北京大学学报(医学版) ›› 2019, Vol. 51 ›› Issue (6): 1091-1095. doi: 10.19723/j.issn.1671-167X.2019.06.020
原发性纵隔卵黄囊瘤7例
马义祥1,刘敬伟1,齐康1,张继新2,林钢1,刘海波1,商学谦1,李简1,△( )
)
- 1. 北京大学第一医院 胸外科,北京 100034
2. 北京大学第一医院 病理科,北京 100034
Diagnosis and treatment of seven primary mediastinal yolk sac tumors
Yi-xiang MA1,Jing-wei LIU1,Kang QI1,Ji-xin ZHANG2,Gang LIN1,Hai-bo LIU1,Xue-qian SHANG1,Jian LI1,△( )
)
- 1. Department of Thoracic Surgery, Peking University First Hospital, Beijing 100034, China
2. Department of Pathology, Peking University First Hospital, Beijing 100034, China
摘要:
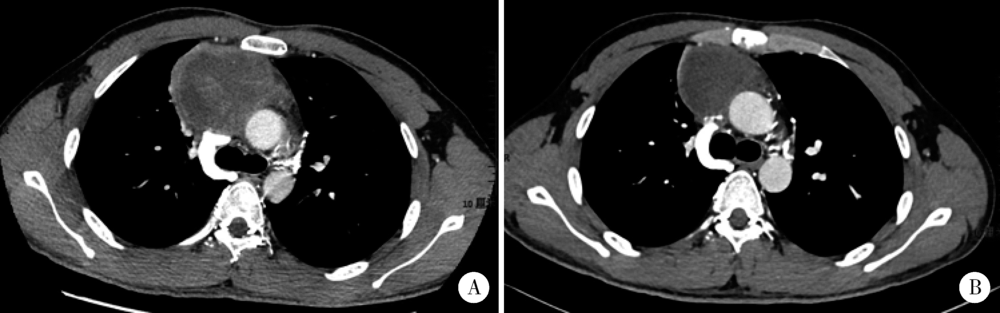
目的 总结原发性纵隔卵黄囊瘤诊治经验。方法 选择北京大学第一医院胸外科2014年8月至2018年8月收治的7例原发性纵隔卵黄囊瘤患者临床及病理资料,进行回顾性分析。结果 7例患者胸部CT显示前纵隔肿物,血清甲胎蛋白(alphafetoprotein, AFP) 水平均明显升高。5例术前接受穿刺活检,诊断为卵黄囊瘤,接受含铂双药或三药方案化疗后行肿瘤扩大切除,其中4例术后继续进行化疗;另2例患者术前未接受穿刺活检,术后病理诊断为卵黄囊瘤,并接受含铂方案化疗。7例患者均顺利完成手术,6例达到R0切除,1例为R1切除。2例出现术后并发症(1例肺炎和1例肺不张)。3例术后1年内出现肺转移,4例未出现复发和转移。结论 原发性纵隔卵黄囊瘤临床罕见,恶性程度较高,经合理诊治后部分患者可获得长期生存。
中图分类号:
- R736
| [1] | Isaacs H . Perinatal (fetal and neonatal) germ cell tumors[J]. J Pediatr Surg, 2004,39(7):1003-1013. |
| [2] | Akasbi Y, Najib R, Arifi S , et al. Complete histologic response to chemotherapy in a patient with a mediastinal yolk sac tumor: a case report[J]. BMC Res Notes, 2014,7(1):803. |
| [3] | 采丽, 章如松, 时姗姗 , 等. 纵隔原发生殖细胞肿瘤56例临床病理分析[J]. 临床与实验病理学杂志, 2018,34(2):162-166. |
| [4] | Rodney AJ, Tannir NM, Siefker-Radtke AO , et al. Survival outcomes for men with mediastinal germ-cell tumors: the University of Texas M. D. Anderson Cancer Center experience[J]. Urol Oncol, 2012,30(6):879-885. |
| [5] | Soriano PK, Iqbal MF, Siddiqui OM , et al. Non-seminomatous germ cell tumor presenting with superior vena cava syndrome[J]. Am J Case Rep, 2017,18:902-907. |
| [6] | Chaudhry IU, Rahhal M, Khurshid I , et al. Radical surgical resection for giant primary mediastinal endodermal sinus tumor with pulmonary metastasis after chemotherapy: can be curative [J/OL]. BMJ Case Rep ( 2014 -06-17)[2019-05-01]. |
| [7] | Saxman S, Nichols CR, Williams SD , et al. Mediastinal yolk sac tumor. The Indiana University experience, 1976 to 1988[J]. J Thorac Cardiovasc Surg, 1991,102(6):913-916. |
| [8] | Kurman RJ . Blaustein’s pathology of the female genital tract[M]. 5th ed.New York: Springer-Verlag, 2002: 967-1033. |
| [9] | César AM, Suster S . Hepatoid yolk sac tumors of the mediastinum: a clinicopathologic and immunohistochemical study of four cases[J]. Am J Surg Pathol, 1997,21(10):1210-1214. |
| [10] | Gao Y, Jiang J, Liu Q . Extragonadal malignant germ cell tumors: a clinicopathological and immunohistochemical analysis of 48 cases at a single Chinese institution.[J]. Int J Clin Exp Pathol, 2015,8(5):5650-5657. |
| [11] | Wang F, Liu A, Peng Y , et al. Diagnostic utility of SALL4 in extragonadal yolk sac tumors: an immunohistochemical study of 59 cases with comparison to placental-like alkaline phosphatase, alpha-fetoprotein, and glypican-3[J]. Am J Surg Pathol, 2009,33(10):1529-1539. |
| [12] | 于秀杰, 申彦 . SALL4与生殖细胞肿瘤[J]. 天津医科大学学报, 2017,23(3):283-285. |
| [13] | Shojaei H, Hong H, Redline RW . High-level expression of divergent endodermal lineage markers in gonadal and extra-gonadal yolk sac tumors[J]. Mod Pathol, 2016,29(10):1278-1288 |
| [14] | Tinica G, Butcovan D, Cimpeanu C , et al. A mediastinal germ cell tumor of yolk sac type: case report[J]. Chirurgia, 2010,105(6):831. |
| [15] | Nakamura Y, Matsumura A, Katsura H , et al. Cisplatin-based chemotherapy followed by surgery for malignant nonseminomatous germ cell tumor of mediastinum: one institution's experience[J]. Gen Thorac Cardiovasc Surg, 2009,57(7):363-368. |
| [16] | 佘祥冬 . 卵巢卵黄囊瘤诊疗进展[J]. 国际妇产科学杂志, 2017,44(2):137-141. |
| [17] | Sudour-Bonnange H, Faure-Conter C, Martelli H , et al. Primary mediastinal and retroperitoneal malignant germ cell tumors in children and adolescents: results of the TGM95 trial, a study of the French Society of Pediatric Oncology (Société Francaise des Can-cers de l’Enfant)[J]. Pediatric Blood Cancer, 2017,64(9):e26294. |
| [18] | Walsh GL, Taylor GD, Nesbitt JC , et al. Intensive chemotherapy and radical resections for primary nonseminomatous mediastinal germ cell tumors[J]. Ann Thorac Surg, 2000,69(2):337-343. |
| [19] | Kesler KA, Rieger KM, Ganjoo KN , et al. Primary mediastinal nonseminomatous germ cell tumors: the influence of postchemotherapy pathology on long-term survival after surgery[J]. J Thorac Cardiovasc Surg, 1999,118(4):692-700. |
| [1] | 刘京,陆爱东,左英熹,吴珺,黄志卓,贾月萍,丁明明,张乐萍,秦炯. 儿童急性淋巴细胞白血病合并癫痫发作75例临床特征和预后分析[J]. 北京大学学报(医学版), 2022, 54(5): 948-953. |
| [2] | 孙志伟,贾军,杨颖,刘传玲,肖艳洁,余靖,张晓东. 肠内营养支持治疗减轻晚期食管癌患者化疗不良反应[J]. 北京大学学报(医学版), 2020, 52(2): 261-268. |
| [3] | 耿良,吕静,范敬. 肺瘤平膏联合环磷酰胺化疗对肺癌的抑瘤作用和酸性微环境的影响[J]. 北京大学学报(医学版), 2020, 52(2): 247-253. |
| [4] | 陈杨,王艳荣,石燕,戴广海. 晚期结直肠癌患者一线应用FOLFOX方案化疗引起中性粒细胞减少的预后价值[J]. 北京大学学报(医学版), 2017, 49(4): 669-674. |
| [5] | 瓦斯里江·瓦哈甫, 何志嵩, 周利群. 成人肾母细胞瘤一例[J]. 北京大学学报(医学版), 2008, 40(3): 334-338. |
| [6] | Guo-hui LU. 治疗相关的急性髓系白血病的临床细胞遗传学诊断[J]. 北京大学学报(医学版), 2005, 37(1): 10-13. |
| [7] | 管宏, 赵慧云, 沈磊, 李五岭, 王建华, 王春荣, 徐福. 联合应用重组TPO和G-CSF对骨髓抑制性小鼠外周血小板及白细胞恢复的影响[J]. 北京大学学报(医学版), 2001, 33(2): 181-182. |
|
||