北京大学学报(医学版) ›› 2019, Vol. 51 ›› Issue (6): 1085-1090. doi: 10.19723/j.issn.1671-167X.2019.06.019
亚洲骨质疏松筛查工具在健康体检中的筛查准确性评价及适宜切点研究
- 1. 北京大学第三医院体检中心,北京 100191
2. 北京大学第三医院骨科,北京 1001901
3. 北京大学公共卫生学院流行病与卫生统计学系,北京 100191
4. 北京大学第三医院临床流行病学研究中心,北京 100191
Evaluation of screening accuracy on osteoporosis self-assessment tool for Asians and its cut-off value in healthy physical examination population
Peng WANG1,Hua WU1,Ying CHE1,Dong-wei FAN2,Jue LIU3,Li-yuan TAO4,△( )
)
- 1. Medical Examination Centre, Peking University Third Hospital, Beijing 100191, China
2. Department of Orthopedics, Peking University Third Hospital, Beijing 100191, China
3. Department of Epidemiology and Biostatistics, Peking University School of Public Health, Beijing 100191, China
4. Research Center of Clinical Epidemiology, Peking University Third Hospital, Beijing 100191, China
摘要:
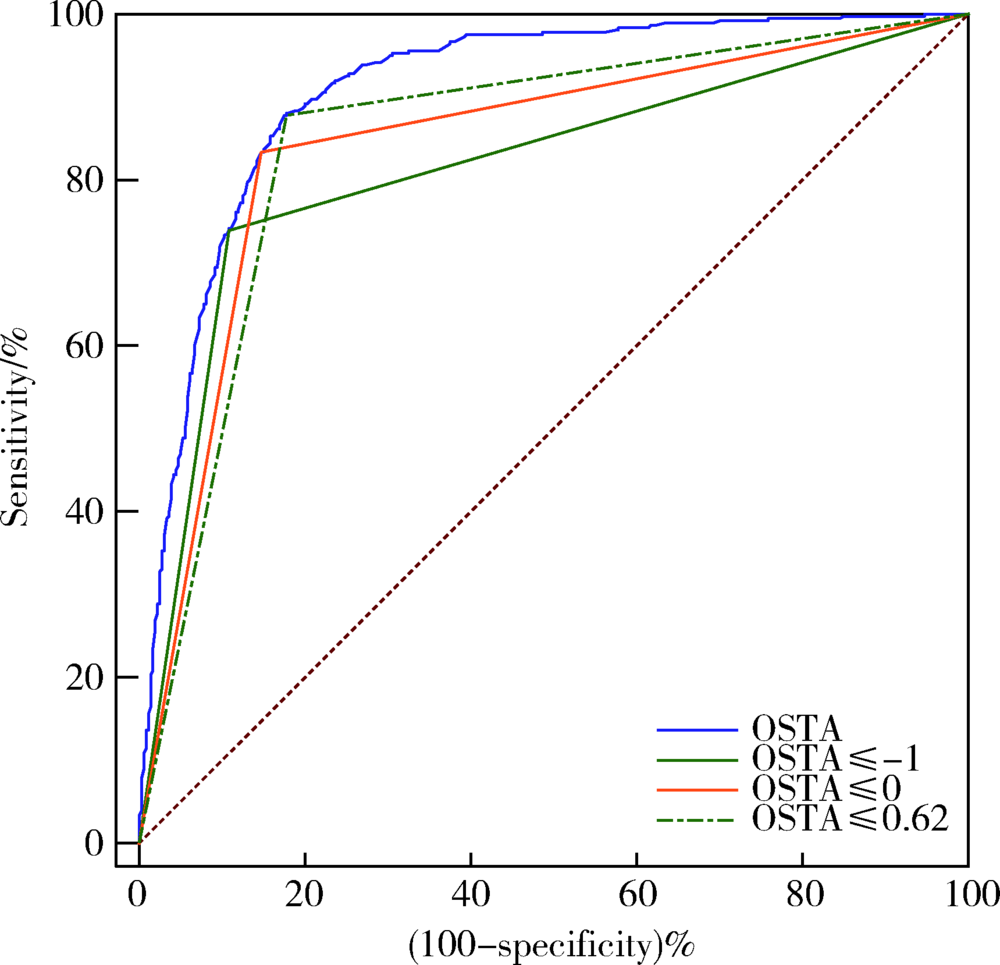
目的 探索亚洲骨质疏松筛查工具(osteoporosis self-assessment tool for Asians, OSTA)在中国健康体检人群中的筛查价值,探索适宜中国健康体检人群的最佳切点值。方法 选取2013—2016年在北京大学第三医院体检中心进行骨密度筛查的体检人群作为研究对象,定量超声骨密度检测(quantitative ultrasound, QUS)结果T值≤-2.5者定义为骨质疏松症患者。分析OSTA在不同切点时的灵敏度、特异度、似然比和曲线下面积(area under curve,AUC),比较不同切点时OSTA的筛查准确性,寻找适宜的切点值。结果 共纳入研究对象5 833名,平均年龄(48.3±17.5)岁,其中女性2 594人(占44.5%)。QUS检测结果显示骨质疏松患者403人(占总人群6.9%),女性患者343人(占女性人群13.22%)。在全年龄组人群中,OSTA国际常规切点值(≤-1)筛查骨质疏松的AUC为0.815(95%CI:0.804~0.825),女性人群筛查准确性(AUC=0.837,95%CI:0.823~0.851)优于男性人群(AUC=0.767,95%CI:0.752~0.781;P<0.05)。在全年龄组人群中以OSTA≤0为筛查切点值筛查骨质疏松的AUC为0.842(95%CI:0.832~0.851),准确性优于以-1为切点值(P<0.01),净重分类指数(net reclassification improvement,NRI)提高5.5%。40~65岁人群中,以OSTA≤0为筛查切点值时,筛查准确性较-1时提高明显(NRI=19.5%,P=0.003)。结论 OSTA筛查工具在健康体检人群中具有较好的骨质疏松筛查价值,且女性人群的筛查准确性优于男性,适度提高OSTA的筛查切点值能够在全年龄组人群和40~65岁年龄组人群中有更好的筛查获益。
中图分类号:
- R681
| [1] | Kanis JA, McCloskey E, Branco J, et al. Goal-directed treatment of osteoporosis in Europe[J]. Osteoporos Int, 2014,25(11):2533-2543. |
| [2] | Lorenc R, Gluszko P, Franek E , et al. Guidelines for the diagnosis and management of osteoporosis in Poland: Update 2017[J]. Endokrynol Pol, 2017,68(5):604-609. |
| [3] | Si L, Winzenberg TM, Jiang Q , et al. Projection of osteoporosis-related fractures and costs in China: 2010—2050[J]. Osteoporos Int, 2015,26(7):1929-1937. |
| [4] | Koh LK, Sedrine WB, Torralba TP , et al. A simple tool to identify Asian women at increased risk of osteoporosis[J]. Osteoporos Int, 2001,12(8):699-705. |
| [5] | Lydick E, Cook K, Turpin J , et al. Development and validation of a simple questionnaire to facilitate identification of women likely to have low bone density[J]. Am J Manag Care, 1998,4(1):37-48. |
| [6] | Cadarette SM, Jaglal SB, Kreiger N , et al. Development and validation of the osteoporosis risk assessment instrument to facilitate selection of women for bone densitometry[J]. CMAJ, 2000,162(9):1289-1294. |
| [7] | Sedrine WB, Chevallier T, Zegels B , et al. Development and assessment of the osteoporosis index of risk (OSIRIS) to facilitate selection of women for bone densitometry[J]. Gynecol Endocrinol, 2002,16(3):245-250. |
| [8] | Salaffi F, Silveri F, Stancati A , et al. Development and validation of the osteoporosis prescreening risk assessment (OPERA) tool to facilitate identification of women likely to have low bone density[J]. Clin Rheumatol, 2005,24(3):203-211. |
| [9] | Crandall CJ . Risk assessment tools for osteoporosis screening in postmenopausal women: a systematic review[J]. Curr Osteoporos Rep, 2015,13(5):287-301. |
| [10] | 中华医学会骨质疏松和骨矿盐疾病分会. 原发性骨质疏松症诊疗指南(2017)[J]. 中华骨质疏松和骨矿盐疾病杂志, 2017,10(5):413-443. |
| [11] | 《中国老年骨质疏松症诊疗指南(2018)》工作组, 中国老年学和老年医学学会骨质疏松分会, 马远征 , 等. 中国老年骨质疏松症诊疗指南(2018)[J]. 中国骨质疏松杂志, 2018,24(12):1541-1567. |
| [12] | Chang SF, Yang RS . Determining the cut-off point of osteoporosis based on the osteoporosis self-assessment tool, body mass index and weight in Taiwanese young adult women[J]. J Clin Nurs, 2014,23(17-18):2628-2636. |
| [13] | Chang AJ, Ying Q, Chen XN , et al. Evaluation of three risk assessment tools in discriminating fracture status among Chinese patients undergoing hemodialysis[J]. Osteoporosis Int, 2016,27(12):3599-3606. |
| [14] | Oh SM, Nam B, Rhee Y , et al. Development and validation of osteoporosis risk-assessment model for Korean postmenopausal women[J]. J Bone Miner Metab, 2013,31(4):423-432. |
| [15] | Pencina MJ, D’Agostino RS, D’Agostino RJ, et al. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond[J]. Stat Med, 2008, 27(2): 157-172, 207-212. |
| [16] | Si L, Winzenberg TM, Chen M , et al. Screening for osteoporosis in Chinese post-menopausal women: a health economic modelling study[J]. Osteoporos Int, 2016,27(7):2259-2269. |
| [17] | Yang Y, Wang B, Fei Q , et al. Validation of an osteoporosis self-assessment tool to identify primary osteoporosis and new osteoporo-tic vertebral fractures in postmenopausal Chinese women in Beijing[J]. BMC Musculoskelet Disord, 2013,14:271. |
| [18] | Huang JY, Song WZ, Zeng HR , et al. Performance of the osteoporosis self-assessment tool for asians (OSTA) in screening osteoporosis among middle-aged and old women in the Chengdu region of China[J]. J Clin Densitom, 2015,18(4):539-545. |
| [19] | Li-Yu JT, Llamado LJ, Torralba TP . Validation of OSTA among Filipinos[J]. Osteoporos Int, 2005,16(12):1789-1793. |
| [20] | Muslim D, Mohd E, Sallehudin A , et al. Performance of osteoporosis self-assessment tool for asian (OSTA) for primary osteoporosis in post-menopausal Malay women[J]. Malays Orthop J, 2012,6(1):35-39. |
| [21] | Kung AW, Ho AY, Ross PD , et al. Development of a clinical assessment tool in identifying Asian men with low bone mineral density and comparison of its usefulness to quantitative bone ultrasound[J]. Osteoporos Int, 2005,16(7):849-855. |
| [22] | Oh SM, Song BM, Nam BH , et al. Development and validation of osteoporosis risk-assessment model for Korean men[J]. Yonsei Med J, 2016,57(1):187-196. |
| [23] | Liu M, Zhang Y, Cheng X , et al. The effect of age on the changes in bone mineral density and osteoporosis detection rates in Han Chinese men over the age of 50[J]. Aging Male, 2014,17(3):166-173. |
| [24] | Huang JY, Song WZ, Huang M . Effectiveness of osteoporosis self-assessment tool for Asians in screening for osteoporosis in healthy males over 40 years old in China[J]. J Clin Densitom, 2017,20(2):153-159. |
| [25] | Geater S, Leelawattana R, Geater A . Validation of the OSTA index for discriminating between high and low probability of femoral neck and lumbar spine osteoporosis among Thai postmenopausal women[J]. J Med Assoc Thai, 2004,87(11):1286-1292. |
| [26] | Chan SP, Teo CC, Ng SA , et al. Validation of various osteoporosis risk indices in elderly Chinese females in Singapore[J]. Osteoporos Int, 2006,17(8):1182-1188. |
| [27] | Moon JH, Kim LO, Kim HJ , et al. Evaluation of the predictive index for osteoporosis as a clinical tool to identify the risk of osteoporosis in Korean men by using the Korea National Health and Nutrition Examination Survey Data[J]. Korean J Fam Med, 2016,37(6):346-350. |
| [28] | Zha XY, Hu Y, Pang XN , et al. Diagnostic value of osteoporosis self-assessment tool for Asians (OSTA) and quantitative bone ultrasound (QUS) in detecting high-risk populations for osteoporosis among elderly Chinese men[J]. J Bone Miner Metab, 2015,33(2):230-238. |
| [1] | 曹瑞洁,姚中强,焦朋清,崔立刚. 不同分类标准对中国大动脉炎的诊断效能比较[J]. 北京大学学报(医学版), 2022, 54(6): 1128-1133. |
| [2] | 姚海红,唐素玫,王志敏,张霞,陈绪勇,高莉,刘婧,戴逸君,胡肇衡,张学武,栗占国. 初发系统性红斑狼疮患者骨密度及血清骨转化因子的研究[J]. 北京大学学报(医学版), 2018, 50(6): 998-1003. |
| [3] | 曹婕1,孟焕新. 锥形束CT用于评估牙槽骨骨缺损的情况和骨再生区域骨密度的变化[J]. 北京大学学报(医学版), 2018, 50(1): 110-116. |
| [4] | 徐筱,徐莉,江久汇,吴佳琪,李小彤,靖无迪. 锥形束CT评判安氏Ⅲ类错牙合上前牙骨开裂与骨开窗的准确性分析[J]. 北京大学学报(医学版), 2018, 50(1): 104-109. |
| [5] | 王昱,郝燕捷,邓雪蓉,李光韬,耿研,赵娟,周炜,张卓莉. 类风湿关节炎患者骨量改变危险因素分析及FRAX的应用价值[J]. 北京大学学报(医学版), 2015, 47(5): 781-786. |
| [6] | 王昱,耿研,邓雪蓉,张卓莉. 女性类风湿关节炎患者手腕骨密度检查与超声腕关节骨侵蚀及炎症评分的相关性[J]. 北京大学学报(医学版), 2015, 47(5): 774-780. |
| [7] | 魏攀, 卢松鹤, 付静雅, 闫志敏, 华红. 原发性干燥综合征2012年美国风湿病学会分类标准的临床验证[J]. 北京大学学报(医学版), 2014, 46(2): 306-310. |
| [8] | 王昱,周炜,郝燕捷,李光韬,邓雪蓉,赵娟,张卓莉. 跟骨定量超声在筛查结缔组织病患者合并骨质疏松中的应用[J]. 北京大学学报(医学版), 2013, 45(5): 766-769. |
| [9] | 程琳, 李杰, 刘淼, 王殊, 蒋宏传, 杨德启. 多中心前瞻性对比动态光学乳腺成像与乳腺钼靶对乳腺癌诊断的灵敏度、特异度和安全性研究[J]. 北京大学学报(医学版), 2011, 43(3): 467-471. |
| [10] | 马彦*, 乔建军, 刘伟, 李若瑜. 烟曲霉sho1基因对渗透压传导的作用和抗真菌药物敏感性的影响[J]. 北京大学学报(医学版), 2009, 41(2): 162-167. |
| [11] | 郑旭, 林久祥. 牙槽骨密度定量测量系统的建立及测量精确性、有效性的检验[J]. 北京大学学报(医学版), 2008, 40(4): 431-436. |
| [12] | 李建平, 梁金峰, 邱建星, 陈大方, 霍勇. 64层螺旋CT对稳定型心绞痛及急性冠状动脉综合征患者冠状动脉病变的诊断价值[J]. 北京大学学报(医学版), 2007, 39(6): 645-648. |
| [13] | 李斌斌, 于世凤. 锌离子对牙各矿化成份破骨细胞性吸收的体外调控[J]. 北京大学学报(医学版), 2006, 38(6): 644-647. |
| [14] | 李荣昌, 杨惠雯, 王夔. 低剂量长期饲喂La(NO3)3后La在大鼠骨中的蓄积及骨微结构的改变[J]. 北京大学学报(医学版), 2003, 35(6): 622-624. |
| [15] | 杨欣, 林守清, 白文佩, 余卫, 陈淑玲, 沈英, 郑淑蓉. 雌孕激素联合疗法对绝经后妇女骨密度和血脂的影响[J]. 北京大学学报(医学版), 2002, 34(3): 294-297. |
|
||