Journal of Peking University (Health Sciences) ›› 2025, Vol. 57 ›› Issue (2): 347-353. doi: 10.19723/j.issn.1671-167X.2025.02.020
Previous Articles Next Articles
Correlation analysis of peri-implant health after single-tooth dental implant
- 1. Department of Periodontology, Peking University School and Hospital of Stomatology, Beijing 100081, China
2. Second Clinical Division, Peking University School and Hospital of Stomatology & National Center of Stomatology & National Clinical Research Center for Oral Diseases & National Engineering Research Center of Oral Biomaterials and Digital Medical Devices & Beijing Key Laboratory of Digital Stomatology & NHC Research Center of Engineering and Technology for Computerized Dentistry & NMPA Key Laboratory for Dental Materials, Beijing 100081, China
CLC Number:
- R783.6
| 1 | Raghoebar GM , Meijer HJ , Slot W , et al. A systematic review of implant-supported overdentures in the edentulous maxilla, compared to the mandible: How many implants?[J]. Eur J Oral Implantol, 2014, 7 (Suppl 2): S191- S201. |
| 2 | Sailer I , Mühlemann S , Zwahlen M , et al. Cemented and screw-retained implant reconstructions: A systematic review of the survival and complication rates[J]. Clin Oral Implants Res, 2012, 23 (Suppl 6): 163- 201. |
| 3 | Meyle J , Casado P , Fourmousis , et al. General genetic and acquired risk factors, and prevalence of peri-implant diseases: Consensus report of working group 1[J]. Int Dent J, 2019, 69 (Suppl 2): 3- 6. |
| 4 |
Vignoletti F , Di Domenico GL , Di Martino M , et al. Prevalence and risk indicators of peri-implantitis in a sample of university-based dental patients in Italy: A cross-sectional study[J]. J Clin Periodontol, 2019, 46 (5): 597- 605.
doi: 10.1111/jcpe.13111 |
| 5 | 余道信, 程梦, 金辉喜. 种植体周围病的发生率及其危险因素[J]. 武汉大学学报(医学版), 2019, 40 (5): 845- 849. |
| 6 | 张停停, 胡晓菁, 林璐. 种植体植入15年内种植体周围炎和种植周黏膜炎发生率调查[J]. 上海口腔医学, 2021, 30 (3): 292- 296. |
| 7 |
Schwendicke F , Tu YK , Stolpe M . Preventing and treating peri-implantitis: A cost-effectiveness analysis[J]. J Periodontol, 2015, 86 (9): 1020- 1029.
doi: 10.1902/jop.2015.150071 |
| 8 | Schwarz F , Alcoforado G , Guerrero A , et al. Peri-implantitis: Summary and consensus statements of group 3. The 6th EAO consensus conference 2021[J]. Clin Oral Implants Res, 2021, 32 (Suppl 21): 245- 253. |
| 9 |
Mombelli A , van Oosten MAC , Schürch Jr. E , et al. The microbiota associated with successful or failing osseointegrated titanium implants[J]. Oral Microbiol Immunol, 1987, 2 (4): 145- 151.
doi: 10.1111/j.1399-302X.1987.tb00298.x |
| 10 | Jemt T . Restoring the gingival contour by means of provisional resin crowns after single-implant treatment[J]. Int J Periodontics Restorative Dent, 1999, 19 (1): 20- 29. |
| 11 |
Wada M , Mameno T , Onodera Y , et al. Prevalence of peri-implant disease and risk indicators in a Japanese population with at least 3 years in function: A multicentre retrospective study[J]. Clin Oral Implants Res, 2019, 30 (2): 111- 120.
doi: 10.1111/clr.13397 |
| 12 | Yotnuengnit B , Yotnuengnit P , Laohapand P , et al. Emergence angles in natural anterior teeth: Influence on periodontal status[J]. Quintessence Int, 2008, 39 (3): e126- e133. |
| 13 | Blanes RJ . To what extent does the crown-implant ratio affect the survival and complications of implant-supported reconstructions? A systematic review[J]. Clin Oral Implants Res, 2010, 20 (Suppl 4): 67- 72. |
| 14 |
Chanthasan S , Mattheos N , Pisarnturakit PP , et al. Influence of interproximal peri-implant tissue and prosthesis contours on food impaction, tissue health and patients' quality of life[J]. Clin Oral Implants Res, 2022, 33 (7): 768- 781.
doi: 10.1111/clr.13958 |
| 15 |
Jeong JS , Chang M . Food impaction and periodontal/peri-implant tissue conditions in relation to the embrasure dimensions between implant-supported fixed dental prostheses and adjacent teeth: A cross-sectional study[J]. J Periodontol, 2015, 86 (12): 1314- 1320.
doi: 10.1902/jop.2015.150322 |
| 16 | Berglundh T , Armitage G , Araujo MG , et al. Peri-implant diseases and conditions: Consensus report of workgroup 4 of the 2017 world workshop on the classification of periodontal and peri-implant diseases and conditions[J]. J Periodontol, 2018, 89 (Suppl 1): S313- S318. |
| 17 | Sanz M , Chapple IL . Working group 4 of the Ⅷ European workshop on periodontology. Clinical research on peri-implant diseases: Consensus report of working group 4[J]. J Clin Periodontol, 2012, 39 (Suppl 12): 202- 206. |
| 18 | Renvert S , Persson GR , Pirih FQ , et al. Peri-implant health, peri-implant mucositis, and peri-implantitis: Case definitions and diagnostic considerations[J]. J Periodontol, 2018, 89 (Suppl 1): S304- S312. |
| 19 |
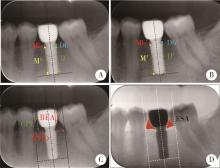
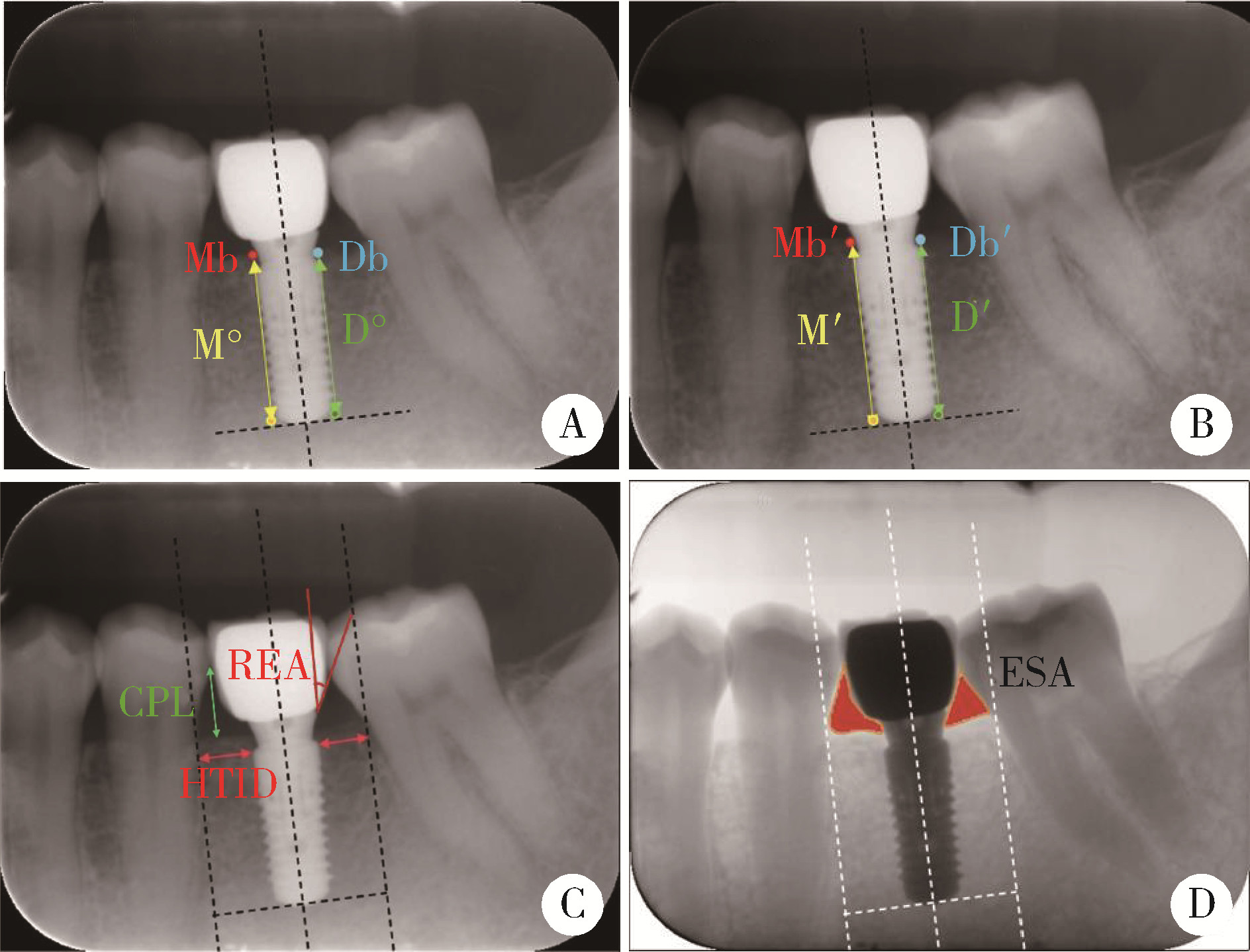
Katafuchi M , Weinstein BF , Leroux BG , et al. Restoration contour is a risk indicator for peri-implantitis: A cross-sectional radiographic analysis[J]. J Clin Periodontol, 2018, 45 (2): 225- 232.
doi: 10.1111/jcpe.12829 |
| 20 |
Yi Y , Koo KT , Schwarz F , et al. Association of prosthetic features and peri-implantitis: A cross-sectional study[J]. J Clin Periodontol, 2020, 47 (3): 392- 403.
doi: 10.1111/jcpe.13251 |
| 21 | Wong AT , Wat PY , Pow EH , et al. Proximal contact loss between implant-supported prostheses and adjacent natural teeth: A retrospective study[J]. Clin Oral Implants Res, 2015, 26 (4): e68- 71. |
| 22 |
Wat PY , Wong AT , Leung KC . Proximal contact loss between implant-supported prostheses and adjacent natural teeth: A Clinical Report[J]. J Prosthet Dent, 2011, 105 (1): 1- 4.
doi: 10.1016/S0022-3913(10)00174-5 |
| 23 |
Saber A , Chakar C , Mokbel N , et al. Prevalence of interproximal contact loss between implant-supported fixed prostheses and adjacent teeth and its impact on marginal bone loss: A retrospective study[J]. Int J Oral Maxillofac Implants, 2020, 35 (3): 625- 630.
doi: 10.11607/jomi.7926 |
| 24 |
Byun SJ , Heo SM , Ahn SG , et al. Analysis of proximal contact loss between implant-supported fixed dental prostheses and adjacent teeth in relation to influential factors and effects. A cross-sectional study[J]. Clin Oral Implants Res, 2015, 26 (6): 709- 714.
doi: 10.1111/clr.12373 |
| 25 | 罗强, 丁茜, 张磊, 等. 后牙种植冠桥修复邻接触丧失的临床回顾研究[J]. 中华口腔医学杂志, 2016, 51 (1): 15- 19. |
| 26 |
Pang NS , Suh CS , Kim KD , et al. Prevalence of proximal contact loss between implant-supported fixed prostheses and adjacent natural teeth and its associated factors: A 7-year prospective study[J]. Clin Oral Implants Res, 2017, 28 (12): 1501- 1508.
doi: 10.1111/clr.13018 |
| 27 | Wei H , Tomotake Y , Nagao K , et al. Implant prostheses and adjacent tooth migration: Preliminary retrospective survey using 3-dimensional occlusal analysis[J]. Int J Prosthodont, 2008, 21 (4): 302- 304. |
| 28 | Varthis S , Randi A , Tarnow DP . Prevalence of interproximal open contacts between single-implant restorations and adjacent teeth[J]. Int J Oral Maxillofac Implants, 2016, 31 (5): 1089- 1092. |
| 29 | Koori H , Morimoto K , Tsukiyama Y , et al. Statistical analysis of the diachronic loss of interproximal contact between fixed implant prostheses and adjacent teeth[J]. Int J Prosthodont, 2010, 23 (6): 535- 540. |
| 30 | Ramanauskaite A , Roccuzzo A , Schwarz F . A systematic review on the influence of the horizontal distance between two adjacent implants inserted in the anterior maxilla on the inter-implant mucosa fill[J]. Clin Oral Implants Res, 2018, 29 (Suppl 15): 62- 70. |
| 31 | Jung RE , Heitz-Mayfield L , Schwarz F . Evidence-based knowledge on the aesthetics and maintenance of peri-implant soft tissues: Osteology foundation consensus report part 3: Aesthetics of peri-implant soft tissues[J]. Clin Oral Implants Res, 2018, 29 (Suppl 15): 14- 17. |
| 32 | Wu YJ , Tu YK , Huang SM , et al. The influence of the distance from the contact point to the crest of bone on the presence of the interproximal dental papilla[J]. Chang Gung Med J, 2003, 26 (11): 822- 828. |
| 33 |
Tarnow D , Elian N , Fletcher P , et al. Vertical distance from the crest of bone to the height of the interproximal papilla between adjacent implants[J]. J Periodontol, 2003, 74 (12): 1785- 1788.
doi: 10.1902/jop.2003.74.12.1785 |
| 34 |
Peng ZZ , Chen XM , Wang J , et al. Effect of proximal contact strength on the three-dimensional displacements of implant-supported cantilever fixed partial dentures under axial loading[J]. J Zhejiang Univ Sci B, 2013, 14 (6): 526- 532.
doi: 10.1631/jzus.B1200264 |
| 35 | Cosyn J , Sabzevar MM , Bruyn HD . Predictors of inter-proximal and midfacial recession following single implant treatment in the anterior maxilla: A multivariate analysis[J]. J Clin Periodontol, 2012, 39 (9): 895- 903. |
| [1] | Yuanyuan ZENG,Yun XIE,Daonan CHEN,Ruilan WANG. Related factors of euthyroid sick syndrome in patients with sepsis [J]. Journal of Peking University (Health Sciences), 2024, 56(3): 526-532. |
| [2] | Qiang FU,Guan-ying GAO,Yan XU,Zhuo-hua LIN,You-jing SUN,Li-gang CUI. Comparative study of ultrasound and magnetic resonance imaging in the diagnosis of asymptomatic anterosuperior acetabular labrum tears [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 665-669. |
| [3] | Yong-wei LIN,Ya-lin ZHOU,Run-long ZHAO,Ya-jun XU,Yan-ping LIU. Analysis on the iron status and associated factors during the first trimester of pregnancy [J]. Journal of Peking University (Health Sciences), 2023, 55(4): 600-605. |
| [4] | Fei SUN,Jian LIU,Si-qi LI,Yi-ping WEI,Wen-jie HU,Cui WANG. Profiles and differences of submucosal microbial in peri-implantitis and health implants: A cross-sectional study [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 30-37. |
| [5] | Ling-wei MENG,Xue LI,Sheng-han GAO,Yue LI,Rui-tao CAO,Yi ZHANG,Shao-xia PAN. Comparison of three methods for establishing rat peri-implantitis model [J]. Journal of Peking University (Health Sciences), 2023, 55(1): 22-29. |
| [6] | Fei SUN,Si-qi LI,Yi-ping WEI,Jin-sheng ZHONG,Cui WANG,Wen-jie HU. Efficacy of combined application of glycine powder air-polishing in non-surgical treatment of peri-implant diseases [J]. Journal of Peking University (Health Sciences), 2022, 54(1): 119-125. |
| [7] | WU Jun-hui,CHEN Hong-bo,WU Yi-qun,WU Yao,WANG Zi-jing,WU Tao,WANG Meng-ying,WANG Si-yue,WANG Xiao-wen,WANG Jia-ting,YU Huan,HU Yong-hua. Prevalence and risk factors of osteoarthritis in patients with type 2 diabetes in Beijing, China from 2015 to 2017 [J]. Journal of Peking University (Health Sciences), 2021, 53(3): 518-522. |
| [8] | Yan GENG,Zhi-bo SONG,Xiao-hui ZHANG,Xue-rong DENG,Yu WANG,Zhuo-li ZHANG. Depression and anxiety in patients with psoriatic arthritis: Prevalence and associated factors [J]. Journal of Peking University (Health Sciences), 2020, 52(6): 1048-1055. |
| [9] | Si-wei DENG,Ze-yi CHEN,Zhi-ke LIU,Jian WANG,Lin ZHUO,Shuang-qing GAO,Jia-kuo YU,Si-yan ZHAN. Epidemiological study of bone and joint injury based on urban medical insurance database [J]. Journal of Peking University (Health Sciences), 2020, 52(3): 527-534. |
| [10] | Lu XU,Lu CHEN,Dong-sheng FAN,Jing-nan FENG,Li-li LIU,Si-yan ZHAN,Sheng-feng WANG. Calculation of the prevalence of progressive muscular atrophy among adults in China based on urban medical insurance data from 15 provinces [J]. Journal of Peking University (Health Sciences), 2020, 52(3): 521-526. |
| [11] | Zhong ZHANG,Huan-xin MENG,Jie HAN,Li ZHANG,Dong SHI. Effect of vertical soft tissue thickness on clinical manifestation of peri-implant tissue in patients with periodontitis [J]. Journal of Peking University (Health Sciences), 2020, 52(2): 332-338. |
| [12] | Dong SHI,Jie CAO,Shi-ai DAI,Huan-xin MENG. Short-term outcome of regenerative surgery treating peri-implantitis [J]. Journal of Peking University(Health Sciences), 2020, 52(1): 58-63. |
| [13] | ZHANG Hai-dong, ZHANG Li, SHI Dong, HAN Jie, YAN Xia, XIE Ye-si, MENG Huan-xin. Clinical study of locking-taper implants in patients treated for periodontitis [J]. Journal of Peking University(Health Sciences), 2018, 50(2): 300-307. |
| [14] | SHI Hui-feng, ZHANG Jing-xu, ZHANG Rong, WANG Xiao-li. Prevalence of autism spectrum disorders in children aged 0-6 years in China: a meta-analysis [J]. Journal of Peking University(Health Sciences), 2017, 49(5): 798-806. |
| [15] | LI Heng, HUANG Yue-Qin, MA Ya-Ting, LIU Zhao-Rui. Descriptive epidemiological study on disabilities attributed to non-dementia organic mental disorder in China [J]. Journal of Peking University(Health Sciences), 2014, 46(2): 247-253. |
|
||