Journal of Peking University (Health Sciences) ›› 2025, Vol. 57 ›› Issue (5): 975-979. doi: 10.19723/j.issn.1671-167X.2025.05.024
Previous Articles Next Articles
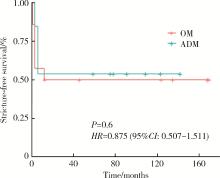
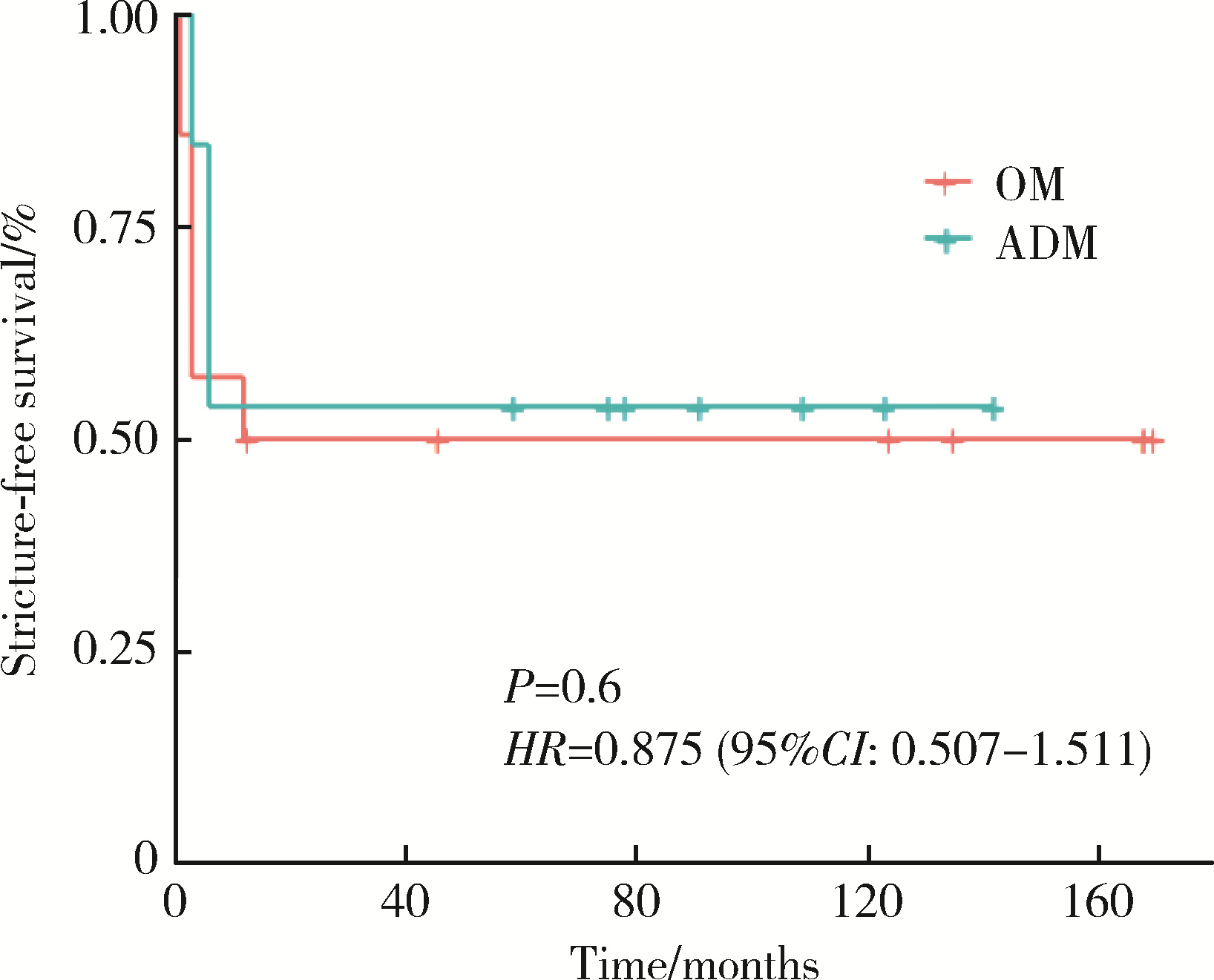
Comparison of efficacy and safety of oral mucosa grafts and acellular dermal matrix grafts in the treatment of long-segment urethral stricture
Wenyuan LENG, Duan GAO, Xiaoyu LI, Wei ZUO, Weimin HU, Zhenpeng ZHU, Chunru XU, Jian LIN*( ), Xuesong LI*(
), Xuesong LI*( )
)
- Department of Urology, Peking University First Hospital; Institute of Urology, Peking University; National Urological Cancer Center, Beijing 100034, China
CLC Number:
- R699.6
| 1 |
doi: 10.1016/j.eururo.2021.05.022 |
| 2 |
doi: 10.1016/j.juro.2016.07.087 |
| 3 |
doi: 10.1016/j.juro.2009.05.023 |
| 4 |
徐月敏. 尿道狭窄的病因与治疗现状[J]. 中华泌尿外科杂志, 2011, 32 (11): 725- 727.
|
| 5 |
doi: 10.1007/s11934-018-0769-0 |
| 6 |
doi: 10.3390/biomedicines9121917 |
| 7 |
doi: 10.1016/j.juro.2018.02.3102 |
| 8 |
doi: 10.1016/j.ebiom.2017.08.014 |
| 9 |
陈彩芳, 曾铭强, 薛睿智, 等. 男性尿道狭窄病因与治疗方式[J]. 中南大学学报(医学版), 2018, 43 (5): 520- 527.
|
| 10 |
doi: 10.21037/tau-21-1149 |
| 11 |
林健, 郝金瑞, 金杰, 等. 人同种异体真皮脱细胞基质在尿道重建中的临床应用[J]. 中华医学杂志, 2005, 85 (15): 1057- 1059.
|
| 12 |
徐月敏, 张炯, 傅强, 等. 小肠黏膜下脱细胞基质修复前尿道狭窄的疗效分析[J]. 中华泌尿外科杂志, 2011, 32 (6): 419- 422.
|
| 13 |
doi: 10.1007/s00345-024-04795-8 |
| 14 |
doi: 10.1111/iju.14786 |
| 15 |
doi: 10.1177/2192568217701105 |
| [1] | Jie WANG, Jianwei WANG, Haizhui XIA, Xiao XU, Jianpo ZHAI, Feng HE, Guanglin HUANG, Guizhong LI. Surgical management of the distal urethral stricture diseases [J]. Journal of Peking University (Health Sciences), 2024, 56(6): 1075-1082. |
| [2] | WANG Jian-wei,XU Xiao,BAO Zheng-qing,LIU Zhen-hua,HE Feng,HUANG Guang-lin,MAN Li-bo. Outcomes of partial pubectomy assisted anastomotic urethroplasty for male patients with pelvic fracture urethral distraction defect [J]. Journal of Peking University (Health Sciences), 2021, 53(4): 798-802. |
| [3] | Chun-long ZHANG,He LI,Qing LI,Wen-jun BAI,Tao XU,Xiao-wei ZHANG. Decision regret analysis among Chinese patients receiving penile girth enhancement with acellular dermal matrix [J]. Journal of Peking University (Health Sciences), 2020, 52(4): 678-683. |
| [4] | Jian-wei WANG,Li-bo MAN,Xiao XU,Zhen-hua LIU,Feng HE,Guang-lin HUANG,Jian-po ZHAI,Ning ZHOU,Wei LI. Combined transperineal and transpubic urethroplasty for patients with complex male pelvic fracture urethral distraction defect [J]. Journal of Peking University (Health Sciences), 2020, 52(4): 646-650. |
| [5] | Zhong-cheng XIN,Bi-cheng YANG,Meng LI,Yi-ming YUAN,Wan-shou CUI,Yuan TANG,Dong FANG,Wei-dong SONG. Appllication of human acellular dermal matrix in surgical treatment of genitourinary disease [J]. Journal of Peking University(Health Sciences), 2019, 51(4): 778-782. |
| [6] | Jian-wei WANG,Li-bo MAN,Guang-lin HUANG,Feng HE,Hai WANG,Hai-dong WANG,Xiao XU,Wei LI,Jian-po ZHAI,Zhen-hua LIU. Single-stage repair of penile urethral stricture using combined dorsal onlay oral mucosa grafting with ventral onlay penile skin flap [J]. Journal of Peking University(Health Sciences), 2019, 51(4): 641-645. |
| [7] | Ting-min XU,Xiao-wei ZHANG,Guo-xi ZHANG,Wen-jun BAI,Qing LI,Tao XU. Complications and management for penile augmentation with acellular dermal matrix [J]. Journal of Peking University(Health Sciences), 2019, 51(4): 636-640. |
| [8] | WANG Jian-wei, MAN Li-bo, HUANG Guang-lin, WANG Hai, Xu Xiao, ZHU Xiao-fei, LI Wei, LIU Zhen-hua. “3-step” strategy of transperineal anastomotic urethroplasty for the simple pelvic fracture urethral distraction defect in male patients [J]. Journal of Peking University(Health Sciences), 2018, 50(4): 617-620. |
| [9] | XIE Tian-Peng, HUANG Xiao-Bo, XU Qing-Quan, YE Hai-Yun, YANG Qing-Ya, WANG Xiao-Feng. Balloon dilation by B ultrasound monitoring for treatment of urethral stricture: 5 case reports [J]. Journal of Peking University(Health Sciences), 2014, 46(4): 657-658. |
| [10] | HUANG Guang-Lin, MAN Li-Bo, WANG Hai, WANG Jian-Wei, DI Jian-Po, ZHU Xiao-Fei, ZHOU Ning, XU Xiao. Management of female urethral obliteration with the rotary excision appliance [J]. Journal of Peking University(Health Sciences), 2014, 46(4): 574-577. |
|
||