北京大学学报(医学版) ›› 2019, Vol. 51 ›› Issue (6): 1096-1102. doi: 10.19723/j.issn.1671-167X.2019.06.021
震颤分析用于早期帕金森病的诊断价值
- 北京大学第三医院神经内科,北京 100191
Diagnostic value of tremor analysis in identifying the early Parkinson’s syndrome
Xiao-xuan LIU,Shuo ZHANG,Na LIU,A-ping SUN,Ying-shuang ZHANG,Dong-sheng FAN( )
)
- Department of Neurology, Peking University Third Hospital, Beijing 100191, China
摘要:
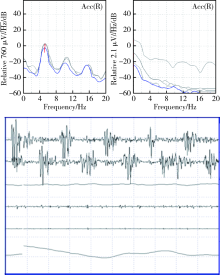
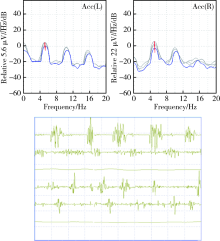
目的 研究震颤分析在以震颤为主的帕金森病患者中的早期识别作用。方法 本研究为前瞻性队列研究,入组对象为年龄>45岁、病程小于3年、于2014年1月至2015年12月在北京大学第三医院门诊或住院的单侧肢体震颤患者,记录流行病学资料、统一帕金森病评定量表-Ⅲ评分、非运动症状量表评分等。对所有患者进行震颤分析和中脑超声检查,按照震颤分析是否符合典型帕金森病的表现将患者分为三组:单侧震颤,震颤分析符合典型帕金森病表现,对侧无特异性表现(25例);单侧震颤,震颤分析双侧均符合典型帕金森病表现(15例);单侧震颤,震颤分析不符合典型帕金森病表现(30 例)。每半年或一年进行电话随访或面访,直到患者确定诊断。结果 三组患者的发病年龄、性别分布、汉密尔顿抑郁量表评分、Hoehn-Yahr(H-Y)分级差异无统计学意义(P>0.05)。统一帕金森病评定量表-Ⅲ评分的平均值三组分别为18.23、18.79和14.67,差异有统计学意义(P=0.001)。非运动症状量表评分的平均值三组分别为15.81、17.07和9.90,差异有统计学意义(P<0.001)。中脑超声检查的阳性率三组分别为48.0%、60.0%和26.67%,差异无统计学意义(P=0.702)。经过3年的随访,本组70例患者中有35例(50%)符合2015年国际帕金森病和运动障碍协会的帕金森病诊断标准,19例(27.1%)为特发性震颤,7例(10%)为帕金森叠加综合征。在进行帕金森病的早期诊断方面,震颤分析灵敏度为82.8%,特异度为68.6%,中脑超声灵敏度为65.7%,特异度为62.9%,两种检查方法具有一致性(Kappa=0.568)和差异性(P=0.031)。结论 震颤分析可以较为敏感和优越地识别以震颤为主要表现的早期帕金森病患者,但同时应注意结合患者的非运动症状和中脑超声检查。
中图分类号:
- R742.5
| [1] | Thenganatt MA, Jankovic J . Parkinson disease subtypes[J]. JAMA Neurol, 2014,71(4):499-504. |
| [2] | 中华医学会神经病学分会帕金森病及运动障碍学组. 中国帕金森病的诊断标准(2016 年)[J]. 中华神经科杂志, 2016,49(4):268-271. |
| [3] | Postuma RB, Berg D, Stern M , et al. MDS clinical diagnostic criteria for Parkinson’s disease[J]. Mov Disord, 2015,30(12):1591-1601. |
| [4] | Arshad AR, Sulaiman SA, Saperi AA , et al. MicroRNAs and target genes as biomarkers for the diagnosis of early onset of Parkinson disease [J/OL]. Front Mol Neurosci , 2017, 10: 352. (2017-10-31). doi: 10.3389/fnmol.2017.00352. |
| [5] | Marras C, Chaudhuri KR . Nonmotor features of Parkinson’s disease subtypes[J]. Mov Disord, 2016,31(8):1095-1102. |
| [6] | Hess CW, Pullman SL. Tremor: clinical phenomenology and assessment techniques [J/OL]. Tremor Other Hyperkinet Mov (N Y), ( 2012 -06-28). doi: 10.7916/D8WM1C41. |
| [7] | Buijink AW, Contarino MF, Koelman JH , et al. How to tackle tremor-systematic review of the literature and diagnostic work-up [J/OL]. Front Neurol, 2012, 3: 146. ( 2012-10-23). doi: 10.3389/fneur.2012.00146. |
| [8] | 杨硕, 潘华, 简凡 , 等. 帕金森病与多系统萎缩P型震颤峰频率、功率及谐波研究[J]. 中华神经科杂志, 2017,50(9):650-654. |
| [9] | Berg D, Roggendoff W, Schroder U , et al. Echogenicity of the substantia nigra: association with increased iron content and mar-ker for susceptibility to nigrostriatal injury[J]. Arch Neurol, 2002,59(6):999-1005. |
| [10] | Schrag A, Horsfall L, Walters K , et al. Prediagnostic presentations of Parkinson’s disease in primary care: a case-control study[J]. Lancet Neurol, 2015,14(1):57-64. |
| [11] | Lawton M, Ben-Shlomo Y, May MT , et al. Developing and validating Parkinson’s disease subtypes and their motor and cognitive progression[J]. J Neurol Neurosurg Psychiatry, 2018,89(12):1279-1287. |
| [12] | Rahimi F, Bee C, Wang D , et al. Subgroup analysis of PD tremor with loading: action tremor as a combination of classical rest and physiological tremor[J]. Clin Biomech (Bristol, Avon), 2015,30(2):114-120. |
| [13] | Abdullah R, Basak I, Patil KS , et al. Parkinson’s disease and age: The obvious but largely unexplored link[J]. Exp Gerontol, 2015,68:33-38. |
| [14] | 冯涛, 陈李 . 早发型帕金森病及其基因研究进展[J]. 中华神经科杂志, 2015,48(8):729-731. |
| [15] | Duval C, Daneault JF, Hutchison WD , et al. A brain network model explaining tremor in Parkinson’s disease[J]. Neurobiol Dis, 2016,85:49-59. |
| [16] | Levin J, Kurz A, Arzberger T , et al. The differential diagnosis and treatment of atypical Parkinsonism[J]. Dtsch Arztebl Int, 2016,113(5):61-69. |
| [17] | Becker G, Seufert J, Bogdahn U , et al. Degeneration of substantia nigra in chronic Parkinson’s disease visualized by transcranial color-coded real-time sonography[J]. Neurology, 1995,45(1):182-184. |
| [18] | Gaenslen A, Unmuth B, Godau J , et al. The specificity and sensitivity of transcranial ultrasound in the differential diagnosis of Parkinson’s disease: a prospective blinded study[J]. Lancet Neurol, 2008,7(5):417-424. |
| [19] | Shafieesabet A, Fereshtehnejad SM, Shafieesabet A , et al. Hyperechogenicity of substantia nigra for differential diagnosis of Parkinson’s disease: A meta-analysis[J]. Parkinsonism Relat Disord, 2017,42:1-11. |
| [20] | Li DH, He YC, Liu J, et al. Diagnostic accuracy of transcranial sonography of the substantia nigra in parkinson’s disease: A systematic review and meta-analysis [J/OL]. Sci Rep, 2016, 6: 20863. ( 2016-02-16). doi: 10.1038/srep20863. |
| [21] | 王宏利, 樊东升, 刘娜 , 等. 肌萎缩侧索硬化患者的中脑超声临床研究[J]. 中华神经科杂志, 2016,49(9):678-681. |
| [1] | 权会会,徐卫星,祁宇泽,李清如,周辉,黄婧. 模拟肽Gap27抑制缝隙连接蛋白43在帕金森病小鼠模型中的作用[J]. 北京大学学报(医学版), 2022, 54(3): 421-426. |
| [2] | 刘梅歌,方朴,王严,丛璐,范洋溢,袁远,徐燕,张俊,洪道俊. 远端型遗传性运动神经病8例的临床、病理及遗传学特点[J]. 北京大学学报(医学版), 2021, 53(5): 957-963. |
| [3] | 祁宇泽,权会会,徐卫星,李清如,周辉. 苯并[a]芘对脑内多巴胺能神经元和α-突触核蛋白的影响及其机制[J]. 北京大学学报(医学版), 2020, 52(3): 438-443. |
| [4] | 王晶,陈俊鹏,王洋,许向亮,郭传瑸. 数字化下颌运动记录及咀嚼肌肌电图在下颌骨肿瘤患者口颌功能评价中的应用[J]. 北京大学学报(医学版), 2019, 51(3): 571-578. |
| [5] | 韩济生. 疼痛、药物成瘾和神经退行性疾病最新研究进展[J]. 北京大学学报(医学版), 2009, 41(3): 249-254. |
| [6] | 高红, 王建军, 张蔚, 蒋玉辉, 牛东滨, 王晓民. 重组胶质细胞源性神经营养因子腺病毒保护小鼠中脑多巴胺能神经元[J]. 北京大学学报(医学版), 2003, 35(3): 256-260. |
| [7] | 何其华, 周慧芳, 薛冰, 牛东滨, 王晓民. 雷公藤单体T10对谷氨酸所致PC12细胞损伤的保护作用及机制研究[J]. 北京大学学报(医学版), 2003, 35(3): 252-255. |
| [8] | 李凌松, 路艳艳. 神经干细胞及帕金森病的细胞治疗[J]. 北京大学学报(医学版), 2002, 34(5): 499-505. |
|
||