Journal of Peking University (Health Sciences) ›› 2022, Vol. 54 ›› Issue (4): 686-691. doi: 10.19723/j.issn.1671-167X.2022.04.017
Previous Articles Next Articles
Risk factors of persistent hypertension in primary aldosteronism patients after surgery
Yu-chao HUANG-FU,Yi-qing DU,Lu-ping YU,Tao XU*( )
)
- Department of Urology, Peking University People' s Hospital, Beijing 100044, China
CLC Number:
- R699
| 1 |
Funder JW , Carey RM , Mantero F , et al. The management of primary aldosteronism: Case detection, diagnosis, and treatment: An endocrine society clinical practice guideline[J]. J Clin Endocrinol Metab, 2016, 101 (5): 1889- 1916.
doi: 10.1210/jc.2015-4061 |
| 2 |
Buffolo F , Burrello J , Burrello A , et al. Clinical score and machine learning-based model to predict diagnosis of primary aldosteronism in arterial hypertension[J]. Hypertension, 2021, 78 (5): 1595- 1604.
doi: 10.1161/HYPERTENSIONAHA.121.17444 |
| 3 |
Xu F , Gao Z , Wang G , et al. Prevalence, subtype classification, and outcomes of treatment of primary aldosteronism: A prospective study in china[J]. Endocr Pract, 2021, 27 (5): 478- 483.
doi: 10.1016/j.eprac.2020.10.007 |
| 4 |
Rossi GP , Bernini G , Caliumi C , et al. A prospective study of the prevalence of primary aldosteronism in 1, 125 hypertensive patients[J]. J Am Coll Cardiol, 2006, 48 (11): 2293- 2300.
doi: 10.1016/j.jacc.2006.07.059 |
| 5 |
Douma S , Petidis K , Doumas M , et al. Prevalence of primary hyperaldosteronism in resistant hypertension: A retrospective observational study[J]. Lancet, 2008, 371 (9628): 1921- 1926.
doi: 10.1016/S0140-6736(08)60834-X |
| 6 |
Calhoun DA , Nishizaka MK , Zaman MA , et al. Hyperaldosteronism among black and white subjects with resistant hypertension[J]. Hypertension, 2002, 40 (6): 892- 896.
doi: 10.1161/01.HYP.0000040261.30455.B6 |
| 7 |
Gomez-Sanchez CE , Gomez-Sanchez EP . Aldosterone-producing adenomas: Mining for genes[J]. Hypertension, 2010, 55 (6): 1306- 1307.
doi: 10.1161/HYPERTENSIONAHA.110.151480 |
| 8 | Rossi GP, Bisogni V, Bacca AV, et al. The 2020 italian society of arterial hypertension (SIIA) practical guidelines for the management of primary aldosteronism [J/OL]. Int J Cardiol Hypertens, 2020, 5: 100029[2022-03-15]. https://doi.org/10.1016/j.ijchy.2020.100029. |
| 9 |
Nishikawa T , Omura M , Satoh F , et al. Guidelines for the diagnosis and treatment of primary aldosteronism: The Japan endocrine society 2009[J]. Endocr J, 2011, 58 (9): 711- 721.
doi: 10.1507/endocrj.EJ11-0133 |
| 10 |
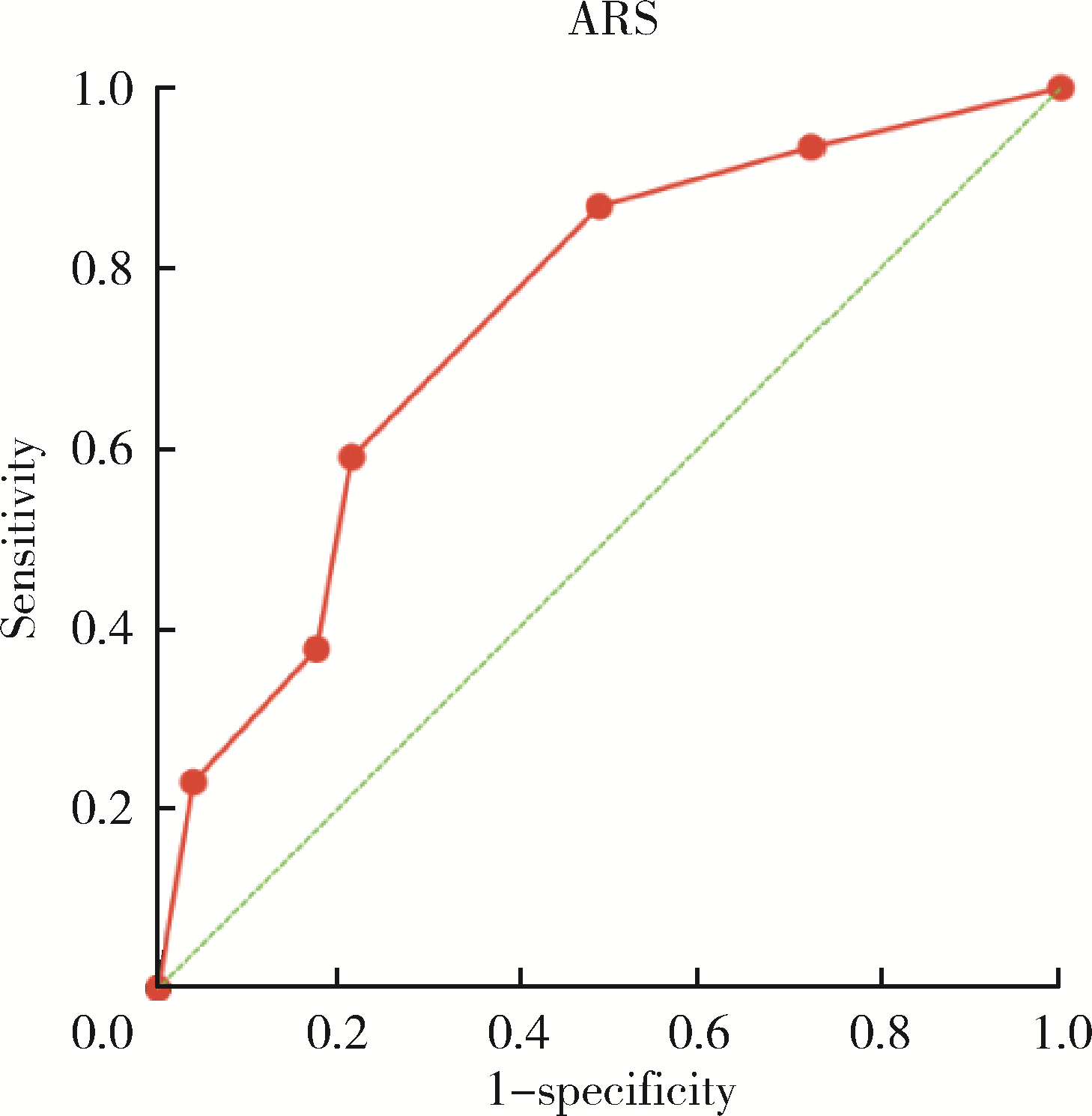
Zarnegar R , Young WF Jr. , Lee J , et al. The aldosteronoma resolution score: Predicting complete resolution of hypertension after adrenalectomy for aldosteronoma[J]. Ann Surg, 2008, 247 (3): 511- 518.
doi: 10.1097/SLA.0b013e318165c075 |
| 11 |
Romero-Velez G , Laird AM , Barajas ME , et al. Outcomes of adrenalectomy and the aldosteronoma resolution score in the black and hispanic population[J]. World J Surg, 2021, 45 (5): 1475- 1482.
doi: 10.1007/s00268-021-05967-y |
| 12 |
Utsumi T , Kawamura K , Imamoto T , et al. High predictive accuracy of aldosteronoma resolution score in japanese patients with aldosterone-producing adenoma[J]. Surgery, 2012, 151 (3): 437- 443.
doi: 10.1016/j.surg.2011.08.001 |
| 13 |
Pasquier L , Kirouani M , Fanget F , et al. Assessment of the aldosteronona resolution score as a predictive resolution score of hypertension after adrenalectomy for aldosteronoma in french patients[J]. Langenbecks Arch Surg, 2017, 402 (2): 309- 314.
doi: 10.1007/s00423-017-1557-x |
| 14 |
中华医学会内分泌学分会肾上腺学组. 原发性醛固酮增多症诊断治疗的专家共识[J]. 中华内分泌代谢杂志, 2016, 32 (3): 188- 195.
doi: 10.3760/cma.j.issn.1000-6699.2016.03.003 |
| 15 |
Williams TA , Lenders JWM , Mulatero P , et al. Outcomes after adrenalectomy for unilateral primary aldosteronism: An international consensus on outcome measures and analysis of remission rates in an international cohort[J]. Lancet Diabete Endocrinol, 2017, 5 (9): 689- 699.
doi: 10.1016/S2213-8587(17)30135-3 |
| 16 |
Milliez P , Girerd X , Plouin PF , et al. Evidence for an increased rate of cardiovascular events in patients with primary aldosteronism[J]. J Am Coll Cardiol, 2005, 45 (8): 1243- 1248.
doi: 10.1016/j.jacc.2005.01.015 |
| 17 |
Stowasser M , Sharman J , Leano R , et al. Evidence for abnormal left ventricular structure and function in normotensive individuals with familial hyperaldosteronism type Ⅰ[J]. J Clin Endocrinol Metab, 2005, 90 (9): 5070- 5076.
doi: 10.1210/jc.2005-0681 |
| 18 |
Jiang SB , Guo XD , Wang HB , et al. A retrospective study of laparoscopic unilateral adrenalectomy for primary hyperaldosteronism caused by unilateral adrenal hyperplasia[J]. Int Urol Nephrol, 2014, 46 (7): 1283- 1288.
doi: 10.1007/s11255-013-0614-9 |
| 19 | Morisaki M , Kurihara I , Itoh H , et al. Predictors of clinical success after surgery for primary aldosteronism in the japanese nationwide cohort[J]. J Endocr Soc, 2019, 3 (11): 2012- 2022. |
| 20 | Vasan RS , Beiser A , Seshadri S , et al. Residual lifetime risk for developing hypertension in middle-aged women and men: The framingham heart study[J]. Jama, 2002, 287 (8): 1003- 1010. |
| 21 | Seravalle G , Grassi G . Obesity and hypertension[J]. Pharmacol Res, 2017, 122 (1): 1- 7. |
| 22 | Nurdiantami Y , Watanabe K , Tanaka E , et al. Association of general and central obesity with hypertension[J]. Clin Nutr, 2018, 37 (4): 1259- 1263. |
| 23 | Yang Y , Williams TA , Song Y , et al. Nomogram-based preoperative score for predicting clinical outcome in unilateral primary aldosteronism[J]. J Clin Endocrinol Metab, 2020, 105 (12): e4382- e4392. |
| 24 | 何小群, 杨珊, 吴珏莅, 等. 预测原发性醛固酮增多症术后血压的转归: fisher判别模型[J]. 中华医学杂志, 2016, 96 (42): 3379- 3383. |
| [1] | Chu-yun CHEN,Peng-fei SUN,Jing ZHAO,Jia JIA,Fang-fang FAN,Chun-yan WANG,Jian-ping LI,Yi-meng JIANG,Yong HUO,Yan ZHANG. Related factors of endogenous erythropoietin and its association with 10-year risks of cardiovascular disease in a community-based Chinese study [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1068-1073. |
| [2] | Zhe LIANG,Fang-fang FAN,Yan ZHANG,Xian-hui QIN,Jian-ping LI,Yong HUO. Rate and characteristics of H-type hypertension in Chinese hypertensive population and comparison with American population [J]. Journal of Peking University (Health Sciences), 2022, 54(5): 1028-1037. |
| [3] | Zhi-sheng LI,Hao-nan QIAN,Tian-yuan FAN. Preparation and in vitro evaluation of fused deposition modeling 3D printed compound tablets of captopril and hydrochlorothiazide [J]. Journal of Peking University (Health Sciences), 2022, 54(3): 572-577. |
| [4] | WANG Wei,CAI Lin,GAO Ying,GUO Xiao-hui,ZHANG Jun-qing. Persistent and serious hyperkalemia after surgery of primary aldosteronism: A case report [J]. Journal of Peking University (Health Sciences), 2022, 54(2): 376-380. |
| [5] | XIAO Yun-shu,ZHU Feng-yun-zhi,LUO Lan,XING Xiao-yan,LI Yu-hui,ZHANG Xue-wu,SHEN Dan-hua. Clinical and immunological characteristics of 88 cases of overlap myositis [J]. Journal of Peking University (Health Sciences), 2021, 53(6): 1088-1093. |
| [6] | AN Wen-cheng,YAN Hui-xian,DENG Zheng-zhao,CHEN Fang,OU Xiao-hong,JIN Hong-xin,HUANG Wei. Chronic kidney disease after adrenalectomy in a patient with primary aldosteronism [J]. Journal of Peking University (Health Sciences), 2021, 53(6): 1201-1204. |
| [7] | KANG Wen-yu,WANG Lu,QIU Min,ZHANG Fan,GUO Wei,QIANG Ya-yong,TUO Peng-fei,ZONG You-long,LIU Lei-lei,WANG Shuai-shuai. Adrenal cavernous hemangioma: A case report and literature review [J]. Journal of Peking University (Health Sciences), 2021, 53(4): 808-810. |
| [8] | Hang YANG,Lin-cheng YANG,Rui-tao ZHANG,Yun-peng LING,Qing-gang GE. Risks factors for death among COVID-19 patients combined with hypertension, coronary heart disease or diabetes [J]. Journal of Peking University (Health Sciences), 2020, 52(3): 420-424. |
| [9] | Hong-chen ZHENG,En-ci XUE,Xue-heng WANG,Xi CHEN,Si-yue WANG,Hui HUANG,Jin JIANG,Ying YE,Chun-lan HUANG,Yun ZHOU,Wen-jing GAO,Can-qing YU,Jun LV,Xiao-ling WU,Xiao-ming HUANG,Wei-hua CAO,Yan-sheng YAN,Tao WU,Li-ming LI. Bivariate heritability estimation of resting heart rate and common chronic disease based on extended pedigrees [J]. Journal of Peking University (Health Sciences), 2020, 52(3): 432-437. |
| [10] | Wen-ying MENG,Wan-tong HUANG,Jie ZHANG,Ming-yuan JIAO,Lei JIN,Lei JIN. Relationship between serum vitamin E concentration in first trimester and the risk of developing hypertension disorders complicating pregnancy [J]. Journal of Peking University (Health Sciences), 2020, 52(3): 470-478. |
| [11] | Ying LIU,Xiang-zhu ZENG,Zheng WANG,Han ZHANG,Xi-lin WANG,Hui-shu YUAN. Cerebral blood flow measurements in patients with comorbid hypertension and depression using 3D arterial spin labeling [J]. Journal of Peking University(Health Sciences), 2019, 51(2): 260-264. |
| [12] | GUO Xiao-yue, SHAO Hui, ZHAO Yang-yu. A case of systemic lupus erythematosus in pregnancy complicated by pulmonary hypertension [J]. Journal of Peking University(Health Sciences), 2018, 50(5): 928-931. |
| [13] | DONG Yan-hui, SONG Yi, DONG Bin, ZOU Zhi-yong, WANG Zheng-he, YANG Zhao-geng, WANG Xi-jie, LI Yan-hui, MA Jun. Association between the blood pressure status and nutritional status among Chinese students aged 7-18 years in 2014: based on the national blood pressure reference for Chinese children and adolescents [J]. Journal of Peking University(Health Sciences), 2018, 50(3): 422-428. |
| [14] | ZHAO Yun, SU Bai-ge, XIAO Hui-jie, ZHANG Hong-wen, LIU Xiao-yu, WANG Fang, DING Jie. Clinical characteristics of glucocorticoid-induced eye adverse reactions in children with primary nephrotic syndrome [J]. Journal of Peking University(Health Sciences), 2017, 49(5): 794-797. |
| [15] | LIU Xue-qin, YAN Hui, QIU Jian-xing, ZHANG Chun-yu, QI Jian-guang, ZHANG Xin, XIAO Hui-jie, YANG Yan-ling, CHEN Yong-hong, DU Jun-bao. Pulmonary arterial hypertension as leading manifestation of methylmalonic aciduria: clinical characteristics and gene testing in 15 cases [J]. Journal of Peking University(Health Sciences), 2017, 49(5): 768-777. |
|
||