Journal of Peking University (Health Sciences) ›› 2025, Vol. 57 ›› Issue (3): 430-435. doi: 10.19723/j.issn.1671-167X.2025.03.004
Previous Articles Next Articles
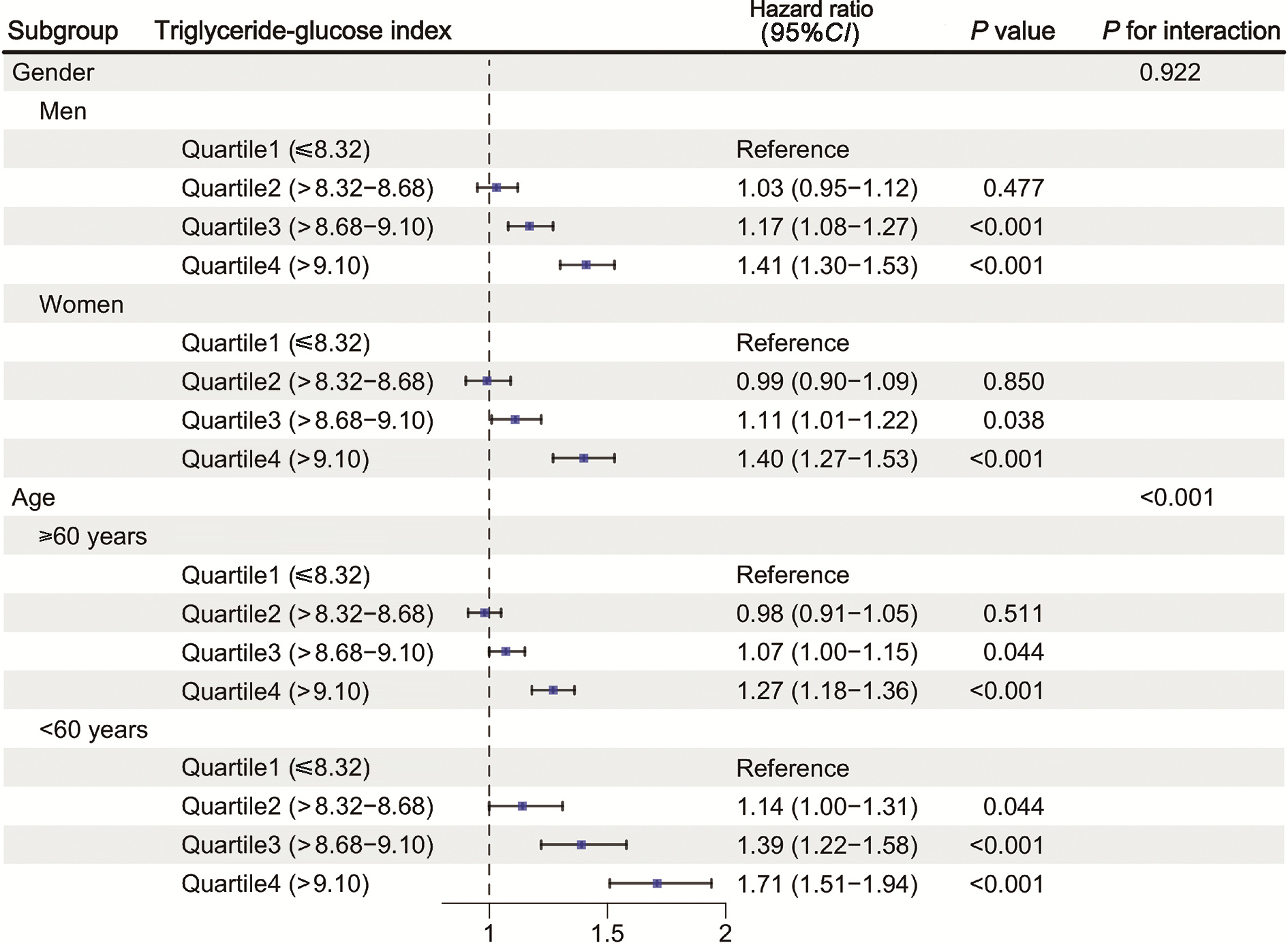
Association of triglyceride-glucose index and cardiovascular disease in a community-based Chinese cohort
Mengxi LU1, Qiuping LIU1, Tianjing ZHOU1, Xiaofei LIU1, Yexiang SUN2, Peng SHEN2, Hongbo LIN2, Xun TANG1,3,*( ), Pei GAO1,3,4,*(
), Pei GAO1,3,4,*( )
)
- 1. Department of Epidemiology and Biostatistics, Peking University School of Public Health, Beijing 100191, China
2. Yinzhou District Center for Disease Control and Prevention, Ningbo 315101, Zhejiang, China
3. Key Laboratory of Epidemiology of Major Disease (Peking University), Ministry of Education, Beijing 100191, China
4. Center for Real-World Evidence Evaluation, Peking University Clinical Research Institute, Beijing 100191, China
CLC Number:
- R54
| 1 |
doi: 10.1161/CIR.0000000000001191 |
| 2 |
doi: 10.1016/j.jacc.2019.03.009 |
| 3 |
doi: 10.1002/dmrr.3502 |
| 4 |
doi: 10.1186/s12933-021-01268-9 |
| 5 |
doi: 10.1186/s12933-024-02571-x |
| 6 |
doi: 10.1186/s12933-022-01511-x |
| 7 |
doi: 10.1186/s12933-024-02244-9 |
| 8 |
doi: 10.1136/bmjopen-2017-019698 |
| 9 |
doi: 10.1186/s12916-020-01824-2 |
| 10 |
doi: 10.1016/S2214-109X(19)30318-3 |
| 11 |
|
| 12 |
doi: 10.1186/s12933-022-01546-0 |
| 13 |
doi: 10.1093/eurjpc/zwae025 |
| 14 |
doi: 10.1038/s41598-019-43776-5 |
| 15 |
doi: 10.1186/s12933-023-02115-9 |
| 16 |
doi: 10.1093/eurheartj/ehab484 |
| 17 |
|
| 18 |
doi: 10.1016/S2214-109X(24)00210-9 |
| 19 |
doi: 10.1186/s12933-024-02334-8 |
| 20 |
doi: 10.1186/s12933-022-01456-1 |
| [1] | Wei LIU, Wen GUO, Zhe GUO, Chunyan LI, Yunlong LI, Siqi LIU, Liang ZHANG, Hui SONG. Risk factors associated with non-radiographic bone erosion in patients with gout [J]. Journal of Peking University (Health Sciences), 2025, 57(4): 735-739. |
| [2] | Huaqiu GUO, Zhe WANG, Xue YANG, Jie BAI. Clinical features and risk factors of patients with oral bleeding in dental emergency [J]. Journal of Peking University (Health Sciences), 2025, 57(1): 142-147. |
| [3] | Minting DENG, Nan WANG, Bin XIA, Yuming ZHAO, Junxia ZHU. Factors associated with spontaneous re-eruption of traumatically intruded permanent anterior teeth in children and adolescents [J]. Journal of Peking University (Health Sciences), 2025, 57(1): 148-153. |
| [4] | Yukai LI, Hongyan WANG, Liang LUO, Yun LI, Chun LI. Clinical significance of antiphospholipid antibodies in Behcet disease with thrombosis [J]. Journal of Peking University (Health Sciences), 2024, 56(6): 1036-1040. |
| [5] | Yang TIAN, Yongzheng HAN, Jiao LI, Mingya WANG, Yinyin QU, Jingchao FANG, Hui JIN, Min LI, Jun WANG, Mao XU, Shenglin WANG, Xiangyang GUO. Incidence and risk factors of postoperative epidural hematoma following anterior cervical spine surgery [J]. Journal of Peking University (Health Sciences), 2024, 56(6): 1058-1064. |
| [6] | Mingrui WANG, Jinhui LAI, Jiaxiang JI, Xinwei TANG, Haopu HU, Qi WANG, Kexin XU, Tao XU, Hao HU. Risk factors for decreased quality of life in patients with kidney stones predicted by the Chinese version of Wisconsin stone quality of life questionnaire [J]. Journal of Peking University (Health Sciences), 2024, 56(6): 1069-1074. |
| [7] | Zhicun LI, Tianyu WU, Lei LIANG, Yu FAN, Yisen MENG, Qian ZHANG. Risk factors analysis and nomogram model construction of postoperative pathological upgrade of prostate cancer patients with single core positive biopsy [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 896-901. |
| [8] | Ye YAN,Xiaolong LI,Haizhui XIA,Xuehua ZHU,Yuting ZHANG,Fan ZHANG,Ke LIU,Cheng LIU,Lulin MA. Analysis of risk factors for long-term overactive bladder after radical prostatectomy [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 589-593. |
| [9] | Shengqi ZHENG,Tianchi HUA,Guicao YIN,Wei ZHANG,Ye YAO,Yifan LI. Association between the triglyceride-glucose index and the incidence of nephrolithiasis in male individuals [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 610-616. |
| [10] | Yan CHEN,Kuangmeng LI,Kai HONG,Shudong ZHANG,Jianxing CHENG,Zhongjie ZHENG,Wenhao TANG,Lianming ZHAO,Haitao ZHANG,Hui JIANG,Haocheng LIN. Retrospective study on the impact of penile corpus cavernosum injection test on penile vascular function [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 680-686. |
| [11] | Bo PANG,Tongjun GUO,Xi CHEN,Huaqi GUO,Jiazhang SHI,Juan CHEN,Xinmei WANG,Yaoyan LI,Anqi SHAN,Hengyi YU,Jing HUANG,Naijun TANG,Yan WANG,Xinbiao GUO,Guoxing LI,Shaowei WU. Personal nitrogen oxides exposure levels and related influencing factors in adults over 35 years old in Tianjin and Shanghai [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 700-707. |
| [12] | Jing HE,Zhongze FANG,Ying YANG,Jing LIU,Wenyao MA,Yong HUO,Wei GAO,Yangfeng WU,Gaoqiang XIE. Relationship between lipid metabolism molecules in plasma and carotid atheroscle-rotic plaques, traditional cardiovascular risk factors, and dietary factors [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 722-728. |
| [13] | Huangda GUO,Hexiang PENG,Siyue WANG,Tianjiao HOU,Yixin LI,Hanyu ZHANG,Mengying WANG,Yiqun WU,Xueying QIN,Xun TANG,Jing LI,Dafang CHEN,Yonghua HU,Tao WU. A ssociations of short-term ambient particulate matter exposure and MTNR1B gene with triglyceride-glucose index: A family-based study [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 375-383. |
| [14] | Shan CAI,Yihang ZHANG,Ziyue CHEN,Yunfe LIU,Jiajia DANG,Di SHI,Jiaxin LI,Tianyu HUANG,Jun MA,Yi SONG. Status and pathways of factors influencing physical activity time among elementary and junior high school students in Beijing [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 403-410. |
| [15] | Zuhong ZHANG,Tianjiao CHEN,Jun MA. Associations between puberty timing and cardiovascular metabolic risk factors among primary and secondary students [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 418-423. |
|
||