xing LIU,Gui-ping HU,Lin ZHAO,Yong-ming ZHANG,Li WANG,Guang JIA,Rui-xiang LIU,Hui-min FENG,Hua-dong XU. Early effects of low-level long-term occupational chromate exposure on workers’ health [J]. Journal of Peking University(Health Sciences), 2019, 51(2): 307-314. |
| [6] | WANG Zi-cheng, CHENG Li, LV Tong-de, SU Li, LIN Jian, ZHOU Li-qun. Inflammatory priming adipose derived stem cells significantly inhibit the proliferation of peripheral blood mononuclear cells [J]. Journal of Peking University(Health Sciences), 2018, 50(4): 590-594. |
| [7] | TANG Xu, ZHAO Wei-hong, SONG Qin-qin, YIN Hua-qi, DU Yi-qing, SHENG Zheng-zuo, WANG Qiang, ZHANG Xiao-wei, LI Qing, LIU Shi-jun, XU Tao. Influence of SOX10 on the proliferation and invasion of prostate cancer cells [J]. Journal of Peking University(Health Sciences), 2018, 50(4): 602-606. |
| [8] | WANG Xiao-tong, RAO Nan-quan, FANG Teng-jiao-zi, ZHAO Yu-ming, GE Li-hong. Comparison of the properties of CD146 positive and CD146 negative subpopulations of stem cells from human exfoliated deciduous teeth [J]. Journal of Peking University(Health Sciences), 2018, 50(2): 284-292. |
| [9] | CHEN Wei, HU Fan-lei, LIU Hong-jiang, XU Li-ling, LI Ying-ni, LI Zhan-guo. Myeloid-derived suppressor cells promoted autologous B cell proliferation in rheumatoid arthritis [J]. Journal of Peking University(Health Sciences), 2017, 49(5): 819-823. |
| [10] | CAI Yi, GUO Hao, LI Han-zhong, WANG Wen-da, ZHANG Yu-shi. MicroRNA differential expression profile in tuberous sclerosis complex cell line TSC2-/- MEFs and normal cell line TSC2+/+ MEFs [J]. Journal of Peking University(Health Sciences), 2017, 49(4): 580-584. |
| [11] | CAI Yuan-fa, ZHANG Hua-ming, NIU Wen-yi, ZOU Yong-qiu, MA De-fu. Effects of equol on colon cancer cell proliferation [J]. Journal of Peking University(Health Sciences), 2017, 49(3): 383-387. |
| [12] | YANG Di, XU Jun-hui, DENG Fu-rong△, GUO Xin-biao . Effects of silver nanoparticle on hemichannel activation and anti-proliferation in HaCaT cells [J]. Journal of Peking University(Health Sciences), 2017, 49(3): 371-375. |
| [13] | GAO Xiang, CHEN Xiang-mei, ZHANG Ting, ZHANG Jing, CHEN Mo, GUO Zheng--yang, SHI Yan-yan, LU Feng-min, DING Shi-gang. Relationship between macrophage capping protein and gastric cancer cell’s proliferation and migration ability [J]. Journal of Peking University(Health Sciences), 2017, 49(3): 489-494. |
| [14] | SIMA Zi-han, HONG Ying-ying, LI Tie-jun△. Effects of PTCH1 mutations on the epithelial proliferation derived from keratocystic odontogenic tumour [J]. Journal of Peking University(Health Sciences), 2017, 49(3): 522-526. |
| [15] | SUI Hua-xin, LV Pei-jun, WANG Yu-guang, WANG Yong, SUN Yu-chun. Effect of lowlevel laser irradiation on proliferation and osteogenic differentiation of human adipose-derived stromal cells [J]. Journal of Peking University(Health Sciences), 2017, 49(2): 337-343. |
|
||