Journal of Peking University(Health Sciences) ›› 2020, Vol. 52 ›› Issue (1): 30-34. doi: 10.19723/j.issn.1671-167X.2020.01.005
Previous Articles Next Articles
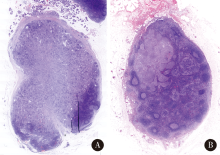
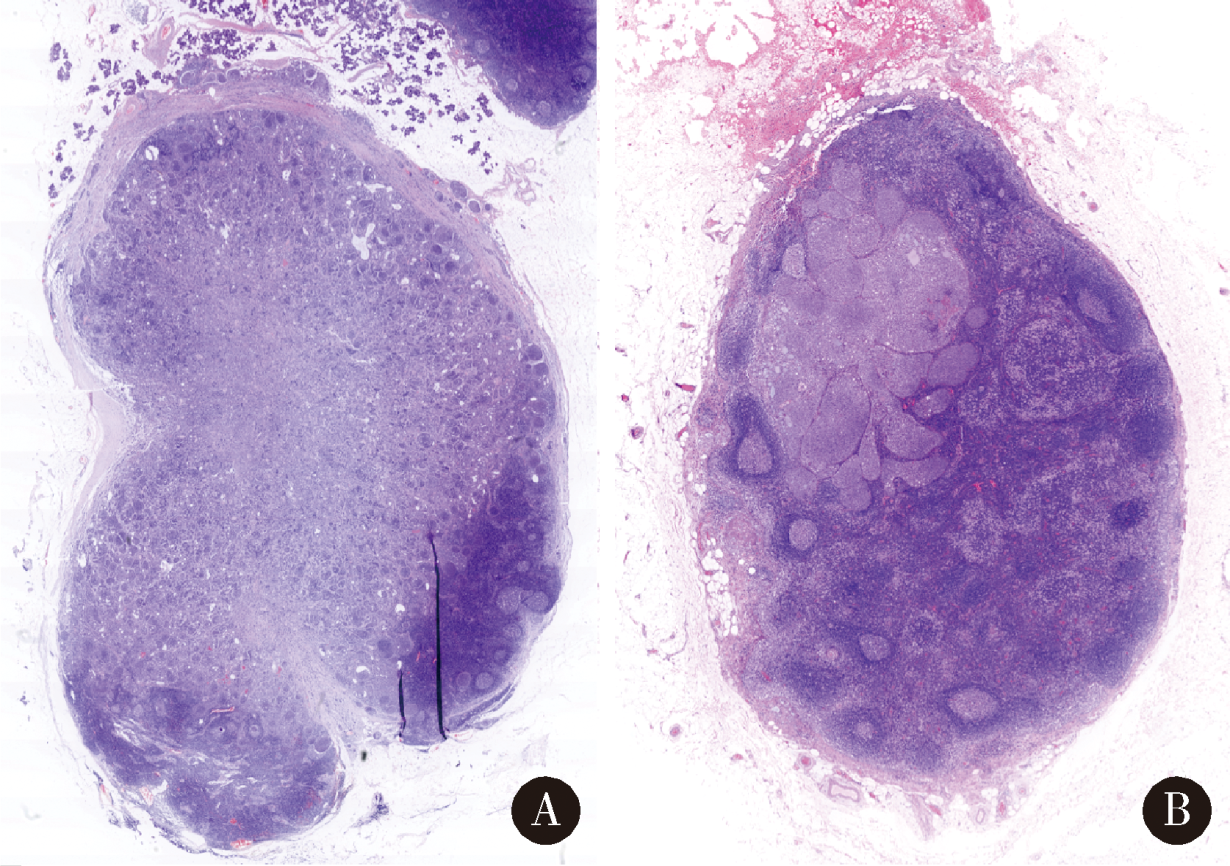
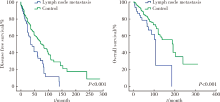
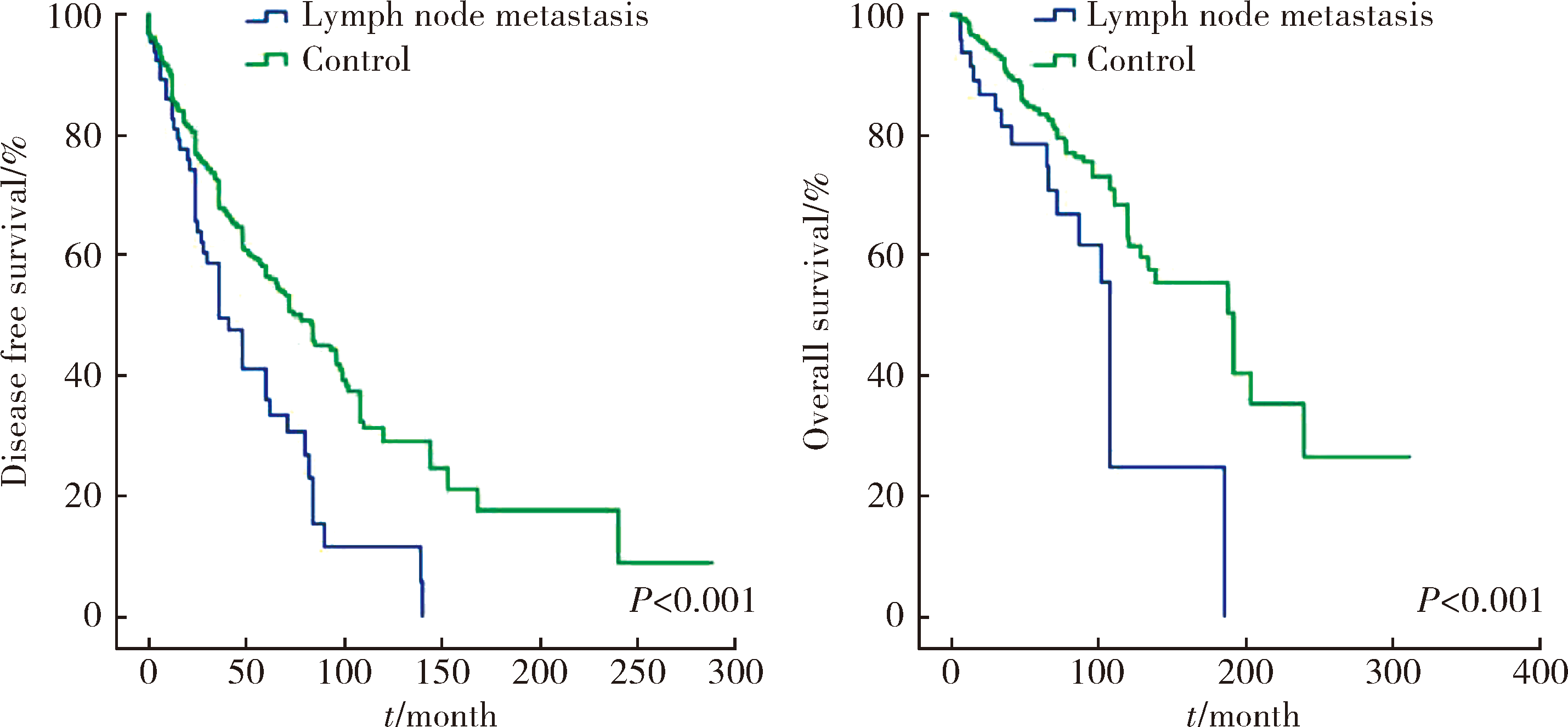
Cervical lymph node metastasis in adenoid cystic carcinoma of the salivary glands: A clinicopathologic study
Ye ZHANG,Ni ZHANG,Xiao-xiao LIU,Chuan-xiang ZHOU( )
)
- Department of Oral Pathology, Peking University School and Hospital of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Laboratory for Digital and Material Technology of Stomatology & Beijing Key Laboratory of Digital Stomatology, Beijing 100081, China
CLC Number:
- R739.87
| [1] | Tian Z, Li L, Wang L , et al. Salivary gland neoplasms in oral and maxillofacial regions: A 23-year retrospective study of 6 982 cases in an eastern Chinese population[J]. Int J Oral Maxillofac Surg, 2010,39(3):235-242. |
| [2] | Gao M, Hao Y, Huang MX , et al. Clinicopathological study of distant metastases of salivary adenoid cystic carcinoma[J]. Int J Oral Maxillofac Surg, 2013,42(8):923-928. |
| [3] | Shen C, Xu T, Huang C , et al. Treatment outcomes and prognostic features in adenoid cystic carcinoma originated from the head and neck[J]. Oral Oncol, 2012,48(5):445-449. |
| [4] | Lloyd S, Yu JB, Wilson LD , et al. Determinants and patterns of survival in adenoid cystic carcinoma of the head and neck, including an analysis of adjuvant radiation therapy[J]. Am J Clin Oncol, 2011,34(1):76-81. |
| [5] | Bhayani MK, Yener M, El-Naggar A , et al. Prognosis and risk factors for early-stage adenoid cystic carcinoma of the major salivary glands[J]. Cancer, 2012,118(11):2872-2878. |
| [6] | Armstrong JG, Harrison LB, Thaler HT , et al. The indications for elective treatment of the neck in cancer of the major salivary glands[J]. Cancer, 1992,69(3):615-619. |
| [7] | Suárez C, Barnes L, Silver CE , et al. Cervical lymph node metastasis in adenoid cystic carcinoma of oral cavity and oropharynx: A collective international review[J]. Auris Nasus Larynx, 2016,43(5):477-484. |
| [8] | Ardekian L, Kokemueller H, Eckardt A , et al. Adenoid cystic carcinoma of the head and neck: A 20 years experience[J]. Int J Oral Maxillofac Surg, 2004,33(1):25-31. |
| [9] | Bianchi B, Copelli C, Cocchi R , et al. Adenoid cystic carcinoma of intraoral minor salivary glands[J]. Oral Oncol, 2008,44(11):1026-1031. |
| [10] | Coca-Pelaz A, Rodrigo JP, Bradley PJ , et al. Adenoid cystic carcinoma of the head and neck: An update[J]. Oral Oncol, 2015,51(7):652-661. |
| [11] | Zhang M, Xu ZF, Tao Y , et al. Clinical analysis of 25 patients with glossal adenoid cystic carcinoma[J]. Int J Stomt, 2009,36(2):148-151. |
| [12] | Min R, Siyi L, Wenjun Y , et al. Salivary gland adenoid cystic carcinoma with cervical lymph node metastasis: A preliminary study of 62 cases[J]. Int J Oral Maxillofac Surg, 2012,41(8):952-957. |
| [13] | Amit M, Binenbaum Y, Sharma K , et al. Incidence of cervical lymph node metastasis and its association with outcomes in patients with adenoid cystic carcinoma. An international collaborative study[J]. Head Neck, 2015,37(7):1032-1037. |
| [14] | Weinreb I, Lee SY, Kim BH , et al. Nineteen-year oncologic outcomes and the benefit of elective neck dissection in salivary gland adenoid cystic carcinoma[J]. Head Neck, 2014,36(12):1796-1801. |
| [15] | Ali S, Palmer FL, Katabi N , et al. Long-term local control rates of patients with adenoid cystic carcinoma of the head and neck managed by surgery and postoperative radiation[J]. Laryngoscope, 2017,127(10):2265-2269. |
| [16] | Nakada M, Nishizaki K, Akagi H , et al. Oncocytic carcinoma of the submandibular gland: a case report and literature review[J]. J Oral Pathol Med, 1998,27(5):225-228. |
| [17] | Amit M, Na’ara S, Sharma K , et al. Elective neck dissection in patients with head and neck adenoid cystic carcinoma: An international collaborative study[J]. Ann Surg Oncol, 2015,22(4):1353-1359. |
| [1] | Dongwu LIU, Jie CHEN, Mingli GAO, Jing YU. Rheumatoid arthritis with Castleman-like histopathology in lymph nodes: A case report [J]. Journal of Peking University (Health Sciences), 2024, 56(5): 928-931. |
| [2] | Yuxuan TIAN,Mingjian RUAN,Yi LIU,Derun LI,Jingyun WU,Qi SHEN,Yu FAN,Jie JIN. Predictive effect of the dual-parametric MRI modified maximum diameter of the lesions with PI-RADS 4 and 5 on the clinically significant prostate cancer [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 567-574. |
| [3] | Shuai LIU,Lei LIU,Zhuo LIU,Fan ZHANG,Lulin MA,Xiaojun TIAN,Xiaofei HOU,Guoliang WANG,Lei ZHAO,Shudong ZHANG. Clinical treatment and prognosis of adrenocortical carcinoma with venous tumor thrombus [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 624-630. |
| [4] | Fan SHU,Yichang HAO,Zhanyi ZHANG,Shaohui DENG,Hongxian ZHANG,Lei LIU,Guoliang WANG,Xiaojun TIAN,Lei ZHAO,Lulin MA,Shudong ZHANG. Functional and oncologic outcomes of partial nephrectomy for cystic renal cell carcinoma: A single-center retrospective study [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 667-672. |
| [5] | Zezhen ZHOU,Shaohui DENG,Ye YAN,Fan ZHANG,Yichang HAO,Liyuan GE,Hongxian ZHANG,Guoliang WANG,Shudong ZHANG. Predicting the 3-year tumor-specific survival in patients with T3a non-metastatic renal cell carcinoma [J]. Journal of Peking University (Health Sciences), 2024, 56(4): 673-679. |
| [6] | Zhanhong LAI,Jiachen LI,Zelin YUN,Yonggang ZHANG,Hao ZHANG,Xiaoyan XING,Miao SHAO,Yuebo JIN,Naidi WANG,Yimin LI,Yuhui LI,Zhanguo LI. A unicenter real-world study of the correlation factors for complete clinical response in idiopathic inflammatory myopathies [J]. Journal of Peking University (Health Sciences), 2024, 56(2): 284-292. |
| [7] | Junqi SU,Xiaoying WANG,Zhiqiang SUN. Establishment and verification of a prognostic nomogram for survival of tongue squamous cell carcinoma patients who underwent cervical dissection [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 120-130. |
| [8] | Xunmin XU,Xiao SHAO,Aiping JI. Analysis of death cases in the oral emergency department [J]. Journal of Peking University (Health Sciences), 2024, 56(1): 185-189. |
| [9] | Lu FENG,Jia-yu ZHAI,Jin-xia ZHAO. Medical visit status and clinical features in patients with IgG4 related disease [J]. Journal of Peking University (Health Sciences), 2023, 55(6): 1028-1032. |
| [10] | Yun-chong LIU,Zong-long WU,Li-yuan GE,Tan DU,Ya-qian WU,Yi-meng SONG,Cheng LIU,Lu-lin MA. Mechanism of nuclear protein 1 in the resistance to axitinib in clear cell renal cell carcinoma [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 781-792. |
| [11] | Dong LAN,Zhuo LIU,Yu-xuan LI,Guo-liang WANG,Xiao-jun TIAN,Lu-lin MA,Shu-dong ZHANG,Hong-xian ZHANG. Risk factors for massive hemorrhage after radical nephrectomy and removal of venous tumor thrombus [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 825-832. |
| [12] | Hui WEI, Ci-dan-yang-zong, Yi-xi-la-mu, Bai-ma-yang-jin. Risk factors associated with different types of Henoch-Schönlein purpura in Tibetan patients at high altitude [J]. Journal of Peking University (Health Sciences), 2023, 55(5): 923-928. |
| [13] | Shang XIE,Zhi-gang CAI,Xiao-feng SHAN. Application value of whole exon sequencing and immune related indicators in the precision treatment of oral squamous cell carcinoma [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 697-701. |
| [14] | Han LU,Jian-yun ZHANG,Rong YANG,Le XU,Qing-xiang LI,Yu-xing GUO,Chuan-bin GUO. Clinical factors affecting the prognosis of lower gingival squamous cell carcinoma [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 702-707. |
| [15] | Yun-fei SHI,Hao-jie WANG,Wei-ping LIU,Lan MI,Meng-ping LONG,Yan-fei LIU,Yu-mei LAI,Li-xin ZHOU,Xin-ting DIAO,Xiang-hong LI. Analysis of clinicopathological and molecular abnormalities of angioimmunoblastic T-cell lymphoma [J]. Journal of Peking University (Health Sciences), 2023, 55(3): 521-529. |
|
||